To analyse the causes of hyperprolactinaemia in patients with symptoms compatible with hyperprolactinaemia evaluated in a primary care setting.
Patients and methodsA retrospective study of all patients tested for serum prolactin levels between 2019 and 2020 in 20 primary care centres at the Hospital Ramón y Cajal in Madrid. Hyperprolactinaemia is defined as a serum prolactin>19.4ng/ml in men and >26.5ng/ml in women. Aetiology is grouped into physiological (pregnancy, lactation, inadequate venipuncture, macroprolactinaemia), pharmacological, pathological (hypothalamic and/or pituitary diseases, chronic renal failure, primary hypothyroidism), and idiopathic.
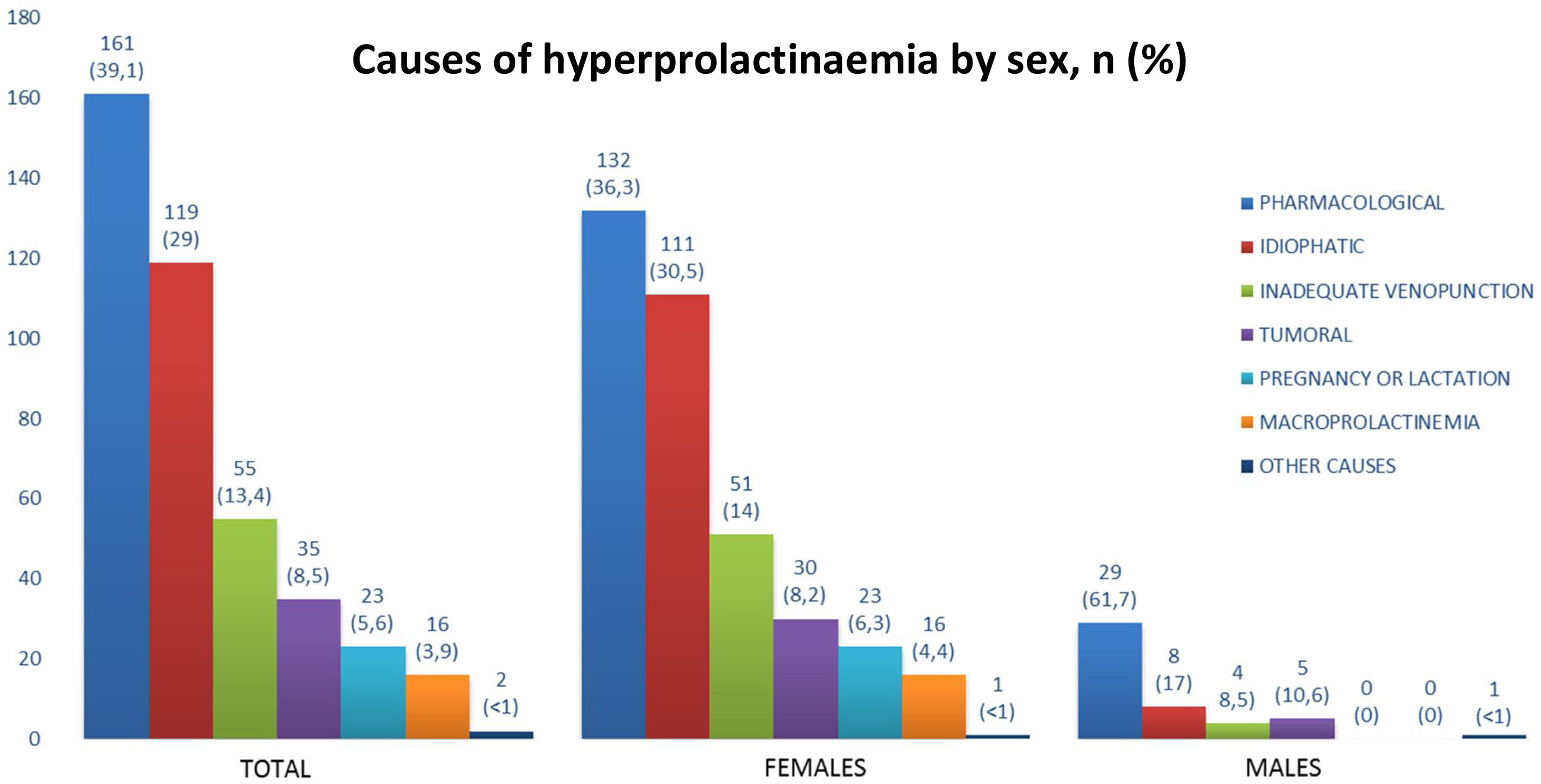
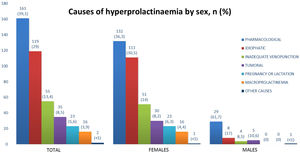
ResultsIn 1630 patients tested for serum prolactin, 30.7% (n=501) had hyperprolactinaemia. Of these 501 patients, 89.6% were females. 149 patients were referred to the Endocrinology Department and 164 to the Gynaecology Department. Aetiological diagnosis of hyperprolactinaemia was achieved in 411 out of 501 cases. The most frequent cause of hyperprolactinaemia was pharmacological, in 39.1%. The second more frequent cause was idiopathic (29%) and less common were inadequate venipuncture extraction (13.4%), tumour (8.5%) and macroprolactinaemia (3.9%). Patients with tumoural hyperprolactinaemia presented higher serum prolactin levels (87.0±80.19 vs 49.7±39.62ng/ml, P=0.010). In addition, symptoms, such as galactorrhoea (33.3% vs 16.5%, P=0.018), and headache (25.7% vs 13.3%, P=0.045), were more frequent than in patients of the other aetiological groups.
ConclusionHyperprolactinaemia is common among patients evaluated in a primary care setting with symptoms of hyperprolactinaemia, but more than 50% of cases are due to pharmacological treatments or improper sample extraction. It is necessary to establish referral protocols to specialised medicine to optimise healthcare resources and avoid unnecessary studies.
Analizar las causas de la hiperprolactinemia en pacientes con síntomas compatibles de hiperprolactinemia evaluados en el ámbito de Atención Primaria.
Pacientes y métodosEstudio retrospectivo de todos los pacientes a los que se les realizó la determinación de prolactina sérica entre 2019 y 2020 en 20 centros de Atención Primaria pertenecientes al área del Hospital Ramón y Cajal de Madrid. La hiperprolactinemia se ha definido como una prolactina sérica>19,4ng/ml en hombres y>26,5ng/ml en mujeres. La etiología se clasificó en fisiológica (embarazo, lactancia, extracción inadecuada, macroprolactinemia), farmacológica, patológica (enfermedades hipotalámicas y/o hipofisarias, insuficiencia renal crónica, hipotiroidismo primario) e idiopática.
ResultadosDe los 1.630 pacientes con solicitud de prolactina sérica, el 30,7% (n=501) tenía hiperprolactinemia. De estos 501 pacientes, el 89,6% eran mujeres. 149 pacientes fueron derivados al Servicio de Endocrinología y 164 al Servicio de Ginecología. El diagnóstico etiológico de hiperprolactinemia se logró en 411 de los 501 casos. La causa más frecuente de hiperprolactinemia fue la farmacológica, en un 39,1%. La segunda causa fue idiopática (29%) y menos frecuente la extracción inadecuada (13,4%), tumoral (8,5%) y presencia de macroprolactinemia (3,9%). Los pacientes con hiperprolactinemia tumoral presentaron niveles séricos de prolactina más elevados (87,0±80,19 vs. 49,7±39,62ng/ml, p=0,010). Además, los síntomas, como galactorrea (33,3 frente a 16,5%, p=0,018) y dolor de cabeza (25,7 frente a 13,3%, p=0,045), fueron más frecuentes que en los pacientes con hiperprolactinemia por otras causas.
ConclusiónLa hiperprolactinemia es común entre los pacientes evaluados en Atención Primaria con síntomas de hiperprolactinemia, pero más del 50% de los casos se deben a tratamientos farmacológicos o a una extracción inadecuada de la muestra. Es necesario establecer protocolos de derivación a medicina especializada para optimizar los recursos sanitarios y evitar estudios innecesarios.
Prolactin is a protein synthesised and released principally by lactotrophs in the anterior pituitary gland. Dopamine is established as the principal inhibitor of prolactin synthesis and secretion.1 Factors principally inducing prolactin synthesis and secretion are oestrogen, dopamine receptor antagonists, thyrotropin-releasing hormone and epidermal growth factor.2
Hyperprolactinaemia is characterised by increased production of prolactin, and different factors can lead to prolactin elevation, including pharmacological, physiological, and pathological causes. Therefore, a comprehensive study is necessary to ensure an adequate aetiological diagnosis in order to adapt the appropriate treatment and follow-up. Regarding its prevalence, different studies have reported variable figures depending on the population studied, ranging from 0.4% in asymptomatic patients to 9–17% in women with amenorrhoea and/or polycystic ovary syndrome.3–5 Furthermore, some authors estimate that the prevalence of hyperprolactinaemia has been increasing in recent years, probably as a consequence of the increase of the consumption of hyperprolactinaemic drugs,4 and due to the fact that serum prolactin is a parameter that is increasingly requested. Moreover, differences by sex have been reported, describing prevalence up to five times higher in women than in men.4
Differential diagnosis can be complex. There are causes which must be considered: physiological causes, such as pregnancy and lactation, pathological causes including hypothalamic and/or pituitary diseases, and pharmacological causes.2,6 The laboratory plays an important role in guiding the diagnosis of hyperprolactinaemia. It all starts with the measurement of isolated serum prolactin levels, always in the context of a non-traumatic venipuncture.2 In cases of discrete elevations of prolactin and/or prolactin levels discordant with the clinical picture, the measurement of this parameter should be repeated in two samples taken at 15–20-min intervals without repeated venipuncture (cannulated prolactin test). A common cause of hyperprolactinaemia is macroprolactinaemia.7,8 The most common cause of non-tumoural hyperprolactinaemia has been found to be pharmacological. Prolactin level varies according to pharmacological group,2,9–11 ranging from 25 to 100ng/ml, but metoclopramide, risperidone and phenothiazines can lead to 200ng/ml.2 Some authors reported that antipsychotic drug-induced hyperprolactinaemia has been estimated to occur in up to 70% of patients with schizophrenia.9 On the other hand, prolactinomas are the most frequent organic cause of prolactin excess and the most common type of hormone-secreting pituitary tumours.12
The aim of our study is to determine the causes of hyperprolactinaemia in the primary care setting and analyse whether there are clinical or hormonal differences depending on the cause of the hyperprolactinaemia. The final objective is to detect improvements in the care process, which could optimise visits to the specialist as well as the treatment itself, from the first determination made in these patients.
Material and methodsSample selectionThe Clinical Biochemistry Laboratory of Hospital Ramón y Cajal receives samples from 20 primary care centres, which represent an estimated population of 550,000 inhabitants. All serum prolactin samples from these were selected during the period 2019–2020 (n=1630 patients). The clinical history was reviewed in order to collect clinical and analytical data.
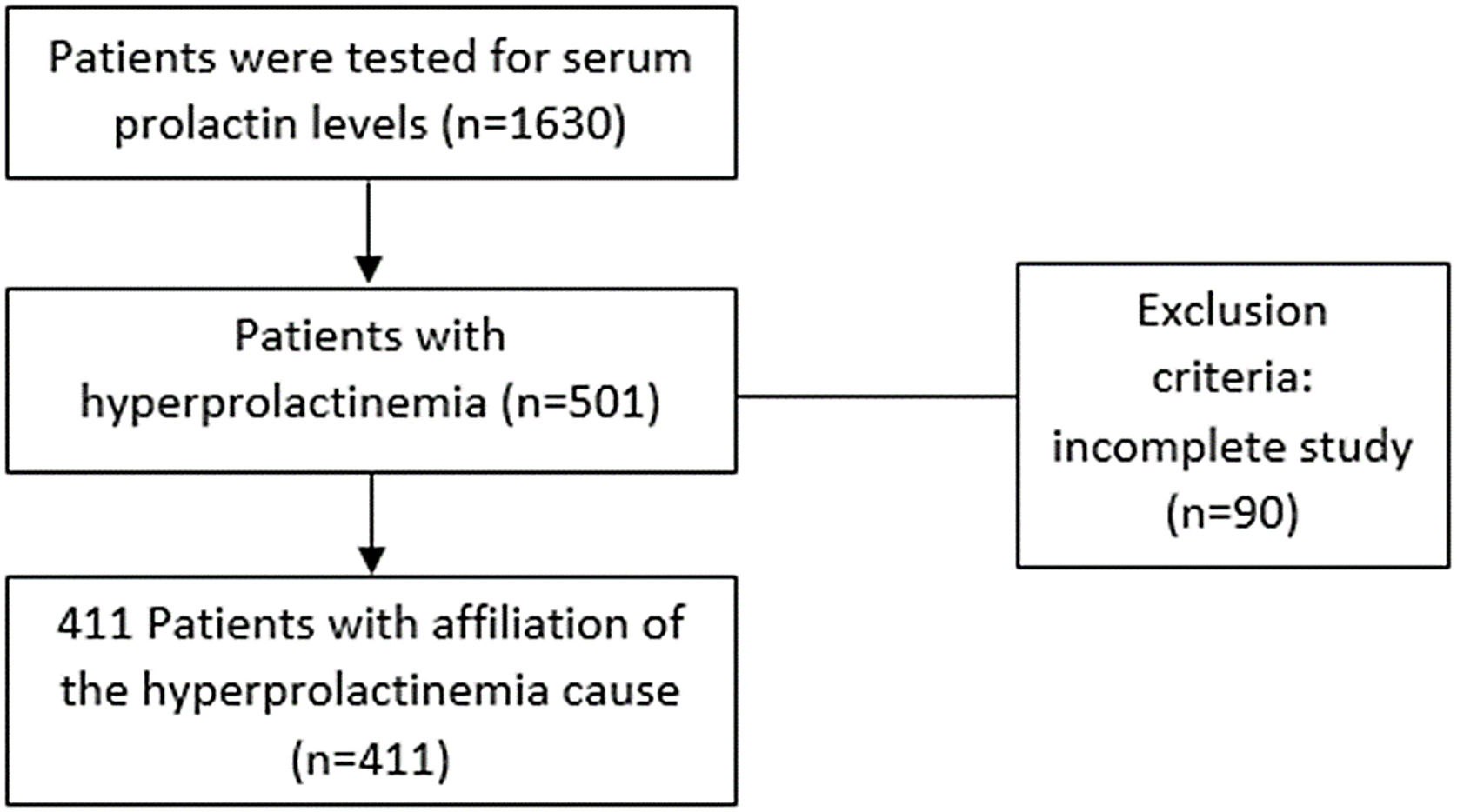
Only cases of hyperprolactinaemia, based on our laboratory ranges (n=501 patients), were selected. There were 90 patients who were excluded from the analysis of the causes of hyperprolactinaemia, 85 females and 5 males, because the final cause of hyperprolactinaemia was not available, as many of them had not yet completed the study or had not yet come for consultation (Fig. 1).
DefinitionsHyperprolactinaemia is defined as serum prolactin above 19.4ng/ml in men and above 26.5ng/ml in women, based on our laboratory range. Hyperprolactinaemia is classified into different groups according to aetiology: (i) physiological (pregnancy, lactation, venipuncture stress, macroprolactinaemia), (ii) pathological (organic by hypothalamic and/or pituitary diseases, chronic renal failure, and primary hypothyroidism), (iii) pharmacological and (iv) idiopathic.
Regarding the physiological causes, pregnancy or lactation were confirmed with data from the medical history. Venipuncture stress included patients who normalised serum prolactin levels at a subsequent extraction in the context of no prior intervention to that second withdrawal. The causes of their first elevation could be attributed to physiological situations such as exercise, anxiety, food intake, stress and venipuncture. Macroprolactinaemia was defined when the ratio Total serum prolactin-Free prolactin/Total prolactin ×100 exceeds 60% (recovery of 40%).13 In addition, the cause was defined as organic if it was of tumoural origin (prolactin-producing pituitary adenomas, non-functioning pituitary macroadenomas or other lesions with displacement of the pituitary stalk) and due to systemic diseases, such as overt primary hypothyroidism (with TSH levels above normal range and low FT4) and renal disease with a glomerular filtration rate<60ml/min/1.73m2. It was classified as pharmacological in those patients who were treated with drugs considered likely to cause an increase in prolactin levels, with normalisation of the serum prolactin after withdrawal or no evidence of another cause if withdrawal was not possible. The drugs considered to cause hyperprolactinaemia were anticonvulsants, antidepressants, antihistamines H2, dopamine receptor blockers and dopamine synthesis inhibitor, oestrogens (oral contraceptives), neuroleptics/antipsychotics2 and antihypertensives (verapamil and methyldopa).1 Idiopathic hyperprolactinaemia included patients who did not correspond to any of the previous groups but who maintained elevated prolactin levels.
Laboratory methodsTotal and post-polyethylene glycol (PEG) serum prolactin levels were determined by immunoassay (Abbott Architect, Chicago, IL, USA) calibrated against the WHO Third International Standard for prolactin (84/500). Total coefficient variation is 4.7% and 3.6% at mean prolactin concentrations of 7 and 35.8ng/ml, respectively; sensitivity is 0.6ng/ml.14
In order to determine the presence of macroprolactinaemia in the sample, it was precipitated with 25% PEG. Next, it was added to the same sample volume, vortexed and centrifuged and then, the prolactin in the supernatant was measured a second time. Free serum prolactin is defined as the concentration of prolactin in the supernatant after precipitation with PEG. PEG-precipitable prolactin (%) represents the amount of macroprolactin, which is calculated according to the formula: (Total serum prolactin-Free serum prolactin)/Total serum prolactin ×100.15
Data collection and statistical analysisStudy data were collected and managed using REDCap electronic data capture tools hosted at Hospital Ramón y Cajal Madrid.16,17 REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.
All statistical analyses were performed with STATA.15. The Shapiro–Wilk test was used to check the normality assumption and Levene's test was used to evaluate variance homogeneity. Categorical variables are expressed as percentages and absolute values. Quantitative variables are expressed as mean±standard deviation or median. For variables following normal distribution, we used Student's t test to compare the differences between the two groups. The chi-square test was used to compare the categorical variables between independent groups. In all cases, the statistical significance threshold was set as <0.05 and two-tailed analyses were performed.
ResultsPrevalence of hyperprolactinaemiaThe prevalence of hyperprolactinaemia in our cohort population was 30.7% (n=501), of which 89.6% of the patients were female. The mean age of the patients was 34.4±10.8 years (34.1±10.5 years old in females and 37.8±14.5 years old in males, P=0.303). The clinical manifestations reported by patients undergoing prolactin testing in primary care are shown in Table 1. The most frequent reason for prolactin testing in women was irregular menstruation and amenorrhoea; and gynaecomastia in men.
Clinical manifestations reported by patients with hyperprolactinaemia.
| Women (n=449) | Men (n=52) | ||
|---|---|---|---|
| Clinical manifestations | n (%) | Clinical manifestations | n (%) |
| Irregular menstruation | 127 (28.3%) | Gynaecomastia | 16 (30.8%) |
| Amenorrhoea | 94 (20.9%) | Headache | 9 (17.3%) |
| Galactorrhoea | 72 (16.0%) | Erectile dysfunction | 5 (9.6%) |
| Other symptoms | 58 (12.9%) | Decreased libido | 3 (5.8%) |
| Headache | 54 (12.0%) | Sterility | 2 (3.9%) |
| Sterility | 38 (8.5%) | Other symptoms | 2 (3.9%) |
| Decreased libido | 2 (0.5%) | ||
The group of other symptoms includes dysmenorrhoea, acne and metrorrhagia in women; and 1 case of anxiety and 1 case in which the reason for the request was unknown in men.
Of the 501 patients with hyperprolactinaemia, 194 were referred to the Endocrinology Department and 164 to the Gynaecology Department (62 of these patients had also been assessed by the endocrinologist). The most frequent cause of hyperprolactinaemia in patients referred to the Endocrinology Department was inadequate sample collection, while the most frequent cause in patients referred to the Gynaecology Department (without assessment by Endocrinology) was idiopathic hyperprolactinaemia (Table 2). Overall, the most frequent cause of referral was idiopathic (27.0%) and pharmacological (24.0%).
Cause of hyperprolactinaemia in patients who had been referred to a medical specialist.
| Cause of hyperprolactinaemia | Endocrinology assessment (n=196) | Gynaecology assessment (n=103) |
|---|---|---|
| Inadequate venipuncture | 53 (27.3%) | 4 (<1%) |
| Pharmacological | 39 (20.1%) | 32 (31.4%) |
| Idiopathic | 38 (19.6%) | 42 (41.1%) |
| Tumour | 28 (16.9%) | 0 (0%) |
| Macroprolactinaemia | 19 (10.0%) | 2 (<1%) |
| Pregnancy or lactation | 3 (<1%) | 5 (<1%) |
| Incomplete study | 14 (7.2%) | 17 (1.7%) |
| Other causes | 2 (<1%) | 1 (<1%) |
The aetiological study was completed in 411 patients. The most frequent cause was pharmacological in 39.1% (36.3% females and 61.7% males). In 8.5% of the cases the cause was tumour. In females (n=364), the most frequent cause was pharmacological, and the most frequent tumour was microprolactinoma (n=22), followed by non-functioning pituitary macroadenoma (n=7), and only one case of macroprolactinoma was detected. The other causes were infrequent (Fig. 2). In the male group (n=47), the main tumoural cause was non-functioning pituitary macroadenoma (n=4), with only one case of microprolactinoma and another case of macroprolactinoma. Patients with tumoural hyperprolactinaemia presented higher serum prolactin levels than patients in the other groups, as well as more frequently having galactorrhoea and headache (Table 3).
Differential characteristics between tumoural hyperprolactinaemia and other causes.
| Tumour (n=35) | Other causes (n=376) | P value | |
|---|---|---|---|
| Age (n=411) mean (standard deviation) | 37.3±12.34 | 34.1±10.94 | P=0.202 |
| Male sex (n=411) | 14.3% (n=5) | 11.2% (n=42) | P=0.580 |
| Amenorrhoea or oligomenorrhoea (n=364) | 26.7% (n=8) | 19.8% (n=66) | P=0.368 |
| Galactorrhoea (n=364) | 33.3% (n=11) | 16.5% (n=59) | P=0.018 |
| Erectile dysfunction (n=52) | 0% | 11.9% (n=5) | P=0.414 |
| Decreased libido (n=411) | 0% | 1.3% (n=5) | P=0.492 |
| Headache (n=411) | 25.7% (n=9) | 13.3% (n=50) | P=0.045 |
| Basal prolactin (first determination) ng/ml (n=411) | 87.0±80.19 | 49.7±39.62 | P=0.010 |
| Basal prolactin (second determination) ng/ml (n=201) | 56.4±52.31 | 30.3±28.47 | P=0.017 |
| Prolactin at 30minng/ml (n=102) | 55.7±41.87 | 22.2±16.33 | P=0.019 |
The main finding of this study is that 30% of the patients tested for serum prolactin levels due to compatible symptoms of hyperprolactinaemia had hyperprolactinaemia, the most frequent cause being pharmacological. Furthermore, it was found that patients with tumoural hyperprolactinaemia had higher prolactin levels, and symptoms such as galactorrhoea and headache were more frequent than in patients with hyperprolactinaemia of other origins.
The prevalence of hyperprolactinaemia in the cohort population, which includes patients with symptoms compatible with high prolactin levels, with a high pretest probability of hyperprolactinaemia, has been found to be 30%. Other studies have described lower figures, ranging from less than 1% in a healthy population to between 5% and 14% in women with secondary amenorrhoea.18 These data are difficult to compare with other studies, given that the clinical context in which this alteration has been studied is very different.3,4,6 Most authors agree that the prevalence is higher in patients who present symptoms of hyperprolactinaemia, such as amenorrhoea, galactorrhoea, or infertility.1,19 In this study, this prevalence has been calculated in a population in which this parameter is measured by clinical manifestations compatible with hyperprolactinaemia in a primary care setting. This fact may justify the differences between the reported prevalence data compared to other studies. In fact, as far as it is known, there is only one previous study that has also evaluated the prevalence of hyperprolactinaemia in a primary care setting in patients with a high pretest probability.6 In this previous study the prevalence of hyperprolactinaemia in patients tested for serum prolactin due to compatible symptoms was 42.3%, which is similar to that reported in our study.
Another important point in our series is that almost 60% of patients with hyperprolactinaemia were referred to the Endocrinology and/or Gynaecology Departments for evaluation. However, less than 10% of these cases actually presented with tumour as the cause. In order to optimise referrals to the Endocrinology and Gynaecology Departments, benign causes of hyperprolactinaemia, such as pregnancy, lactation, or incorrect sample collection, should be always excluded before considering requesting a medical specialist evaluation. Thus, it is highly important to review the medical history (i.e., review of pharmacological treatments likely to raise prolactin), perform a complete physical examination, evaluate clinical findings as well as certain laboratory parameters (i.e., prolactin levels, beta HCG, serum TSH levels, free t4 and serum creatinine).
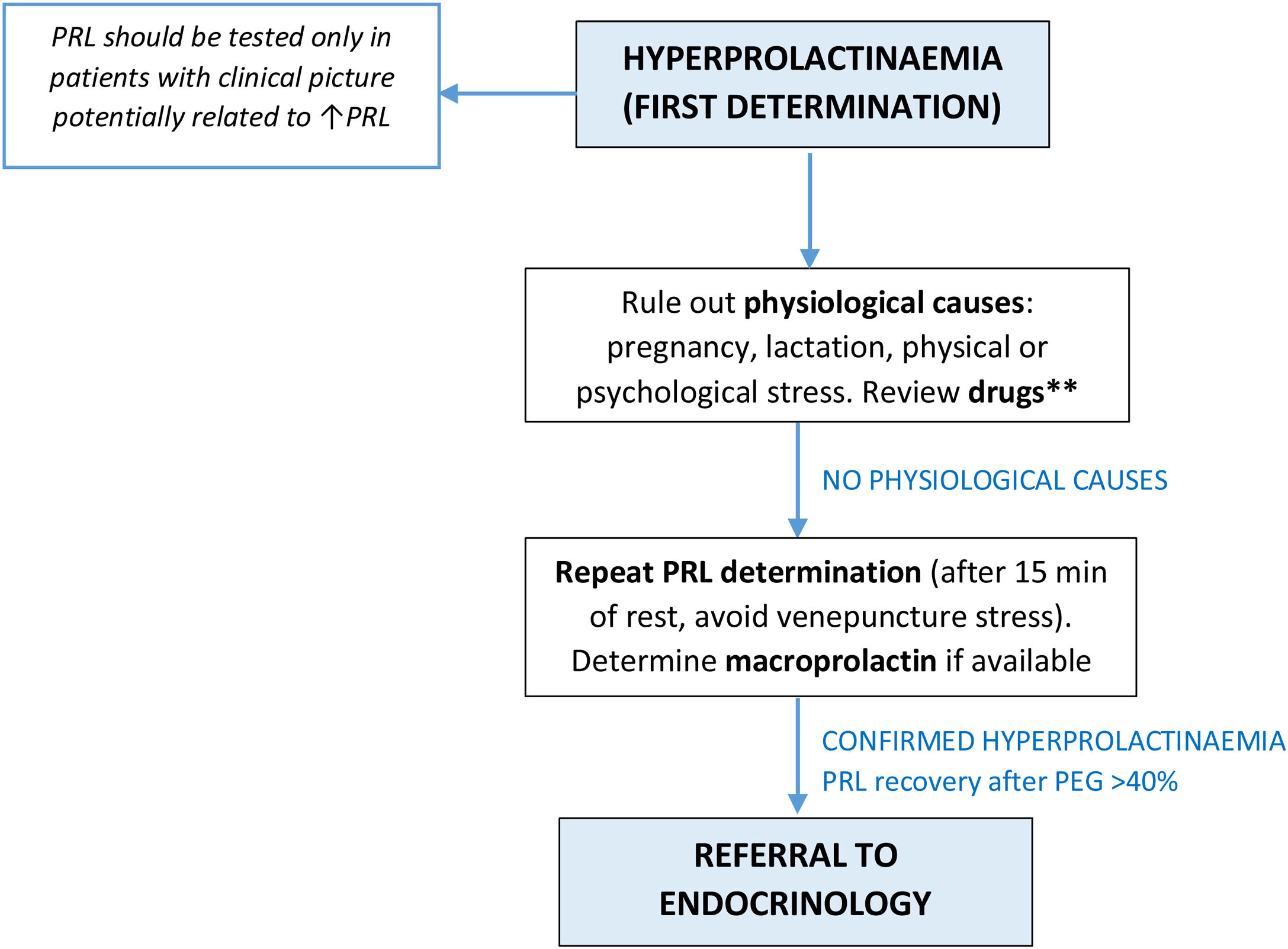
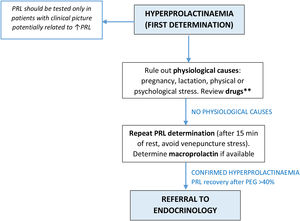
In cases where a physiological cause has been ruled out, the possibility of macroprolactin should be considered, especially in cases in which the patient is asymptomatic and has normal gonadotropins and sex steroids.2,20 The prevalence of macroprolactinaemia in this study is 4.4%, which does not coincide with that reported by other authors,7,15,21 probably because in this study PEG-precipitation has not been performed in all cases in which it should have been done. This finding supports the inclusion of PEG precipitation in the diagnostic algorithm of patients with hyperprolactinaemia to preclude unnecessary further investigations and treatment, especially in asymptomatic patients. Nevertheless, this determination is not available in most primary care centres. It is considered that if physicians in a primary care setting are properly instructed on the indications for testing macroprolactin, it could be a cost-effective measure and lead to avoiding unnecessary referrals to the specialty setting. An algorithm for a referral to a medical specialist is proposed based mainly on the clinical history (Fig. 3).
Proposal of algorithm for referral to medical specialist in Primary Care setting. **Primary Care doctors should also review drugs that could potentially be related to hyperprolactinaemia, consider withdrawal if possible and repeat determination. If PRL continues to be elevated after withdrawal, patients should be referred to Endocrinology. PRL: serum prolactin; PEG: polyethylene glycol.
The most frequent cause of hyperprolactinaemia in the cohort population is pharmacological (39.1%), which coincides with data reported in previous studies.4,11,22 Along this line, in the PROLEARS study, a population-based retrospective study of 1301 patients with hyperprolactinaemia, 45.9% were drug-induced.4 Nevertheless, the study by Malik et al. reported tumour as the most frequent cause in the primary care setting (37% in women and 27.6% in men).6 Therefore, in cases of pharmacological hyperprolactinaemia, the role of the physician is to exclude a co-existing hypothalamic-pituitary structural lesion. Also, some authors recommend that psychiatric management be adjusted and drugs substituted for others with a lesser effect on prolactin secretion.22. If the patient is taking a drug known, which causes hyperprolactinaemia, it is important to determine prolactin levels by withdrawing the drug for at least 72h, provided it is safe.23 This can be controversial especially in patients with severe psychiatric illness who are stable with their treatments, so in these cases it is advisable to do a Pituitary Magnetic Resonance Imaging (MRI).
Furthermore, in 13.4% of patients with hyperprolactinaemia, the cause is inadequate extraction due to stress or exercise and a second extraction or a two-stage extraction would be required to confirm this fact.
One of the most important findings in the current series is that in hyperprolactinaemia of tumoural origin it has been found that serum prolactin levels are higher than in other causes, both in basal prolactin and prolactin at 30min in those cases with serial prolactin sampling. Most authors agree that prolactin levels above 100–150ng/ml correspond to prolactinomas, and in cases of macroadenoma this value would be higher than 250ng/ml.2,24 Serum prolactin values between the upper limits of normal and 100ng/ml may be due to psychoactive drugs, oestrogen, or idiopathic causes, but can also be caused by a microprolactinoma. For this reason, although serum prolactin levels help guide diagnosis, they should be interpreted with caution, since there is overlap between serum prolactin levels in the different aetiologies.19,23–25 Moreover, in the cannulated prolactin test, hyperprolactinaemia of tumoural origin has higher basal prolactin and 30-minute levels than other causes. Therefore, authors suggest that a single prolactin value between 24 and 94ng/ml should be confirmed with a cannulated study.26
In addition, the symptoms presented by the patients studied may point to the diagnosis of a tumoural cause, which presents galactorrhoea and headache in a greater proportion than in those causes of non-tumoural origin. There is a study that did not find such differences in symptoms between the tumoural and non-tumoural groups,25 which may be due to differences in the populations studied, since in this study the group of patients with non-tumoural hyperprolactinaemia has been much larger. Furthermore, in other studies, the different clinical manifestations are not studied according to their cause, while they are distinguished between sex: female patients suffer amenorrhoea and irregular menstruation, and on the other hand, male patients show infertility and erectile dysfunction.6,25,27 Studies suggest that the prolactin level is commonly associated with different apparent clinical pictures.19
Many of the cases of hyperprolactinaemia finish up being classified as idiopathic (29%); it should be assumed that some patients classified in this group may have a small prolactinoma not visible on imaging tests.3 Prevalence of idiopathic hyperprolactinaemia in previous studies ranged from in 3.6–27.8% of all cases. This wide range is probably reflected in the differences found in the population studied and it may also be related to an underestimation of macroprolactin or an incomplete work-up of patients.4,27
The limitations of the study must be taken into consideration. They are mainly related to the retrospective nature of the study, and the possible bias induced by individual decisions in the consideration of referral to medical specialist and to test prolactin levels. Second, macroprolactinaemia may have been underdiagnosed in the study, as macroprolactin is not routinely screened in all patients. However, this study has several strengths and it is remarkable that all serum prolactin tested in a defined period of time has been included. In addition, this is the largest study assessing hyperprolactinaemia in Spain, and all patients were evaluated using the same prolactin assay.
ConclusionHyperprolactinaemia is common in patients evaluated in the primary care setting, but almost 50% are due to pharmacological treatments or improper sample extraction. It is necessary to establish protocols for referral to specialised medicine to optimise health resources and avoid unnecessary studies.
Protection of personsAll procedures performed on the participants of the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical approvalThe study was evaluated and approved by the ethics committee of the Hospital Ramón y Cajal (approval date: 27/04/2021, ACTA 412).
Data protectionThe authors declare that no patient data appear in this article.
Informed consentThe exemption of informed consent is requested, because it is a retrospective study.
Compliance with Ethical Standards.
Financial supportNo financial support has been received.
Conflict of interestThe authors have no conflict of interest.
We thank all the participants who have agreed to take part in this study. We wish to acknowledge the help of IRYCIS for the database and REDCap for data collection.