This study was promoted by Sociedad Castellano Manchega de Endocrinología, Nutrición y Diabetes to ascertain the characteristics of patients seen at the outpatient clinics of endocrinology and nutrition of the Castilla-La Mancha Health Authority and the case mix of diagnoses.
Patients and MethodsThis was a retrospective, cross-sectional study of the activity of the endocrinology and nutrition outpatient clinics of public hospitals of Castile-La Mancha during 2018. All visits made on 10% of the working days were analyzed. Data collected comprised patient age and sex, whether a first or subsequent had been made, and whether this was face-to-face or not, and up to five diagnoses per visit.
ResultsA total of 10,709 visits with a subsequent/first visit ratio of 3.4 were analyzed. Patient age was 52.1?±?18.2 years, and 67.1% were women. Type 2 diabetes mellitus, primary hypothyroidism, thyroid nodular disease, and obesity/overweight were the most common conditions recorded as first diagnosis, accounting for more than half of the total number of visits. Type 1 diabetes mellitus and thyroid cancer were the diagnoses in which the subsequent/first visit ratio was greater. Type 2 diabetes mellitus, obesity, and primary hypothyroidism accounted for almost half of the first visits.
ConclusionsA wide variety of conditions were seen, some of which are among the most prevalent in the general population, while others are not so prevalent, but are complex and difficult to manage by other specialties. Improved knowledge and analysis of the data should allow for the identification of opportunities for improvement and for the implementation of specific actions.
Estudio promovido por la Sociedad Castellano Manchega de Endocrinología, Nutrición y Diabetes para conocer las características de los pacientes atendidos en las consultas externas de Endocrinología y Nutrición del Servicio de Salud de Castilla-La Mancha y la casuística de la patología atendida en dichas consultas.
Material y MétodosEstudio transversal retrospectivo de la actividad en 2018 de las consultas externas de Endocrinología y Nutrición de los hospitales públicos de Castilla-La Mancha. Se analizaron todas las visitas del 10% de los días laborables. Se recogió edad y sexo del paciente, si la consulta era primera o sucesiva, presencial o no presencial y hasta cinco diagnósticos por visita.
ResultadosSe analizaron 10.709 visitas con una relación sucesivas/primeras 3,4. La edad de los pacientes fue 52,1?±?18,2 años con un 67,1% de mujeres. Diabetes mellitus tipo 2, hipotiroidismo primario, enfermedad nodular tiroidea y obesidad/sobrepeso fueron las patologías más frecuentemente registradas como primer diagnóstico, superando entre las cuatro la mitad del total de visitas. Diabetes mellitus tipo 1, y cáncer de tiroides fueron los diagnósticos en los que la relación sucesivas/primeras fue mayor. Diabetes mellitus tipo 2, obesidad e hipotiroidismo primario supusieron casi la mitad de las primeras visitas.
ConclusionesSe atendieron una amplia variedad de patologías, algunas de las cuales están entre las más prevalentes en la población general y otras que son poco prevalentes, pero complejas, y difícilmente manejables por otras especialidades. El conocer y analizar estos datos permitirá identificar oportunidades de mejora y poner en marcha acciones en este sentido.
Endocrinology and Nutrition is the branch of Medicine involving the study of the physiology and pathology of the endocrine system, the metabolism of nutritional substances and natural and artificial nutrition, health promotion through the prevention of diet-related diseases, and the corresponding diagnostic, therapeutic and preventive techniques used in these areas of medical knowledge.1
Endocrinology and Nutrition Departments provide patient care, while also carrying out teaching, management and research. The healthcare activities are performed both in-hospital (in-patients and day hospital admissions) and out of hospital, through the Endocrinology and Nutrition outpatient clinics.1
The prevalence and incidence of many endocrine and nutritional disorders are known, and there are even studies that address this issue as a whole,2,3 but not all these disorders receive (or require) the same attention, nor are they all managed by specialists in Endocrinology and Nutrition. Moreover, there is little in the literature on the disorders treated in Endocrinology and Nutrition outpatient clinics, and what there is refers to settings very different from ours.4
The study entitled Healthcare Activity at the Endocrinology and Nutrition Outpatient Clinics of Castilla-La Mancha (AACENCAM) was sponsored by the Castellano-Manchega Society of Endocrinology, Nutrition and Diabetes and was designed to identify the characteristics of the patients attending the Castilla-La Mancha Health Service Endocrinology and Nutrition outpatients clinics, and to analyse the specific types of disorder seen in these consultations.
Material and methodsThe AACENCAM study was a retrospective cross-sectional study that analysed the outpatient clinic activity at the Endocrinology and Nutrition departments of the public hospitals of Castilla-La Mancha in 2018.
A randomly chosen sample was selected from among all the working days of 2018, stratified by day of the week and quarter of the year, and all the healthcare activity from consultations on those days was collected (except for the provision of ultrasound/thyroid FNA and other techniques specific to the speciality). The days selected were the same for all hospitals. If any of the selected days coincided with a holiday in one of the centres, another day from the same quarter and the same day of the week was randomly selected for that centre.
Variables analysedFor each outpatient consultation, the age and gender of the patient, whether it was a first or subsequent consultation and whether face-to-face or not, and up to five diagnoses from a predetermined list were recorded (Table 1). Even if no principal diagnosis was defined, the investigators tabulated in first place the diagnosis that in their opinion was the reason for the patient attending the Endocrinology or Nutrition outpatient clinic, and called this the “first diagnosis”. If several of the diagnoses the patient was being treated for were of equal importance, the order in which they were recorded was at the discretion of each investigator.
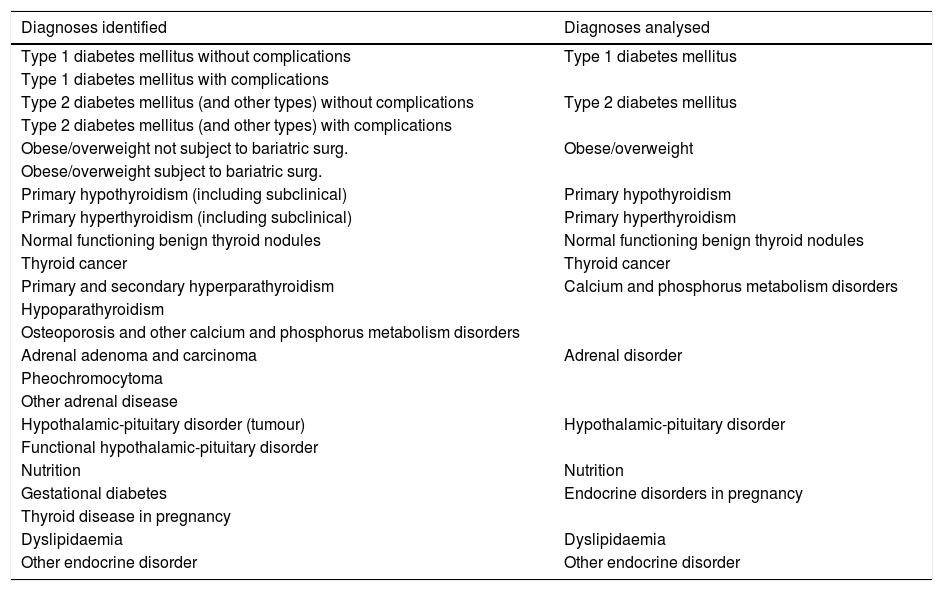
Relationship between diagnoses identified and diagnoses analysed.
| Diagnoses identified | Diagnoses analysed |
|---|---|
| Type 1 diabetes mellitus without complications | Type 1 diabetes mellitus |
| Type 1 diabetes mellitus with complications | |
| Type 2 diabetes mellitus (and other types) without complications | Type 2 diabetes mellitus |
| Type 2 diabetes mellitus (and other types) with complications | |
| Obese/overweight not subject to bariatric surg. | Obese/overweight |
| Obese/overweight subject to bariatric surg. | |
| Primary hypothyroidism (including subclinical) | Primary hypothyroidism |
| Primary hyperthyroidism (including subclinical) | Primary hyperthyroidism |
| Normal functioning benign thyroid nodules | Normal functioning benign thyroid nodules |
| Thyroid cancer | Thyroid cancer |
| Primary and secondary hyperparathyroidism | Calcium and phosphorus metabolism disorders |
| Hypoparathyroidism | |
| Osteoporosis and other calcium and phosphorus metabolism disorders | |
| Adrenal adenoma and carcinoma | Adrenal disorder |
| Pheochromocytoma | |
| Other adrenal disease | |
| Hypothalamic-pituitary disorder (tumour) | Hypothalamic-pituitary disorder |
| Functional hypothalamic-pituitary disorder | |
| Nutrition | Nutrition |
| Gestational diabetes | Endocrine disorders in pregnancy |
| Thyroid disease in pregnancy | |
| Dyslipidaemia | Dyslipidaemia |
| Other endocrine disorder | Other endocrine disorder |
After data collection, some diagnoses were grouped as shown in Table 1, such that in the secondary variable “any diagnosis”, all categories had a minimum proportion of 2% so that the confidence interval for the proportion did not include 0. In a second phase, all the recorded diagnoses were considered for analysis as if there were a single diagnosis at each visit (that is, if two diagnoses were recorded at one visit, it was counted as two visits), calling this variable “any diagnosis”.
Statistical analysisFor the statistical analysis, the computer program R, version 3.5.2 was used,5 through the integrated development environment RStudio.6
Age, in years, was analysed as a continuous variable and the results expressed as mean and standard deviation. Gender, and whether or not the visit was face-to-face are expressed as a percentage with the 95% confidence interval, calculated using the epi.conf function of the epiR package version 1.0–2.7 The subsequent/first visit ratio and its confidence interval were calculated with the same function, as odds, not as a percentage.
The proportion of the different diagnoses recorded as first diagnosis and as “any diagnosis” were analysed, calculating the percentage of each with its 95% confidence interval, determined using the MultinomCI function of the DescTools package version 0.99.28.8 With the same function, the percentage of visits at which one, two, three, four or five diagnoses had been recorded was also calculated.
The subsequent/first visit ratio was calculated for each diagnosis recorded as first diagnosis with the same function used to calculate the overall subsequent/first ratio.
With the set of diagnoses, regardless of the order in which they were recorded (“any diagnosis” variable), the age and proportion of females for each diagnosis were calculated.
Last of all, the proportion of diagnoses recorded as first diagnosis at first visits was calculated, in order to determine why the patients were referred to the Endocrinology and Nutrition clinic. The MultinomCI function of the DescTools package was also used for this calculation.
Sample sizeThe sample size was calculated so that the confidence intervals in estimating the proportions of the different consultation diagnoses were sufficiently narrow so that they could also be analysed for each Endocrinology and Nutrition Department (analysis not provided). At the same time, the size of the sample compared to the population seen had to be the same for all hospitals, so that the representation of each centre in the overall sample was proportional to its activity.
Through simulation with the MultinomCI function of the DescTools package, considering a total of 14 diagnoses, it was calculated that in order to have a confidence interval of ±3% in the proportions of first diagnoses for a hospital carrying out 6000 consultations per year, a sample of 600 consultations would be needed, so it was decided that the sample should be 10% of the working days, equating to 25 days.
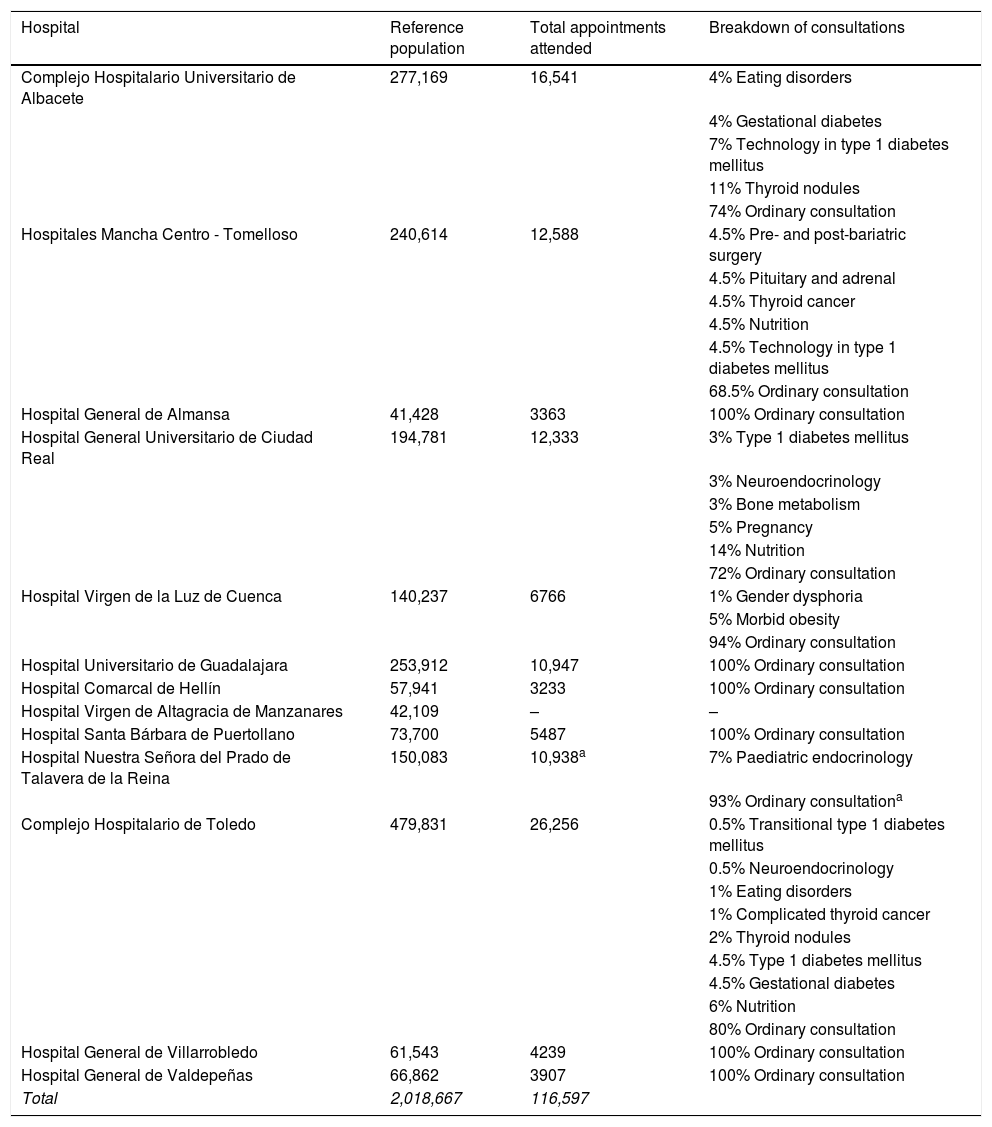
ResultsTable 2 shows the hospitals forming part of the Castilla-La Mancha Health Service which have an Endocrinology and Nutrition Department/Section/Unit and the outpatient clinic activity of those that participated in the AACENCAM study (12 of 13); in 2018, they carried out 116,597 consultations, 27,398 of which were first appointments and 89,199 subsequent visits. The analysed sample consisted of 10,709 consultations, 2427 of which were first appointments and 8282 subsequent visits, giving a subsequent to first ratio of 3.4 (3.3–3.6). Table 2 also shows the proportion of clinic time (number of patients) devoted at each centre to ordinary consultations and to specific-disorder specialised consultations.
Public hospitals in Castilla-La Mancha with an Endocrinology and Nutrition department/section/unit.
| Hospital | Reference population | Total appointments attended | Breakdown of consultations |
|---|---|---|---|
| Complejo Hospitalario Universitario de Albacete | 277,169 | 16,541 | 4% Eating disorders |
| 4% Gestational diabetes | |||
| 7% Technology in type 1 diabetes mellitus | |||
| 11% Thyroid nodules | |||
| 74% Ordinary consultation | |||
| Hospitales Mancha Centro - Tomelloso | 240,614 | 12,588 | 4.5% Pre- and post-bariatric surgery |
| 4.5% Pituitary and adrenal | |||
| 4.5% Thyroid cancer | |||
| 4.5% Nutrition | |||
| 4.5% Technology in type 1 diabetes mellitus | |||
| 68.5% Ordinary consultation | |||
| Hospital General de Almansa | 41,428 | 3363 | 100% Ordinary consultation |
| Hospital General Universitario de Ciudad Real | 194,781 | 12,333 | 3% Type 1 diabetes mellitus |
| 3% Neuroendocrinology | |||
| 3% Bone metabolism | |||
| 5% Pregnancy | |||
| 14% Nutrition | |||
| 72% Ordinary consultation | |||
| Hospital Virgen de la Luz de Cuenca | 140,237 | 6766 | 1% Gender dysphoria |
| 5% Morbid obesity | |||
| 94% Ordinary consultation | |||
| Hospital Universitario de Guadalajara | 253,912 | 10,947 | 100% Ordinary consultation |
| Hospital Comarcal de Hellín | 57,941 | 3233 | 100% Ordinary consultation |
| Hospital Virgen de Altagracia de Manzanares | 42,109 | – | – |
| Hospital Santa Bárbara de Puertollano | 73,700 | 5487 | 100% Ordinary consultation |
| Hospital Nuestra Señora del Prado de Talavera de la Reina | 150,083 | 10,938a | 7% Paediatric endocrinology |
| 93% Ordinary consultationa | |||
| Complejo Hospitalario de Toledo | 479,831 | 26,256 | 0.5% Transitional type 1 diabetes mellitus |
| 0.5% Neuroendocrinology | |||
| 1% Eating disorders | |||
| 1% Complicated thyroid cancer | |||
| 2% Thyroid nodules | |||
| 4.5% Type 1 diabetes mellitus | |||
| 4.5% Gestational diabetes | |||
| 6% Nutrition | |||
| 80% Ordinary consultation | |||
| Hospital General de Villarrobledo | 61,543 | 4239 | 100% Ordinary consultation |
| Hospital General de Valdepeñas | 66,862 | 3907 | 100% Ordinary consultation |
| Total | 2,018,667 | 116,597 |
Reference population of public hospitals in Castilla-La Mancha (according to the census, approximately 5% of the population consists of beneficiaries of Mutualidad General de Funcionarios Civiles del Estado (MUFACE) [General Mutual Fund for Spanish Civil Servants], Instituto Social de las Fuerzas Armadas (ISFAS) [Social Institute of the Armed Forces] or Mutualidad General Judicial (MUGEJU) [General Judicial Mutual Fund]), total appointments attended in 2018 at the Endocrinology and Nutrition departments/sections/units participating in this study and breakdown of the outpatient appointments at each centre, expressing the percentage of the clinic time devoted to specialist and ordinary consultations. There are no clinic data for Hospital Virgen de Altagracia de Manzanares as this centre did not participate in the study.
The age of the patients was 52.1?±?18.2 years (mean?±?standard deviation) with a median of 53.1 years and an interquartile range from 38.1 to 66.3 years, the proportion of females was 67.1% (66.3–67.9), and 97.9% (97.7–98.2) of the consultations were face-to-face.
A single diagnosis was recorded in 52.1% (51.1–53.2) of the consultations, two diagnoses in 27.6% (26.6–28.6), three in 15.6% (14.6–16.6) and four in 3.8% (2.8–4.0). Five diagnoses were only recorded in 0.8% (0–1.9) of the consultations.
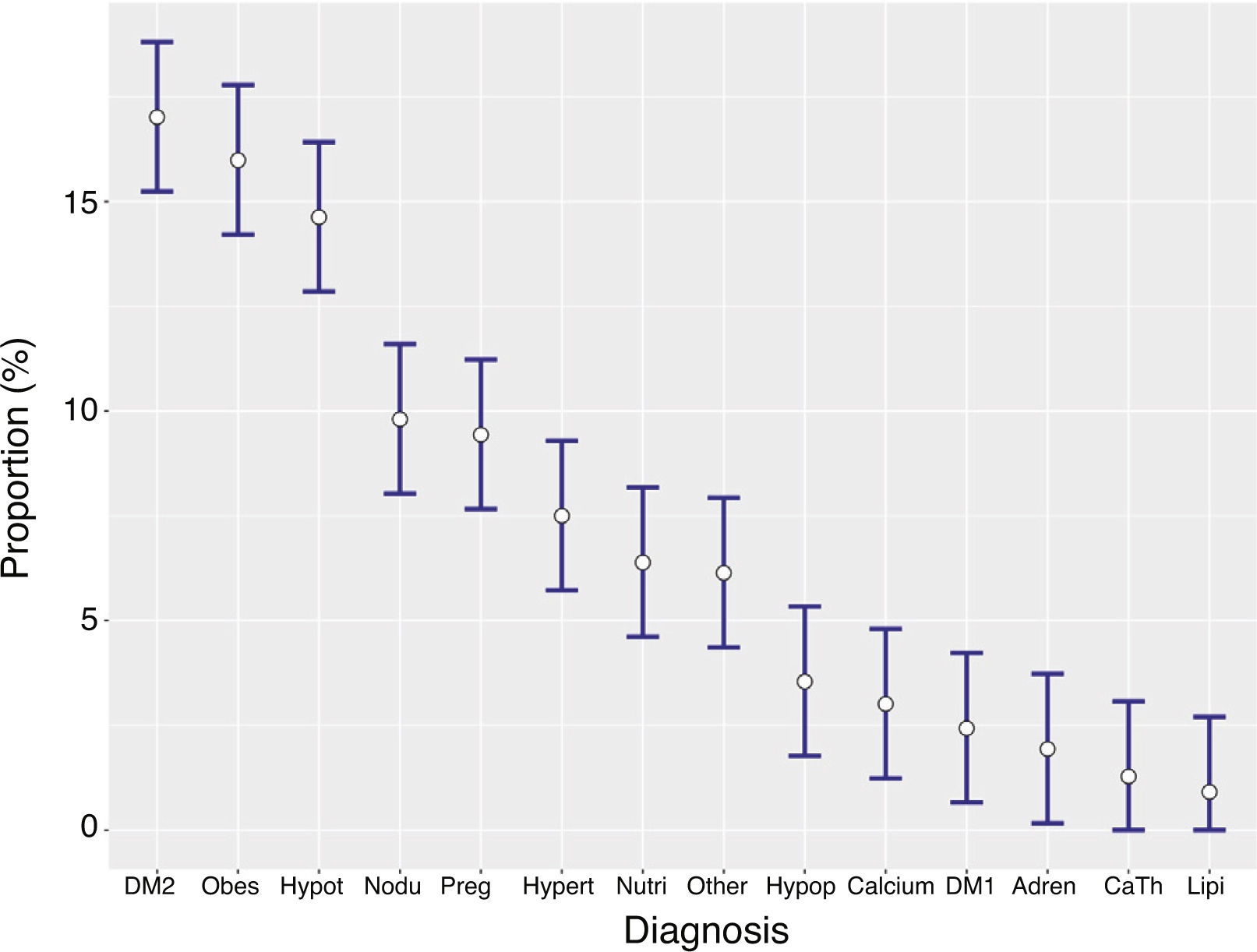
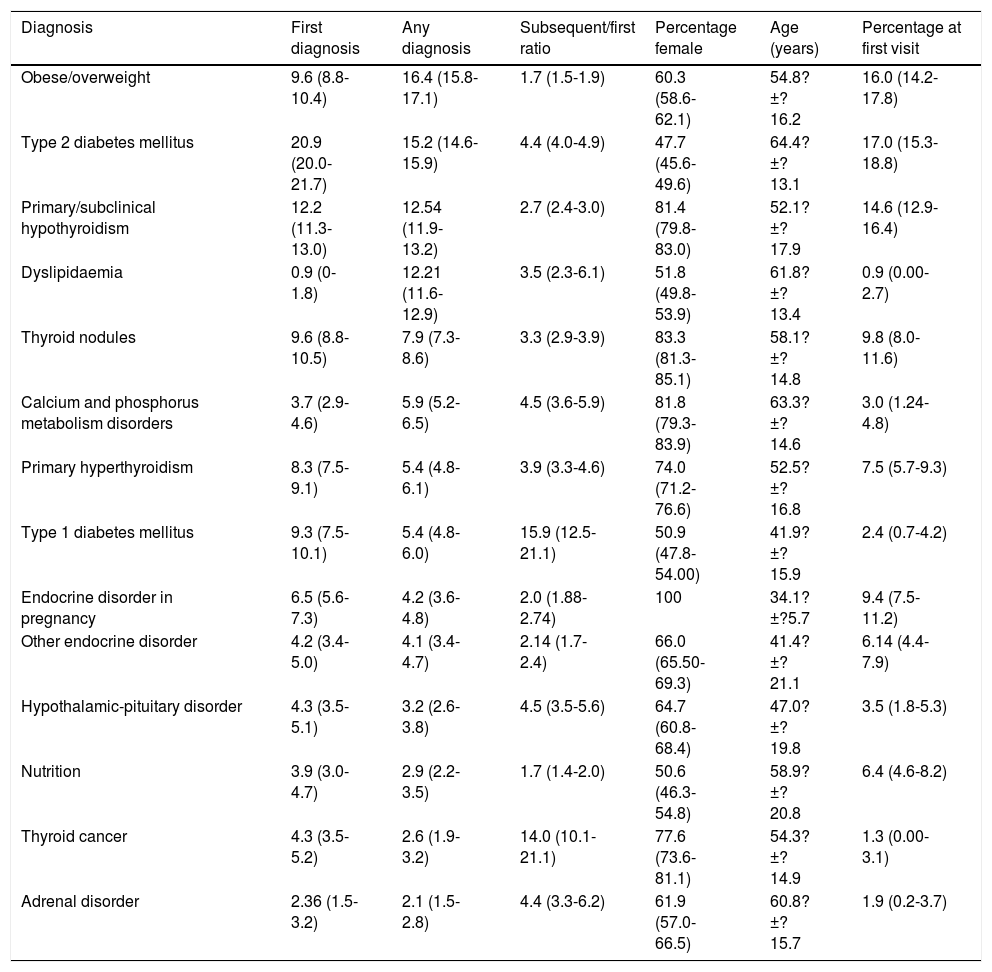
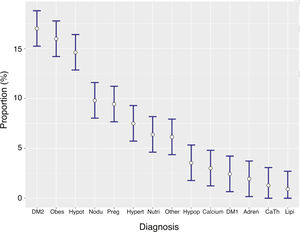
Type 2 diabetes mellitus, primary hypothyroidism, thyroid nodules and obesity/being overweight were the most common disorders recorded as first diagnosis, together accounting for over half of all visits. Table 3 (Fig. 1) shows the proportions of diagnoses recorded as first diagnosis.
Analysis of diagnoses.
| Diagnosis | First diagnosis | Any diagnosis | Subsequent/first ratio | Percentage female | Age (years) | Percentage at first visit |
|---|---|---|---|---|---|---|
| Obese/overweight | 9.6 (8.8-10.4) | 16.4 (15.8-17.1) | 1.7 (1.5-1.9) | 60.3 (58.6-62.1) | 54.8?±?16.2 | 16.0 (14.2-17.8) |
| Type 2 diabetes mellitus | 20.9 (20.0-21.7) | 15.2 (14.6-15.9) | 4.4 (4.0-4.9) | 47.7 (45.6-49.6) | 64.4?±?13.1 | 17.0 (15.3-18.8) |
| Primary/subclinical hypothyroidism | 12.2 (11.3-13.0) | 12.54 (11.9-13.2) | 2.7 (2.4-3.0) | 81.4 (79.8-83.0) | 52.1?±?17.9 | 14.6 (12.9-16.4) |
| Dyslipidaemia | 0.9 (0-1.8) | 12.21 (11.6-12.9) | 3.5 (2.3-6.1) | 51.8 (49.8-53.9) | 61.8?±?13.4 | 0.9 (0.00-2.7) |
| Thyroid nodules | 9.6 (8.8-10.5) | 7.9 (7.3-8.6) | 3.3 (2.9-3.9) | 83.3 (81.3-85.1) | 58.1?±?14.8 | 9.8 (8.0-11.6) |
| Calcium and phosphorus metabolism disorders | 3.7 (2.9-4.6) | 5.9 (5.2-6.5) | 4.5 (3.6-5.9) | 81.8 (79.3-83.9) | 63.3?±?14.6 | 3.0 (1.24-4.8) |
| Primary hyperthyroidism | 8.3 (7.5-9.1) | 5.4 (4.8-6.1) | 3.9 (3.3-4.6) | 74.0 (71.2-76.6) | 52.5?±?16.8 | 7.5 (5.7-9.3) |
| Type 1 diabetes mellitus | 9.3 (7.5-10.1) | 5.4 (4.8-6.0) | 15.9 (12.5-21.1) | 50.9 (47.8-54.00) | 41.9?±?15.9 | 2.4 (0.7-4.2) |
| Endocrine disorder in pregnancy | 6.5 (5.6-7.3) | 4.2 (3.6-4.8) | 2.0 (1.88-2.74) | 100 | 34.1?±?5.7 | 9.4 (7.5-11.2) |
| Other endocrine disorder | 4.2 (3.4-5.0) | 4.1 (3.4-4.7) | 2.14 (1.7-2.4) | 66.0 (65.50-69.3) | 41.4?±?21.1 | 6.14 (4.4-7.9) |
| Hypothalamic-pituitary disorder | 4.3 (3.5-5.1) | 3.2 (2.6-3.8) | 4.5 (3.5-5.6) | 64.7 (60.8-68.4) | 47.0?±?19.8 | 3.5 (1.8-5.3) |
| Nutrition | 3.9 (3.0-4.7) | 2.9 (2.2-3.5) | 1.7 (1.4-2.0) | 50.6 (46.3-54.8) | 58.9?±?20.8 | 6.4 (4.6-8.2) |
| Thyroid cancer | 4.3 (3.5-5.2) | 2.6 (1.9-3.2) | 14.0 (10.1-21.1) | 77.6 (73.6-81.1) | 54.3?±?14.9 | 1.3 (0.00-3.1) |
| Adrenal disorder | 2.36 (1.5-3.2) | 2.1 (1.5-2.8) | 4.4 (3.3-6.2) | 61.9 (57.0-66.5) | 60.8?±?15.7 | 1.9 (0.2-3.7) |
Percentage of diagnoses between the first diagnoses and overall diagnoses, subsequent/first visit ratio for first diagnosis, percentage of females and age by diagnosis, and percentage of first diagnosis at the first visit.
The 95% confidence interval is given for the percentages and the subsequent/first visit ratio, while the mean and standard deviation are given for age.
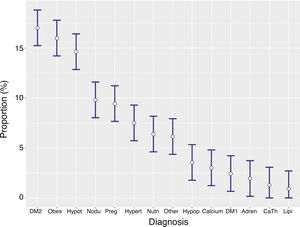
Proportion of diagnoses recorded as first diagnosis. The bars represent the 95% confidence interval.
Adren: adrenal disorder; CaTh: thyroid cancer; DM1: type 1 diabetes mellitus; DM2: type 2 diabetes mellitus and other diabetes mellitus; Hypert: primary hyperthyroidism; Hypop: hypothalamic-pituitary disorder; Hypot: hypothyroidism; Lipi: dyslipidaemia; Nodu: nodular thyroid disease; Nutri: nutrition; Obes: obese/overweight; Other: other endocrine disorder; Preg: endocrine abnormalities in pregnancy.
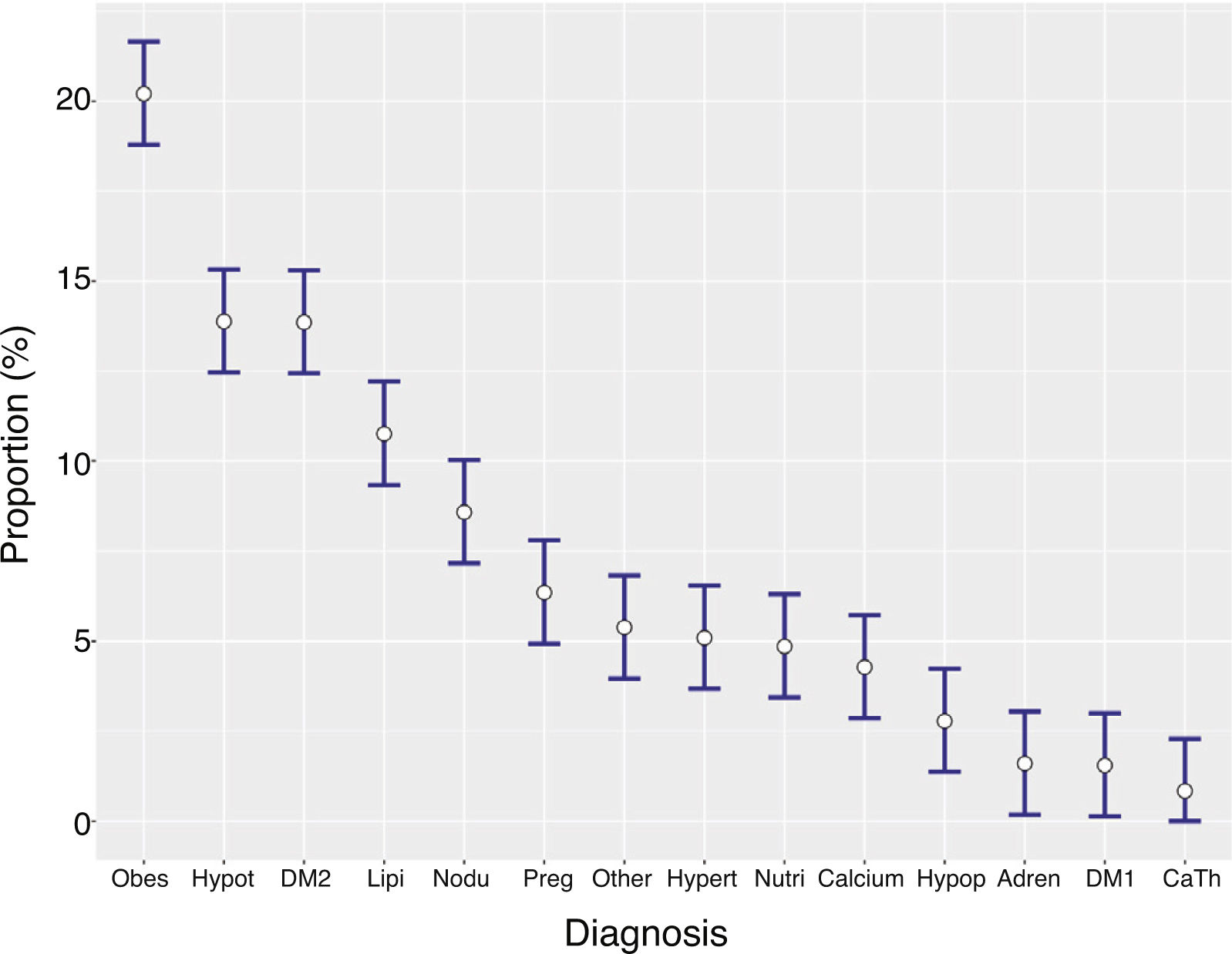
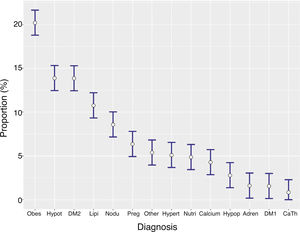
Taking into account all the diagnoses, regardless of whether recorded as first or not, there were a total of 18,602 diagnoses in the 10,709 visits analysed. Obesity, type 2 diabetes mellitus, primary hypothyroidism and dyslipidaemia accounted for more than half of the diagnoses. Table 3 (Fig. 2) shows the proportions for all the diagnoses recorded.
Proportion of diagnoses regardless of the order in which they were recorded. The bars represent the 95% confidence interval.
Adren: adrenal disorder; CaTh: thyroid cancer; DM1: type 1 diabetes mellitus; DM2: type 2 diabetes mellitus and other diabetes mellitus; Hypert: primary hyperthyroidism; Hypop: hypothalamic-pituitary disorder; Hypot: hypothyroidism; Lipi: dyslipidaemia; Nodu: nodular thyroid disease; Nutri: nutrition; Obes: obese/overweight; Other: other endocrine disorder; Preg: endocrine abnormalities in pregnancy.
In terms of principal diagnosis, type 1 diabetes mellitus and thyroid cancer were found to have the biggest subsequent/first ratio (Table 3). Apart from type 2 diabetes mellitus, there was a female predominance in all other diagnoses (Table 3). The highest mean age was found in patients whose diagnosis was type 2 diabetes mellitus, while patients with endocrine disorders in pregnancy were the youngest (Table 3).
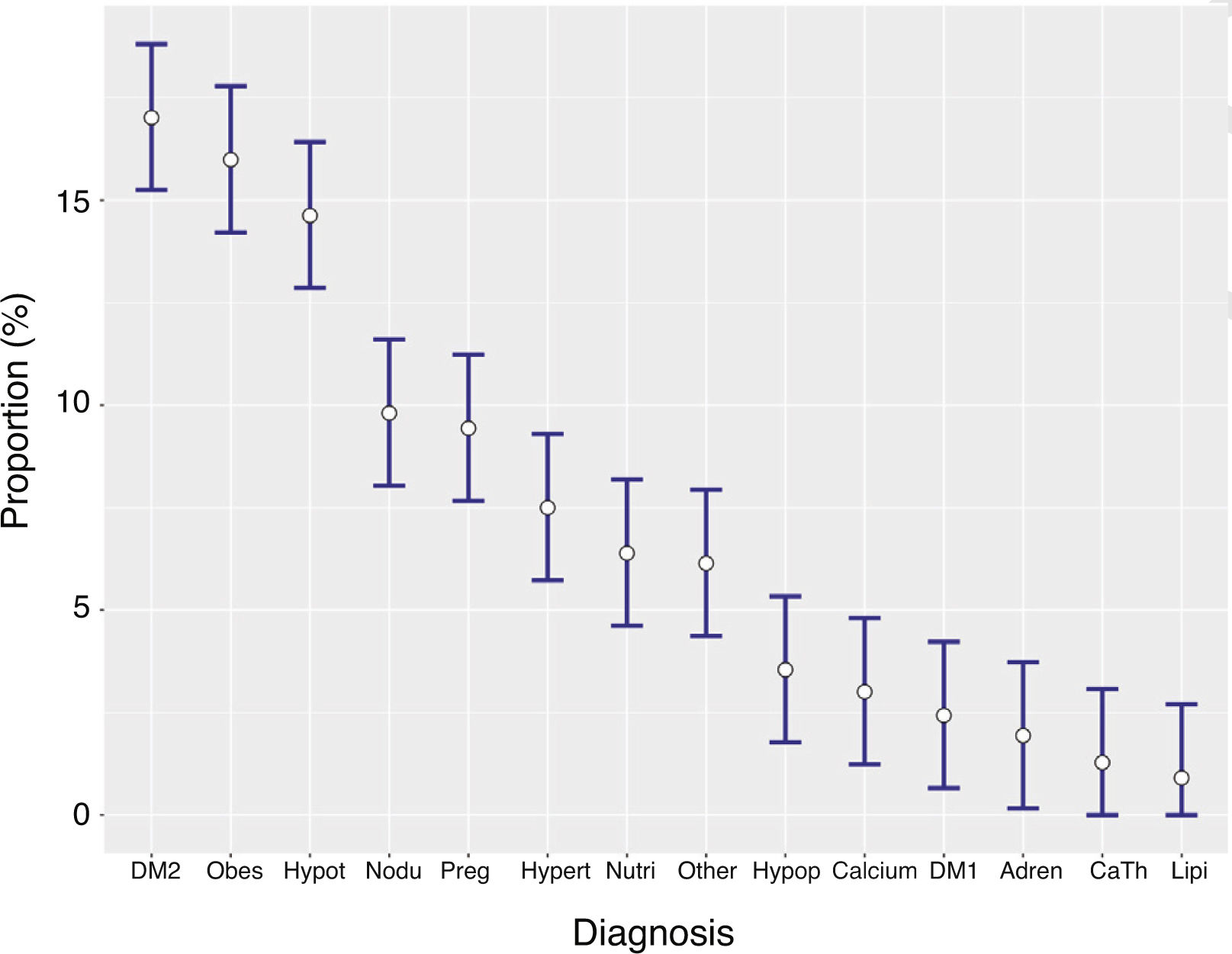
Type 2 diabetes mellitus, obesity and primary hypothyroidism accounted for almost half of the diagnoses for which the patients were seen at the first visit (Table 3, Fig. 3).
Proportion of primary diagnoses at first visits. The bars represent the 95% confidence interval.
Adren: adrenal disorder; CaTh: thyroid cancer; DM1: type 1 diabetes mellitus; DM2: type 2 diabetes mellitus and other diabetes mellitus; Hypert: primary hyperthyroidism; Hypop: hypothalamic-pituitary disorder; Hypot: hypothyroidism; Lipi: dyslipidaemia; Nodu: nodular thyroid disease; Nutri: nutrition; Obes: obese/overweight; Other: other endocrine disorder; Preg: endocrine abnormalities in pregnancy.
We have presented here what, to our knowledge, is the first multicentre study on clinical activity in Endocrinology and Nutrition outpatient clinics for an entire Autonomous Region Health Service in Spain.
Our results confirm that more females than males tend to be treated by Endocrinology and Nutrition departments, with a wide range of ages.
The subsequent/first visit ratio is very similar to that published for the whole of Spain in the RECALSEEN study,9 being 0.15 higher in this sample than that obtained with the data for all first and subsequent consultations provided by the different health administrations (0.04 if the lower limit of the confidence interval is considered). This may be due to the fact that the patient data compiled in the different appointment books for non-clinical purposes were not collected (mainly administrative and management).
The percentage of non-face-to-face consultations is lower than that recorded in the RECALSEEN study, and considering that the region of Castilla-La Mancha is widely dispersed geographically, this would be an opportunity for improvement, particularly as promoting telemedicine is one of this speciality's strategic objectives.10
Almost half of the patients seen in the clinics had more than one diagnosis. Obesity, and especially dyslipidaemia, were both markedly less represented among the main diagnoses than among the overall diagnoses, while the opposite was true of type 2 diabetes mellitus. This is because both obesity and dyslipidaemia were very often companion diagnoses to type 2 diabetes mellitus in our series.
As might be expected, type 2 diabetes mellitus, obesity and thyroid disorder, both functional and nodular, were some of the disorders most seen by endocrinologists in Castilla-La Mancha. In a study specific to Castilla-La Mancha, the prevalence of diabetes in subjects aged over 20 years was 17.9% (10.7% of known diabetes mellitus),11 while the ENPE study revealed a prevalence of overweight and obese patients in Castilla-La Mancha of 40% and 23.6%, respectively.12 We do not have statistics on the prevalence of other disorders in the general population of Castilla-La Mancha, but the conditions most treated in our clinics are broadly in line with those most prevalent in other regions, such as the United States.2 Studies carried out in settings very different from ours show a much higher proportion of patients with type 2 diabetes mellitus than in our clinics.4
The principal diagnosis of more than 10% of the consultations was for complex conditions that are difficult to refer to Primary Care or other specialities, such as hypothalamic-pituitary disorders, thyroid cancer or adrenal disease. Meanwhile almost another 10% of the consultations were for type 1 diabetes mellitus. These diagnoses consequently had a much higher subsequent/first visit ratio than the rest. However, analysing this ratio by diagnoses, we have to take into account that some of these disorders are under-represented in the first consultations (for example, the patient who is seen at a subsequent visit for thyroid cancer was seen at the first visit for a thyroid nodule, or many patients with type 1 diabetes are seen for the first time on admission, coinciding with the onset, and the first consultation at the outpatient clinic is recorded as subsequent).
Patients with nutritional disorders accounted for 6.4% of the first consultations and 3.9% of the principal diagnoses, showing the lowest subsequent/first ratio of all the diagnoses analysed. Despite much of the growth of our speciality in recent years having taken place in the area of Clinical Nutrition,9 the current provision of specialists in the specific field of Nutrition remains insufficient in most hospitals,10 as patients who require nutritional care are often complex and frail.9 As such, we believe there is an opportunity to improve the care of these patients by increasing the number of check-ups they are offered.
One type of condition in particular that we analysed was endocrine disorders in pregnancy, mainly gestational diabetes and subclinical hypothyroidism, which accounted for almost 10% of the first consultations. Although these disorders are not particularly complex, they do require a quick response after referral from Obstetrics or Primary Care. Coordination protocols with these specialities and, in some cases, non-face-to-face consultations would facilitate a more efficient response.
The AACENCAM study did not consider the diagnostic and therapeutic techniques specific to the speciality, such as thyroid and muscle ultrasound and impedance measurement, or technologies applied to diabetes. This was because the number of procedures was much lower than the number of consultations attended, and as they were not available in all the hospitals, the data obtained from the sample analysed would not have had the robustness of the analysis of the consultation diagnoses. However, given the importance of these techniques for the future of the speciality of Endocrinology and Nutrition, a study with regional scope, sample size and sampling technique specifically aimed at obtaining reliable information on the subject should be designed.
One limitation of our project is that it is a retrospective study that analysed a sample of approximately 10% of the total number of patients seen. However, because more than 10,000 consultations were compiled by stratified randomised sampling, in which all the activity of all the appointment books was collected on a series of days of the year (randomly chosen), where all the days of the week and all the quarters of the year were equally represented, significantly reduces the likelihood of bias. Even in the case of disorders treated in specialist clinics, more exposed to sampling bias as they are not held on a daily basis, the fact that for less prevalent diseases, specialist clinics are only available in some of our centres and for some of these disorders, and given the stratified sampling method, we believe the sample is sufficiently representative.
Our results are in line with those of other studies carried out by groups belonging to the Castellano-Manchega Society of Endocrinology, Nutrition and Diabetes on specific disorders. In our study, 50.6% of the patients with type 1 diabetes mellitus were female, with a mean age of 41.9 years, while in the DIACAM1 study (published six years ago) 49.5% were female and the mean age was 39 years.13 The mean age of the patients with thyroid cancer in our study was 54.3 years, with 77.6% being female, while in the CADIT-CAM study, 77% of the patients were female with a mean age of 54 years.14 Lastly, in our study, 61.9% of the patients with adrenal disease were female, albeit with a confidence interval of 57.0%–66.5%, and the mean age was 60.8 years, while in the study by Lamas et al. on adrenal incidentalomas, 53% of the patients were female with a mean age of 60.3 years.15
The RECALSEEN study revealed differences in Endocrinology and Nutrition activities between different Autonomous Region Health Services in Spain,9 so our results do not have to be directly comparable to those of other parts of the country. However, our methodology is applicable to studies that can be carried out in other autonomous regions or even in Spain as a whole.
One of the strengths of our study is that it is the first to analyse the clinical activities of the Endocrinology and Nutrition outpatient clinics of practically all the hospitals of an autonomous region health service, with a random sample of thousands of consultations.
In short, our study shows that endocrinologists treat patients with a wide variety of disorders, some of which are among the most prevalent in the general population, while others are far less prevalent but complex and difficult to refer to Primary Care or other specialities. Having collected and analysed these data, not only at the regional level but at each individual centre, we can now identify opportunities for improvement and implement actions in this regard. As Lord Kelvin said, “When you can measure what you are speaking about, and express it in numbers, you know something about it; but when you cannot measure it, when you cannot express it in numbers, your knowledge is of a meagre and unsatisfactory kind”,16 and, clearly, you cannot improve something that you are not aware of.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Albacete
- •
Francisco Botella Romero
- •
Silvia Aznar Rodríguez
- •
Lourdes García Blasco
- •
Cortes María Jiménez Martínez
- •
Cristina Lamas Oliveira
- •
Luz María López Jiménez
- •
Jose Juan Lozano García
- •
Pedro José Pinés Corrales
- •
Alejandro Esteban Sirvent Segovia
Alcázar de San Juan-Tomelloso
- •
Cristina Contreras Pascual
- •
Álvaro García Manzanares Vazquez de Agredos
- •
Paloma González Lázaro
- •
Francisco Javier Gomez Alfonso
- •
Julia Silva Fernandez
- •
Florentino del Val Zaballos
Ciudad Real
- •
Miguel Aguirre Sánchez-Covisa
- •
Manuel Delgado del Rey
- •
Belen Fernandez de Bobadilla
- •
Abel Gonzalez González
- •
Carlos Roa Llamazares
- •
Pedro Rozas Moreno
Cuenca
- •
Mubarak Alramadan Aljamalah
- •
David Martín Iglesias
- •
José Pérez Rodríguez
- •
Javier González López
Guadalajara
- •
Visitación Alvarez de Frutos
- •
Marta Cano Mejias
- •
Sandra Herranz Antolín
Talavera
- •
Benito Blanco Samper
- •
Iván Quiroga López
Toledo
- •
Bárbara Cánovas Gaillemin
- •
Enrique Castro Martínez
- •
Andrea Cruz Gordillo
- •
José López López
- •
Ofelia Llamazares Iglesias
- •
Esther Maqueda Villaizán
- •
Amparo Marco Martínez
- •
Julia Sastre Marcos
- •
Almudena Vicente Delgado
Villarrobledo
- •
María Olmos Alemán
Please cite this article as: Alfaro Martínez J-J, Peña-Cortés V-M, Gómez-García I-R, Platero-Rodrigo E, Moreno-Fernandez J, Calderón-Vicente D-M, et al. Actividad asistencial en las consultas de Endocrinología y Nutrición de Castilla-La Mancha (estudio AACENCAM). Endocrinol Diabetes Nutr. 2021;68:251–259.