Hypoparathyroidism is the most common complication after total or completion thyroidectomy. It is defined as the presence of hypocalcemia accompanied by low or inappropriately normal parathyroid hormone (PTH) levels. Acute hypocalcemia is a potential lethal complication. Hypocalcemia treatment is based on endovenous or oral calcium supplements as well as oral calcitriol, depending on the severity of the symptoms. The risk of clinical hypocalcemia after bilateral thyroidectomy is considered very low if postoperative intact PTH decrease less than 80% with respect to preoperative levels. These patients could be discharged home without treatment, although this threshold may vary between institutions, and we recommend close surveillance in cases with increased risk (Graves disease, large goiters, reinterventions or evidence of parathyroid gland removal). Long-term treatment objectives are to control the symptoms and to keep serum calcium levels at the lower limit of the normal range, while preserving the calcium phosphate product and avoiding hypercalciuria.
El hipoparatiroidismo es la complicación más frecuente tras la tiroidectomía total. Se define por la presencia de hipocalcemia con unos niveles de hormona paratiroidea (PTH) bajos o inadecuadamente normales. La hipocalcemia aguda es una complicación potencialmente grave. Su tratamiento se basa, según la gravedad del cuadro, en la administración de calcio por vía oral o intravenosa, pudiendo requerir asimismo calcitriol oral. El riesgo de hypocalcemia sintomática tras una tiroidectomía es muy bajo si la PTH postoperatoria desciende menos del 80% respecto de la preoperatoria. Estos pacientes podrían ser dados de alta sin tratamiento, aunque los umbrales son variables entre laboratorios y recomendamos extremar la vigilancia en los casos de riesgo aumentado (enfermedad de Graves, grandes bocios, reintervenciones o constancia de la extirpación de alguna paratiroides). El tratamiento a largo plazo busca controlar los síntomas manteniendo la calcemia en el límite bajo de la normalidad, vigilando el producto calcio-fósforo y la aparición de hipercalciuria.
Post-thyroidectomy hypoparathyroidism (hypoPTH-PT) is the most common complication after one- or two-step total thyroidectomy. Although this disorder is a surgical complication, its immediate treatment often involves the Endocrinology Department, and long-term management is mainly supervised by the endocrinologist. For this reason, the Spanish Society of Otorhinolaryngology and Head and Neck Surgery (Sociedad Española de Otorrinolaringología y Cirugía de Cabeza y Cuello [SEORL CCC]) and the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]) have decided to prepare a joint consensus document addressing the most important aspects of this disease.
Post-thyroidectomy hypoparathyroidism is defined as the presence of hypocalcemia with inadequate PTH levels (manifestly low or inappropriately normal). The disorder may be transient or permanent when it persists beyond 6–12 months. The recovery of parathyroid function should be defined not only by the PTH levels, but also by the need or not for treatment, because up to 50% of all patients achieving normal PTH levels require treatment to prevent symptoms of hypocalcemia.
The consequence of deficient parathyroid function is the development of hypocalcemia, with no exact correlation between the appearance of biochemical hypocalcemia and the occurrence of associated symptoms. The treatment of acute hypocalcemia seeks to control symptoms and prevent serious complications, since the more severe presentations can prove life-threatening.
The nadir in calcium concentration and the appearance of symptoms may be delayed up to 48–72 h after surgery. For this reason, different methods have been developed to predict the occurrence of clinical manifestations of hypocalcemia after thyroidectomy. The measurement of PTH levels has been shown to be the most reliable method in this regard.
Based on the existing evidence, this consensus document advocates the following recommendations regarding hypoPTH-PT.
Preoperative recommendations- •
The prophylactic administration of calcium and vitamin D is not recommended, except in cases with preoperative evidence of deficiency.
- •
Surgery by an experienced surgical team is recommended.
- •
Closer monitoring is recommended in patients with Graves’ disease, especially if they have elevated alkaline phosphatase levels suggesting a risk of postoperative hungry bone syndrome.
- •
It is advisable to program closer postoperative monitoring in cases of greater surgical complexity, particularly second surgeries (reoperations), large goiters with intrathoracic spread and central compartment dissections.
- •
It is advisable for all parathyroid glands to be searched and identified during surgery.
- •
Careful identification and preservation of the vascular pedicle is recommended.
- •
Assessment of parathyroid gland status at the end of surgery is advised, with detailed recording of the findings.
- •
If not all the parathyroid glands have been identified, field revision of the surgical specimen and reimplantation of inadvertently removed glands is recommended.
- •
When thyroidectomy is performed, gland reimplantation is recommended only in the case of objective lesion or doubts regarding final gland functionality.
- •
In the case of bilateral central lymph node removal after thyroidectomy, resection and reimplantation of at least one parathyroid gland is recommended.
- •
The routine postoperative use of calcium and/or vitamin D supplements is not recommended in all patients undergoing total thyroidectomy.
- •
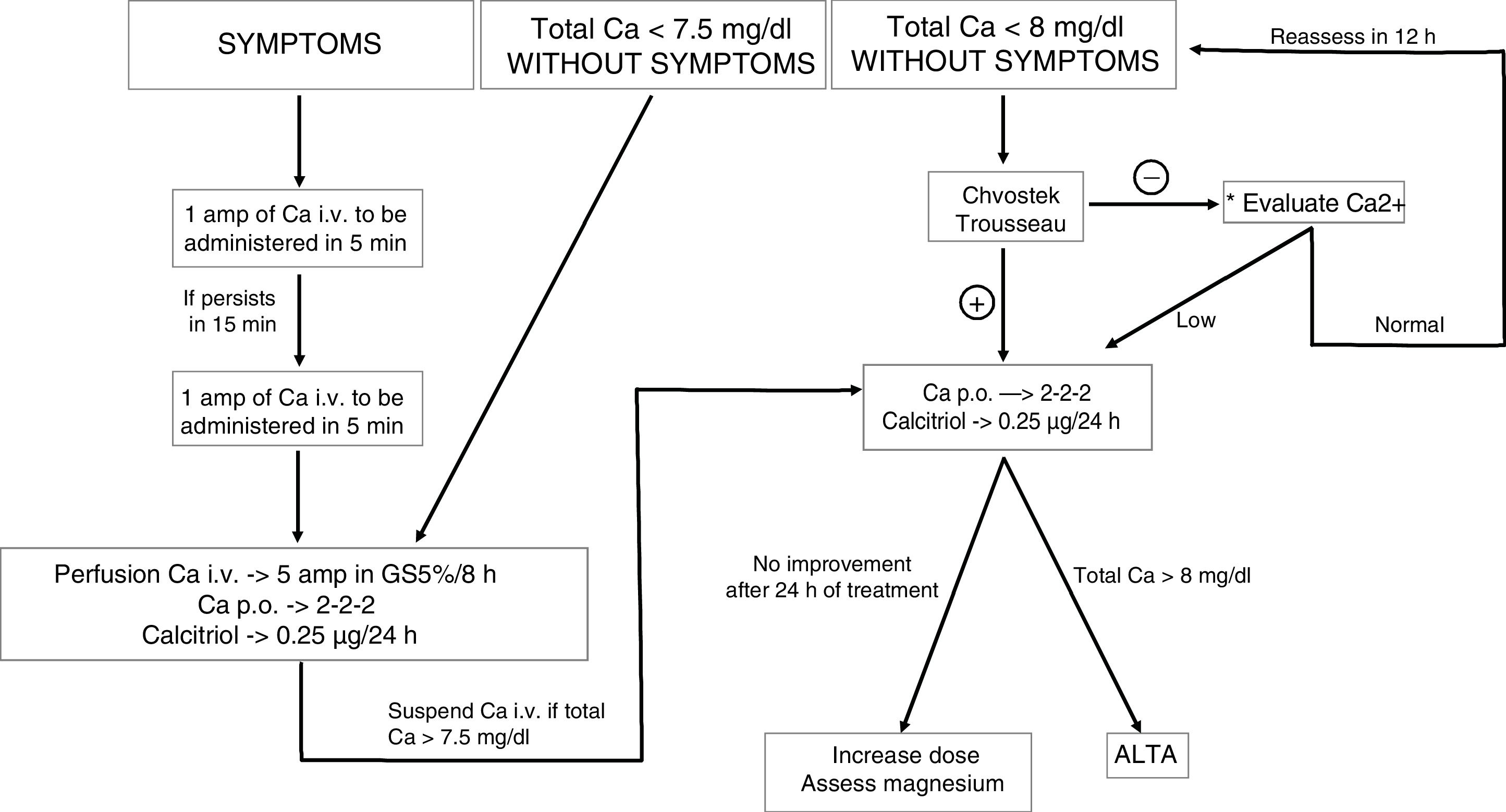
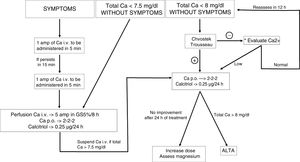
Manifest tetany or severe hypocalcemia should be treated with intravenous calcium. Moderate hypocalcemia can be treated with oral calcium formulations and calcitriol. Mild hypocalcemia or latent tetany may be treated with oral calcium supplements (Fig. 1).
- •
The use of PTH is recommended to determine the risk of developing clinical hypocalcemia in the first few hours after surgery. It is advisable to compare the postoperative and preoperative values, and to collect the sample at a time that allows its processing under optimum conditions.
- •
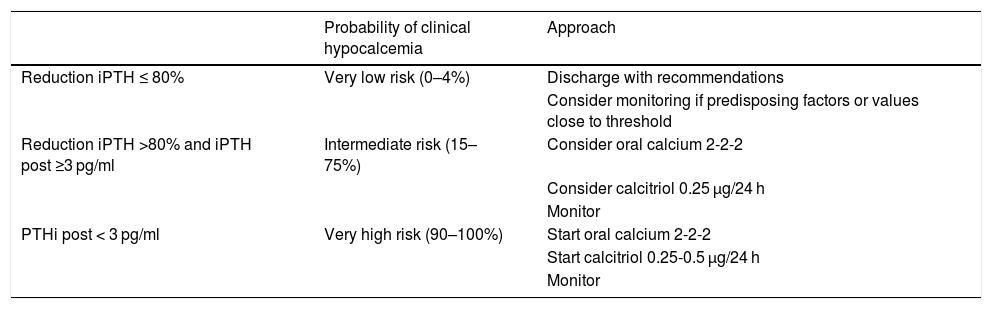
On an orientative basis, patients in whom preoperative PTH variation is less than 80% have a very low risk of clinical hypocalcemia, and can be discharged without supplements. However, it is advisable to adjust this threshold according to the characteristics of each center and each specific case, and to instruct the patients on what to do in the event of symptoms of hypocalcemia (Table 1).
Table 1.Stratification into risk groups for symptomatic hypoPTH-PT according to the cut-off points established in the studies of Hospital Universitario La Paz.
Probability of clinical hypocalcemia Approach Reduction iPTH ≤ 80% Very low risk (0–4%) Discharge with recommendations Consider monitoring if predisposing factors or values close to threshold Reduction iPTH >80% and iPTH post ≥3 pg/ml Intermediate risk (15–75%) Consider oral calcium 2-2-2 Consider calcitriol 0.25 μg/24 h Monitor PTHi post < 3 pg/ml Very high risk (90–100%) Start oral calcium 2-2-2 Start calcitriol 0.25-0.5 μg/24 h Monitor hypoPTH-PT: post-thyroidectomy hypoparathyroidism; monitor: monitoring of clinical manifestations and calcium levels every 12–24 h to assess dose adjustment of calcium and/or calcitriol.
Reduction iPTH = [(PTHpost-PTHpre)/PTHpre] × 100.
iPTH < 3 pg/ml implies undetectable intact PTH.
- •
Treatment comprising calcium supplements, with or without calcitriol, should be considered in patients with a high or indeterminate risk of clinical hypocalcemia (PTH decrease > 80% with respect to the preoperative level) (Table 1).
- •
Patients in whom a very high risk of symptomatic hypocalcemia has been determined (generally with undetectable postoperative PTH levels) should start oral calcium and calcitriol supplements in the first 24 h after surgery (Table 1).
- •
In cases where calcium supplements are started with or without calcitriol, the patients should be monitored, and the clinical signs and serum calcium levels should be monitored to adjust the dose. It is advisable for such monitoring to be performed on an in-hospital basis until calcemia has stabilized. Under adequate safety conditions, monitoring may be performed on an outpatient basis.
- •
Once stable calcium levels have been achieved, the dose should be maintained for 1–3 weeks before starting to gradually lower it.
- •
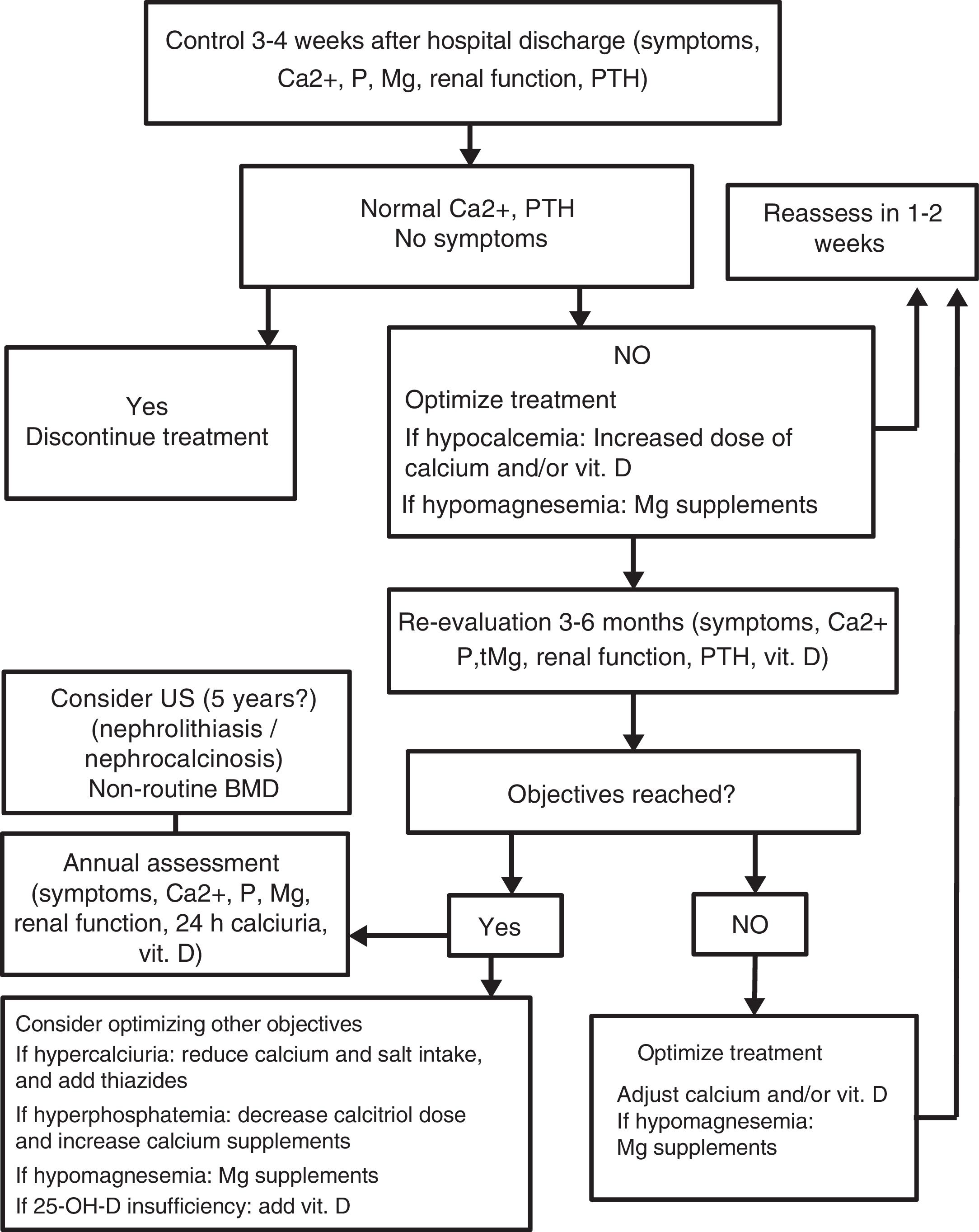
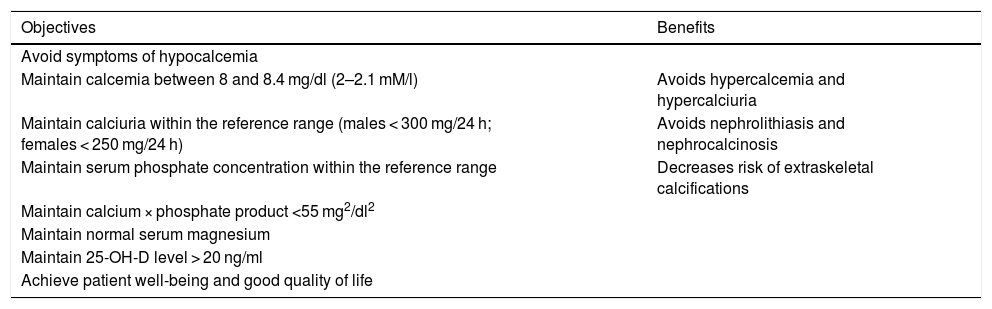
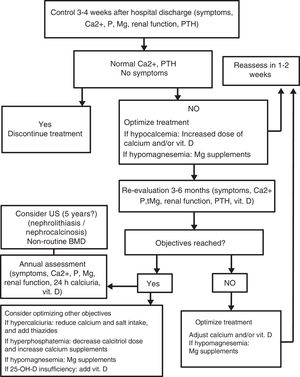
It is advisable to treat patients with permanent hypoparathyroidism using oral calcium salts and calcitriol to keep them free of symptoms and with serum calcium levels at or slightly below the lower limit of normal (Table 2 and Fig. 2).
Table 2.Objectives of the treatment of chronic hypoPTH-PT.
Objectives Benefits Avoid symptoms of hypocalcemia Maintain calcemia between 8 and 8.4 mg/dl (2–2.1 mM/l) Avoids hypercalcemia and hypercalciuria Maintain calciuria within the reference range (males < 300 mg/24 h; females < 250 mg/24 h) Avoids nephrolithiasis and nephrocalcinosis Maintain serum phosphate concentration within the reference range Decreases risk of extraskeletal calcifications Maintain calcium × phosphate product <55 mg2/dl2 Maintain normal serum magnesium Maintain 25-OH-D level > 20 ng/ml Achieve patient well-being and good quality of life hypoPTH-PT: post-thyroidectomy hypoparathyroidism.
- •
In the event of hypercalciuria, it is advisable to reduce calcium intake and restrict dietary salt intake. The addition of a thiazide-type diuretic to the treatment may prove necessary.
- •
In patients with hyperphosphatemia and/or a high calcium-phosphorus product, dietary intervention, an increase in the dose of calcium salts, and a reduction in the dose of calcitriol are recommended.
- •
In order to maintain adequate 25-OH-D levels, supplementing with 400–800 U of cholecalciferol a day is recommended in patients treated with calcitriol.
- •
In patients with hypomagnesemia, it is advisable to adopt measures to increase the magnesium levels.
- •
Once the therapeutic objectives have been reached, the clinical and biochemical parameters should be re-evaluated at least once a year.
- •
The routine use of rhPTH is not recommended.
Please cite this article as: Castro A, Oleaga A, Parente Arias P, Paja M, Gil Carcedo E, Álvarez Escolá C. Resumen ejecutivo del documento de consenso SEORL CCC-SEEN sobre hipoparatiroidismo postiroidectomía. Endocrinol Diabetes Nutr. 2019;66:459–463.