To evaluate the impact of obesity and overweight on surgical outcomes in a large cohort of patients who underwent adrenalectomy due to benign or malignant primary adrenal disease.
MethodsA retrospective single-center study of patients without history of active extraadrenal malignancy, with adrenal tumors operated on consecutively in our center between January 2010 and December 2022. Obesity was defined as a body mass index (BMI)≥30kg/m2 and overweight as BMI between 25.0 and 30.0kg/m2.
ResultsOf 146 patients with adrenal tumors who underwent adrenalectomy, 9.6% (n=14) were obese, 54.8% (n=80) overweight and 35.6% (n=52) normal weight. Obese patients had higher diastolic blood pressure (87.6±12.22 vs. 79.3±10.23mmHg, P=0.010) and a higher prevalence of dyslipidemia (57.1% vs. 25.8%, P=0.014) and bilateral tumors (14.3% vs. 3.1%, P=0.044) than non-obese patients. The rates of intraoperative and of postsurgical complications were similar between obese/overweight patients and patients with normal weight. However, a significantly higher rate of postsurgical complications (27.3% vs. 5.7%, P=0.009) and a longer hospital stay (5.4±1.39 vs. 3.5±1.78 days, P=0.007) were observed in patients with obesity than in non-obese patients. In the multivariant analysis, obesity, age, ASA>2 and tumor size were independent risk factors for postoperative complications, with obesity being the most important factor (OR 23.34 [2.23–244.24]).
ConclusionObesity and overweight are common conditions in patients who undergo adrenalectomy. Adrenalectomy is considered a safe procedure in patients with overweight, but it is associated with a higher risk of postsurgical complications and longer hospital stay in obese patients.
Evaluar el impacto de la obesidad y el sobrepeso en los resultados quirúrgicos en una cohorte de pacientes que se sometieron a adrenalectomía debido a enfermedad suprarrenal primaria benigna o maligna.
MétodosEstudio unicéntrico retrospectivo de pacientes sin antecedentes de neoplasia maligna extraadrenal activa con tumores suprarrenales operados de forma consecutiva en nuestro centro durante enero de 2010 y diciembre de 2022. Se definió obesidad como un índice de masa corporal (IMC) ≥30kg/m2 y sobrepeso como un IMC entre 25,0 y 30,0kg/m2.
ResultadosDe 146 pacientes con tumores suprarrenales a los que se les realizó adrenalectomía, el 9,6% (n=14) presentaba obesidad, el 54,8% (n=80) sobrepeso y el 35,6% (n=52) normopeso. Los pacientes obesos tenían cifras más altas de tensión arterial diastólica (87,6±12,22 vs. 79,3±10,23mmHg; p=0,010) y una mayor prevalencia de dislipemia (57,1 vs. 25,8%; p=0,014) y de tumores bilaterales (14,3 vs. 3,1%; p=0,044) que los pacientes no obesos. La tasa de complicaciones intraoperatorias y posquirúrgicas fue similar entre pacientes obesos/con sobrepeso y pacientes con normopeso. Sin embargo, se observó una tasa significativamente mayor de complicaciones posquirúrgicas (27,3 vs. 5,7%; p=0,009) y una estancia hospitalaria más prolongada (5,4±1,39 vs. 3,5±1,78 días; p=0,007) en pacientes con obesidad que en los no obesos. En el análisis multivariante, la obesidad, la edad, un ASA>2 y el tamaño tumoral fueron factores de riesgo independientes de complicaciones postoperatorias, siendo la obesidad el factor más importante (OR: 23,34 [2,23-244,24]).
ConclusiónLa obesidad y el sobrepeso son condiciones frecuentes en los pacientes que se someten a adrenalectomía. La suprarrenalectomía se considera un procedimiento seguro en los pacientes con sobrepeso, pero se asocia con un mayor riesgo de complicaciones posquirúrgicas y a una mayor estancia hospitalaria en los pacientes obesos.
Obesity is an increasingly common disease worldwide.1 Patients with obesity are usually at higher risk of intraoperative and postoperative complications due to the greater difficulty of anesthetic management, higher rate of conversion to open surgery, and higher number of surgical wound infections among others.2
Adrenalectomy can be performed by different approaches (open, laparoscopic, or robot-assisted). Today, laparoscopic adrenalectomy is considered the first-line treatment for most adrenal tumors.3 It has been demonstrated that laparoscopy compared with open adrenalectomy has a lower risk of intraoperative morbidity, shorter hospital stays, and fewer postoperative complications.3,4 Nevertheless, open adrenalectomy is still the technique of choice in patients with large tumors or with signs of infiltration of adjacent tissues.4 The rise in the number of obese patients in recent years, has increased the difficulty of the surgical technique, with a higher rate of conversion to open surgery in laparoscopic adrenalectomy (1–22%).5 Some other studies have examined the results of laparoscopic adrenalectomy in obese and non-obese patients.6 However, most of these studies are retrospective, the number of patients included is usually low, and they do not distinguish whether the indication of surgery was for a primary tumor or for metastasis, taking into account that patients with a previous oncological history tend to have a lower weight than patients with a primary adrenal tumor. To overcome these limitations, we have included all consecutive patients with adrenal tumors operated on in our center, but we have excluded those patients with metastatic tumors in the adrenal gland.
The aim of our study is to evaluate the impact of obesity on surgical outcomes in adrenal gland surgery in a large cohort of patients who underwent adrenalectomy due to benign or malignant primary adrenal disease.
Material and methodsStudy populationWe designed a retrospective study performed at Ramón y Cajal University Hospital, Madrid, Spain, between January 1, 2010, and July 20, 2022. This study received approval from the Ethics Committee of our hospital (approval date: July 2020, Minutes 395). All patients diagnosed with an adrenal tumor who underwent adrenalectomy were included in the study. However, those with a history of active extra-adrenal malignancy and metastasis to the adrenal gland were excluded. In addition, two patients for whom information on anthropometric parameters was not available were excluded.
Data were extracted from the electronic medical records system and were collected in an electronic database (RedCAP® database). Information recorded in the database included demographic, clinical, biochemical, hormonal, radiological data, anesthetic risk [American Society of Anesthesiologists classification (ASA)], and variables related to preoperative, intraoperative, and surgical management.
Medical history of comorbidities at diagnosis including hypertension, type 2 diabetes mellitus, obesity, dyslipidemia, cerebrovascular, and cardiovascular disease, and physical examination variables including body mass index (BMI) and systolic and diastolic blood pressure were also recorded. Information about biochemical studies including fasting plasma glucose, total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, was recorded for most patients. All patients underwent unenhanced CT scan and/or MRI examinations at diagnosis. All specimens were analyzed following standardized protocols.
The term obesity was defined as a BMI≥30kg/m2. The remaining patients were included in the “non-obese” group characterized by a BMI<30kg/m2 (both overweight and appropriate weight patients were included here). Overweight was defined as a BMI between 25.0 and 30.0kg/m2. Cardiovascular disease, type 2 diabetes, hypertension and dyslipidemia were defined as we described in a previous work.7
The diagnosis of overt Cushing's syndrome, pheochromocytoma, and primary aldosteronism was based on the latest European guidelines. As we have previously reported,7 autonomous cortisol secretion (ACS) was defined as an adrenal tumor with cortisol post-dexamethasone suppression test (DST)>1.8μg/dl in the absence of specific clinical signs of hypercortisolism.8
Surgical technique and outcomesMost patients included in the study underwent laparoscopic adrenalectomy as the technique of choice (n=117). There were 29 patients operated on by an open approach. The choice of approach was based on the patient's tumor size and risk of malignancy, with the open approach being more common in patients with large tumors or higher risk of malignancy (adrenal carcinoma). Laparoscopic surgery was performed transperitoneally with the patients placed in a lateral decubitus position. Open surgery was performed through a transabdominal approach using a transverse incision just below the costal margin. All surgeries were conducted under general anesthesia. Only two patients required conversion to laparoscopic approach. All surgeries were conducted under general anesthesia.
As we have previously described,9 the intraoperative complications recorded include hypertensive crisis, intraoperative bleeding, an episode of maintained hypotension, arrhythmias, hemodynamic instability, and conversion to open surgery. Postoperative complications also included hypertensive crisis, a hypotensive episode, hypoglycemia, acute renal failure, paralytic ileus, need for transfusion, postoperative fever, and surgical wound infection. They were also classified based on their severity, following the classical Clavien–Dindo scale.10
Statistical analysisThe statistical analysis was performed using STATA.15. The assumption of normality was checked using the Shapiro–Wilk test. Categorical variables are expressed as percentages and absolute values and quantitative variables as mean±standard deviation or median and ranges depending on whether the variable had a normal distribution. When data are missing for a variable, the number of patients analyzed is indicated. A logistic regression model was used for the estimation of the odds ratios (OR) and 95% confidence intervals. The Chi2 test was performed for the comparison of categorical variables between independent groups and the t-test for comparison between means. In all cases, a two-tailed P value<0.05 or a 95% confidence interval of the OR not including the number 1, were considered statistically significant.
ResultsStudy populationA total of 146 patients were included in the study. The median age was 57.5 years (range 26.9–78.7) and 58.2% were women. There were 14 patients with obesity (9.6%) and 80 patients with overweight (54.8%). In the group of patients with obesity, 10 had grade I obesity and 4 grade II. The main indications of surgery were overt Cushing's syndrome in 18, pheochromocytoma in 36, primary aldosteronism in 30, ACS in 9, and tumor size greater than 40mm and/or atypical features in the remainder. The 6 patients with bilateral tumors had ACS or overt Cushing's syndrome. The baseline characteristics of the patients are described in Table 1.
Baseline characteristics of the cohort study (n=146).
| Variable | % (n) |
|---|---|
| Age | 56.2±12.51 |
| Women | 58.2% (85) |
| Type 2 diabetes | 26.7% (39) |
| Obesity | 9.6% (14) |
| Overweight or obesity | 64.4% (94) |
| Hypertension | 63.7% (93) |
| Cardiovascular disease | 4.1% (6) |
| Smoker (n=97) | 26.8% (26) |
| ASA>2 (n=138) | 16.6% (27) |
| Functionality | 63.7% (93) |
| Body mass index, kg/m2 | 26.3±3.06 |
| Systolic blood pressure | 137.1±15.60 |
| Diastolic blood pressure | 80.0±10.62 |
| Tumor size | 46.5±30.90 |
| Tumor size≥40mm | 58.2% (85) |
| Bilaterality | 4.1% (6) |
| Calcifications in CT (n=129) | 14.7% (19) |
| Necrosis in CT (n=129) | 7.8% (10) |
| Low lipid content (n=128) | 92.2% (118) |
| Hounsfield units (n=98) | 45.2±40.99 |
| Hounsfield units>10 (n=87) | 77.5% (76) |
ASA: American Society of Anesthesiologists classification.
No significant differences in presurgical characteristics were found between patients with and without obesity/overweight, except for a higher proportion of adrenal tumors with high lipid content in obese/overweight patients than in those with normal weight (Table 2). However, when we compared obese and non-obese (including overweight) patients, obese patients had higher diastolic blood pressure (87.6±12.22 vs.79.3±10.23mmHg, P=0.010) and a higher prevalence of dyslipidemia (57.1% vs. 25.8%, P=0.014) and bilateral tumors (14.3% vs. 3.1%, P=0.044) than non-obese patients.
Differences in presurgical, surgical and postsurgical variables between patients with and without obesity/overweight.
| Variable | Obese/overweight (N=94) | Normal weight (N=52) | P value |
|---|---|---|---|
| Presurgical variables | |||
| Age | 56.5±11.40 | 55.5±14.40 | 0.627 |
| Women | 54.3% (43) | 34.6% (n=18) | 0.192 |
| Type 2 diabetes | 28.7% (27) | 23.1% (n=12) | 0.460 |
| Hypertension | 68.1% (64) | 55.8% (n=29) | 0.138 |
| Cardiovascular disease | 3.2% (3) | 5.8% (3) | 0.452 |
| Dyslipidemia | 33.0% (31) | 21.2% (11) | 0.131 |
| Smoker | 27.8% (20) | 24.0% (6) | 0.713 |
| Pheochromocytoma | 26.6% (25) | 21.1% (11) | 0.465 |
| Cushing's syndrome | 14.9% (14) | 7.7% (4) | 0.205 |
| Primary aldosteronism | 19.2% (18) | 23.1% (12) | 0.574 |
| Autonomous cortisol secretion | 5.3% (5) | 7.7% (4) | 0.568 |
| ASA>2 | 24.4% (21) | 11.5% (6) | 0.065 |
| BMI, kg/m2 | 27.8±2.70 | 23.6±1.36 | <0.001 |
| Systolic blood pressure | 135.6±13.20 | 139.8±19.05 | 0.123 |
| Diastolic blood pressure | 80.2±10.87 | 79.6±10.25 | 0.749 |
| Fasting glucose, mg/dl | 107.3±46.31 | 113.9±31.62 | 0.474 |
| GFR, ml/min/1.73m2 | 82.4±12.06 | 81.6±14.21 | 0.766 |
| Tumor size | 44.4±27.66 | 50.1±36.04 | 0.286 |
| Tumor size≥40mm | 56.4% (53) | 61.5% (32) | 0.545 |
| Bilaterality | 6.4% (6) | 0% | 0.063 |
| Calcifications in CT (n=129) | 10.0% (8) | 22.5% (11) | 0.053 |
| Necrosis in CT (n=129) | 6.3% (5) | 10.2% (5) | 0.415 |
| High lipid content (n=128) | 12.5% (10) | 0% | 0.011 |
| Hounsfield units (n=98) | 49.0±42.83 | 39.5±37.83 | 0.263 |
| Hounsfield units>10 (n=87) | 78.0% (46) | 76.9% (30) | 0.904 |
| Open adrenalectomy | 18.1% (17) | 23.1% (12) | 0.469 |
| Surgical and postsurgical variables | |||
| Operative time, minutes | 124.2±53.21 | 122.6±50.70 | 0.878 |
| Intraoperative complications | 6.4% (6) | 7.7% (4) | 0.764 |
| Postsurgical complications | 9.5% (8) | 3.9% (2) | 0.228 |
| Hospital stay, days | 3.7±2.20 | 3.6±2.22 | 0.793 |
ASA: American Society of Anesthesiologists classification; BMI: body mass index; GFR: glomerular filtration rate.
A total of 10 patients with intraoperative complications were recorded: six patients had intraoperative bleeding, one had a hypertensive crisis together with intraoperative bleeding, one had hemodynamic instability, another patient had hemodynamic instability, asystole and intraoperative death, and the remaining patient was recorded as other complications. Postsurgical complications occurred in 10 patients and 5 were classified as Clavien–Dindo>2 (Fig. 1). The median length of hospital stay across the whole cohort was 3 days (range 2–15 days).
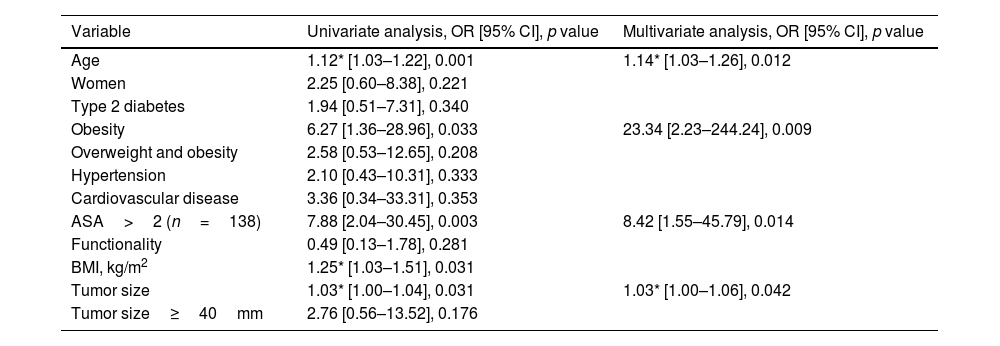
The rates of intraoperative and postsurgical complications were similar between obese/overweight patients and patients with normal weight. Nor was a difference found in hospital stay or duration of surgery. However, when we compared obese and non-obese patients, we observed a significantly higher proportion of postsurgical complications in the first group (27.3% vs. 5.7%, P=0.009) than in the second. Moreover, obese patients had a longer hospital stay (5.4±1.39 vs. 3.5±1.78, P=0.007) than non-obese patients (Fig. 2). No correlation was found between BMI and operative time (r=0.044, P=0.639) or hospital stay (r=0.129, P=0.150). In the multivariant analysis, obesity, age, ASA>2, and tumor size were independent risk factors for postoperative complications (Table 3).
Risk factors for postsurgical complications.
| Variable | Univariate analysis, OR [95% CI], p value | Multivariate analysis, OR [95% CI], p value |
|---|---|---|
| Age | 1.12* [1.03–1.22], 0.001 | 1.14* [1.03–1.26], 0.012 |
| Women | 2.25 [0.60–8.38], 0.221 | |
| Type 2 diabetes | 1.94 [0.51–7.31], 0.340 | |
| Obesity | 6.27 [1.36–28.96], 0.033 | 23.34 [2.23–244.24], 0.009 |
| Overweight and obesity | 2.58 [0.53–12.65], 0.208 | |
| Hypertension | 2.10 [0.43–10.31], 0.333 | |
| Cardiovascular disease | 3.36 [0.34–33.31], 0.353 | |
| ASA>2 (n=138) | 7.88 [2.04–30.45], 0.003 | 8.42 [1.55–45.79], 0.014 |
| Functionality | 0.49 [0.13–1.78], 0.281 | |
| BMI, kg/m2 | 1.25* [1.03–1.51], 0.031 | |
| Tumor size | 1.03* [1.00–1.04], 0.031 | 1.03* [1.00–1.06], 0.042 |
| Tumor size≥40mm | 2.76 [0.56–13.52], 0.176 |
ASA: American Society of Anesthesiologists classification; BMI: body mass index.
Nowadays, obesity/overweight has become an increasingly common feature in patients undergoing surgery, with rates ranging between 39% and 72% of patients undergoing adrenalectomy surgery according to some series.11 In our series, almost 10% of the patients are obese patients and up to 65% are obese or overweight; these rates are similar to other series described in the literature,12 or even have a lower percentage of obesity than other series.11 Moreover, in contrast to other studies, we have also analyzed the influence of overweight compared to obese patients.
In our cohort, obese/overweight patients had higher rates of high blood pressure (68.1%), dyslipidemia (33%) and type 2 diabetes mellitus (28.7%). These data are in agreement with other studies, where patients with obesity have higher rates of cardiovascular risk factors and metabolic syndrome.13 Furthermore, in our series, overweight patients have a higher prevalence of lipid-rich tumors, possibly explained by the fact that patients with metabolic syndrome have a higher tendency to have benign tumors related to Cushing's syndrome or ACS than patients with normal or low weight.14 In contrast, patients with adrenocortical carcinoma, or pheochromocytoma usually have a normal or low BMI. In line with this statement, in our recent study comparing 76 pheochromocytomas and 56 patients with adrenal cortical adenomas with ACS and non-functioning adrenal adenomas, we found that BMI was significantly lower in the first group (24.4±5.7 vs. 26.9±4.3kg/m2, P=0.006).15 Lower BMI is also expected in patients with malignant disease such as adrenocortical carcinoma, in relation to the catabolic effect of the tumor itself.
In addition, we observed that all 6 patients with bilateral tumors were overweight/obese. This finding could be explained by the theory that insulin is able to promote adrenal growth as recognized by Reincke et al.16 who also refer to a proliferative effect of insulin on an adrenal cancer cell line. Moreover, it could be related to the fact that benign adrenocortical adenomas are more commonly bilateral than pheochromocytoma and adrenocortical carcinoma,17 and benign adrenal tumors are more common in obese/overweight than patients with low/normal weight.
Excess body mass is not only associated with a higher prevalence of metabolic syndrome, which can be associated with a higher risk of surgical complications, but it also makes the surgical procedure more difficult in many cases, with increasing demands on the surgeon.6 In our series, we found a complication rate in obese/overweight patients of 15%; this percentage is in keeping with the range of complication rates of laparoscopic adrenalectomy reported in obese patients in the literature (4.6–32%).18 Moreover, in line with other studies, we found higher rates of postsurgical complications (27.3% vs. 5.7%) and a longer hospital stay (5.4±1.39 vs. 3.5±1.78, P=0.007) in obese compared to nonobese patients. However, no differences were found in intraoperative complications and operative time. These results are in agreement with those described in other studies such as the Dancea et al. series19 that concluded that obesity was associated with increased complications. The conversion rate to open surgery in laparoscopic adrenalectomy may vary from 1 to 22%.20 One of the causes of conversion is obesity, but it may also be caused by uncontrollable bleeding, large masses or invasion of adjacent structures. In our study, there are only 2 cases (1.4%) of conversion to open surgery, but they are not related to obesity in either case.
In contrast with our results, other studies such as the Pedziwiatr et al. study11 found no significant differences in short-term outcomes (operative time, blood loss, conversion and complication rates, hospital stay, or readmissions) between normal weight, overweight, obese, and morbidly obese patients. These differences may be related to the different study design, the included study population (patients with or without malignant adrenal tumors), and the definitions employed for obesity and surgical complications, that are not always the same.
Other studies have reported that surgical complications were higher in patients with ASA grade>2, previous abdominal surgery, obesity, diabetes, and larger tumor size.21 In this vein, in our series, the multivariate analysis showed that obesity, age, ASA>2, and tumor size were independent risk factors for postoperative complications; with obesity being the most important factor, with an OR of 23.3 in comparison with non-obese patients. Despite a higher rate of surgical complications in obese patients, laparoscopic adrenalectomy should also be considered the technique of choice in these patients.11 In addition, other authors state that age ≥70 years, ASA≥3, BMI≥35kg/m2, tumor≥6cm, and previous upper abdominal surgery should not be considered contraindications for laparoscopic adrenalectomy,20 since they found that the only independent predictive factors in the multivariable logistic regression analysis for overall complications were conversion to open surgery (OR 6.2) and left-sided laparoscopic adrenalectomy (OR 1.89). In accordance with this study, despite our having found a higher rate of complications in obese compared to non-obese patients, we believe that with adequate experience, laparoscopic adrenalectomy can be a feasible and safe technique in obese patients.
We are aware that our study has several limitations. Firstly, the main limitation is the retrospective nature of study. However, the inclusion of the patients was consecutive, reducing the possibility of selection biases. Secondly, the study was carried out in a single center that is considered a reference center for the management of adrenal tumors, with a high volume of adrenalectomies per year, so our results are probably not representative of other centers with a lower number of adrenalectomies and with less complex cases. Moreover, our series included patients with different etiologies of adrenal tumors, and although we did not find differences in the etiology of these tumors depending on weight status, it is possible that some specific types of tumors are more common in patients with overweight/obesity, like Cushing's syndrome and ACS.21 In addition, it would have been interesting to have information about waist circumference to determine the prevalence of visceral obesity, since it is possible that the association of waist circumference with intraoperative and postoperative complications was even higher than those we have obtained, even in overweight patients.22 In the same vein, we are aware that BMI is an inaccurate marker for estimating overall body composition. Information about the proportion of muscle mass and fat mass would allow us to establish the prevalence of sarcopenic obesity, which is related to a higher rate of complications than non-sarcopenic obesity.23
ConclusionObesity and overweight are common conditions in patients who undergo adrenalectomy. Adrenalectomy is considered a safe procedure in patients with overweight, but it is associated with a higher risk of postsurgical complications and longer hospital stay in obese patients compared to patients with overweight and normal weight. Thus, obesity is an independent risk factor of postsurgical complications that needs to be considered in surgical decisions of adrenalectomy.
Authors’ contributionsCésar Mínguez Ojeda and Marta Araujo-Castro wrote the draft of the manuscript, all authors have reviewed and approved the final version of the article.
Ethical approvalAll procedures performed in the participants of the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was evaluated and approved by the Ethics Committee of Hospital Universitario Ramón y Cajal ((approval date: July 2020, Minutes 395).
Data availability statementThe data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Financial supportSENDIMAD [Sociedad de Endocrinología, Nutrición y Diabetes de la Comunidad de Madrid, Endocrinology, Nutrition and Diabetes Society of the Community of Madrid]: BECA SENDIMAD de Ayuda a la Investigación en Endocrinología, Nutrición y Diabetes 2019 [SENDIMAD GRANT in Support of Research in Endocrinology, Nutrition and Diabetes 2019].
IRYCIS [Instituto Ramón y Cajal de Investigación Sanitaria, Ramón y Cajal Health Research Institute]: Convocatoria intramural de ayudas a proyectos de investigación de investigadores noveles, investigadores clínicos asociados y/o grupos emergentes del Hospital Universitario Ramón y Cajal 2019 [Intramural call for grant applications for research projects by new researchers, clinical research associates and/or emerging groups of Hospital Universitario Ramón y Cajal (Ramón y Cajal University Hospital) 2019].
Conflict of interestThe authors have no conflict of interest.