Malnutrition is a common medical problem in cancer patients with a negative impact on quality of life. The aim of this study was to address different issues related to nutritional management of cancer patients in clinical practice. A multidisciplinary group of experts in Medical Oncology, Pharmacy, and Endocrinology and Nutrition prepared a list of topics related to the nutritional status of cancer patients and grouped them into three blocks: nutritional support, parenteral nutrition (PN), and home PN (HPN). A literature review was made of articles published in Spanish, English and French until April 2017. This consensus emphasizes several key elements that help physicians standardize management of the nutritional status of cancer patients in clinical practice, and establishes common guidelines for indication, monitoring, nutritional requirements, and access routes to PN.
La desnutrición es un problema médico frecuente de los pacientes oncológicos que impacta de forma negativa en la calidad de vida. El objetivo de este trabajo es analizar y dar respuesta a diferentes cuestiones relacionadas con el manejo nutricional de un paciente oncológico en la práctica clínica. Un grupo multidisciplinar de expertos en Oncología Médica, Endocrinología y Nutrición y Farmacia elaboró una lista de temas relacionados con el estado nutricional del paciente oncológico agrupados en 3 bloques: soporte nutricional, nutrición parenteral (NP) y NP domiciliaria (NPD). Se realizó una revisión de la literatura que incluyó artículos publicados en español, inglés y francés hasta abril de 2017. Este consenso destaca diferentes elementos clave que ayudarán a los médicos a normalizar el manejo del estado nutricional del paciente oncológico en la práctica clínica, estableciendo pautas comunes de indicación, monitorización, requerimientos nutricionales y vías de acceso a la NP.
Malnutrition is relatively common in cancer patients, and often has a significant impact on their quality of life. The proportion of patients with weight loss at the time of diagnosis ranges from 15% to 40% depending on the type of cancer. Moreover, the incidence of malnutrition increases as the disease progresses, eventually affecting up to 80% of patients.1–3
Malnutrition has a negative impact on the course of patients with cancer, increasing the incidence of infections, hospital stay, and the risk of mortality.3,4
Despite this, limited information is available on the nutritional recommendations that should be implemented, and there are still a number of doubts concerning the nutritional management of patients with cancer in standard clinical practice.
In order to answer the questions faced by oncologists as regards the nutritional management of cancer patients, a consensus document has been prepared to provide specialists responsible for the nutritional management of those patients with a reference framework based on the available scientific evidence and the clinical experience of the group.
MethodsA multidisciplinary group consisting of specialists in medical oncology, endocrinology and nutrition, and pharmacy jointly prepared a consensus document on the various aspects that affect the nutritional status and treatment of cancer patients (available at: http://www.seen.es/herramientasClinicas/guias/seen/guiaSeen.aspx). An executive summary of this document is provided here. A literature review was made in the MEDLINE database, through the Pubmed supplier, of all articles published in Spanish, English, and French up to April 2017.
The document was structured as a questionnaire and contained all the questions which, in the opinion of the panel members, could give rise to controversy or doubts.
The different aspects on which the panel focused its attention were: (1) nutritional support in cancer patients; (2) parenteral nutrition (PN) in cancer patients; and (3) home parenteral nutrition (HPN) in cancer patients.
ResultsWhat is the incidence of malnutrition in the different types of neoplastic disease and oncological treatments?The incidence of malnutrition varies, depending on the type and stage of the tumor. By type of tumor, the prevalence of malnutrition is 80% in pancreatic cancer, 48–61% in lymphomas of poor prognosis and colorectal cancer, up to 46% in urological and pulmonary tumors, and 30–40% in lymphomas of good prognosis, breast cancer, and sarcoma.3–5 By stage, malnutrition is found in up to 15–20% of early stages, in 80% of patients with advanced disease, and in 80–90% of cases with terminal disease.3–5 The Spanish study NUPAC6 confirmed moderate to severe malnutrition rates of 52%, 57.7% in esophageal cancer, 50% in gastric cancer, 47.1% in laryngeal cancer, and 17.6% in prostate cancer.
The PREDyCES® study found an impact of malnutrition on hospital stay and costs, with a mean increase in the length of stay of 3–4 days in malnourished as compared to well-nourished patients and a 20–25% increase in the costs associated with hospitalization.7
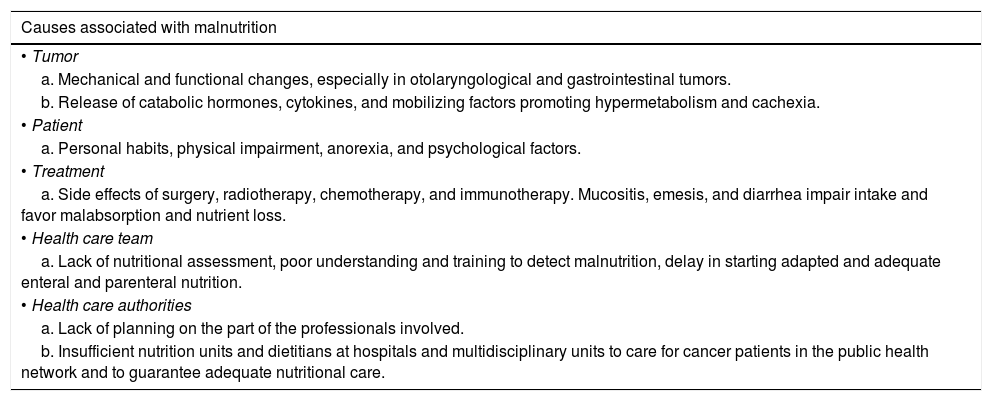
How does cancer influence the nutritional status of patients?There are multiple causes associated with malnutrition in cancer patients (Table 1).
Different causes associated with malnutrition in cancer patients.
| Causes associated with malnutrition |
|---|
| • Tumor |
| a. Mechanical and functional changes, especially in otolaryngological and gastrointestinal tumors. |
| b. Release of catabolic hormones, cytokines, and mobilizing factors promoting hypermetabolism and cachexia. |
| • Patient |
| a. Personal habits, physical impairment, anorexia, and psychological factors. |
| • Treatment |
| a. Side effects of surgery, radiotherapy, chemotherapy, and immunotherapy. Mucositis, emesis, and diarrhea impair intake and favor malabsorption and nutrient loss. |
| • Health care team |
| a. Lack of nutritional assessment, poor understanding and training to detect malnutrition, delay in starting adapted and adequate enteral and parenteral nutrition. |
| • Health care authorities |
| a. Lack of planning on the part of the professionals involved. |
| b. Insufficient nutrition units and dietitians at hospitals and multidisciplinary units to care for cancer patients in the public health network and to guarantee adequate nutritional care. |
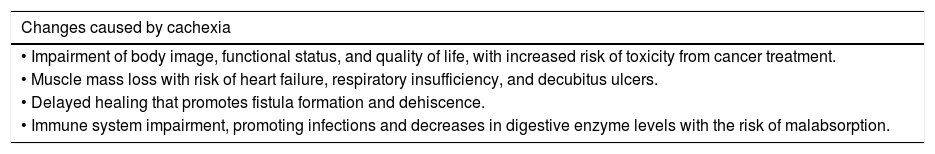
The cachexia associated with cancer causes various changes8 (Table 2). Cachexia and malnutrition have a negative impact on prognosis and are associated with up to 30% of deaths from cancer.1–3,9,10 In addition, weight losses greater that 5% before diagnosis and the start of cancer treatment predicted for early mortality irrespective of stage, histology, and general status.11
Changes related to cancer-associated cachexia.
| Changes caused by cachexia |
|---|
| • Impairment of body image, functional status, and quality of life, with increased risk of toxicity from cancer treatment. |
| • Muscle mass loss with risk of heart failure, respiratory insufficiency, and decubitus ulcers. |
| • Delayed healing that promotes fistula formation and dehiscence. |
| • Immune system impairment, promoting infections and decreases in digestive enzyme levels with the risk of malabsorption. |
Source: Adapted from Tisdale.8
A nutritional assessment is recommended in all cancer patients at diagnosis and during treatment in order to detect patients malnourished or at nutritional risk and to implement early intervention, because late diagnosis may impair recovery and weight gain.12
The 2017 guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN)13 recommend the regular assessment of nutritional intake, weight changes, and the body mass index (BMI) after a diagnosis of cancer. Assessments should be repeated depending on the stability of the patient's clinical condition.
Among the multiple tools available for nutritional screening, the most widely recommended are the 2002 Nutritional Risk Screening (NRS 2002) system for inpatients, the Malnutrition Universal Screening Tool (MUST) for the general population, and the Mini Nutritional Assessment Short Form (MNA-SF) for elderly patients. The Malnutrition Screening Tool (MST) is a simple screening method that has been validated for cancer patients.
The Patient-Generated Subjective Global Assessment (PG-SGA) tool is the gold standard method to assess the nutritional status of cancer patients.14 The PG-SGA classifies patients into three groups: A, normally nourished; B, nutritional risk or moderate malnutrition; and C, severe malnutrition.14
What parameters (clinical, laboratory, and anthropometric) should be taken into account in assessing initial nutritional status and during follow-up of cancer patients?There is no single parameter that provides information regarding nutritional status; instead, a combination of several parameters (clinical, laboratory, anthropometric, and functional) should be used.
The ESPEN13 guidelines recommend the assessment of nutritional intake using a dietary survey, muscle mass evaluation by dual-energy X-ray absorptiometry (DEXA), bioimpedance analysis (BIA), or CT scan, and the assessment of physical performance using various scales such as the ECOG and Karnofsky scales, dynamometry, gait speed, etc.13 As regards laboratory parameters, the ESPEN guidelines recommend the use of serum C-reactive protein (CRP) and albumin levels to measure systemic inflammation.13
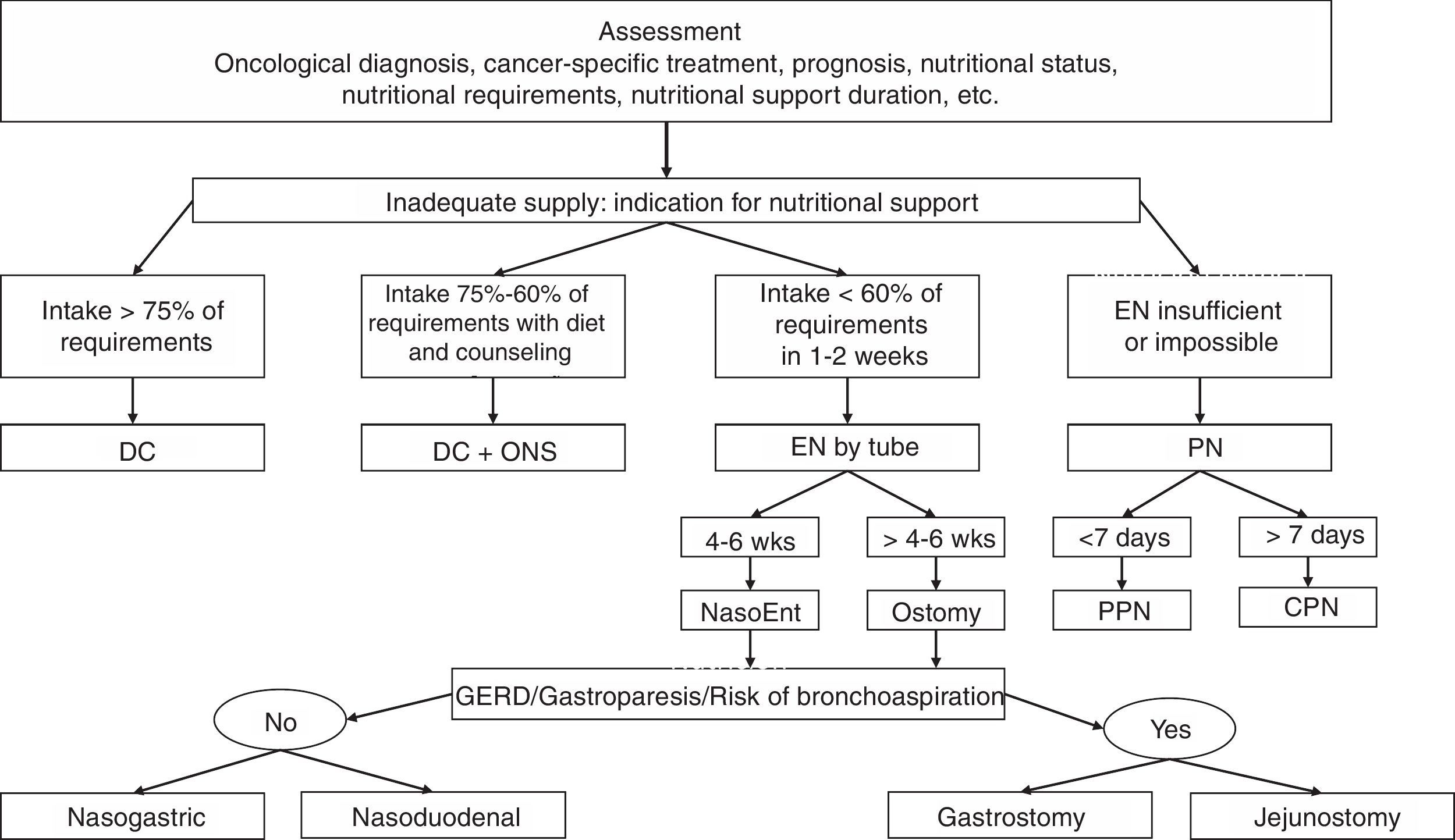
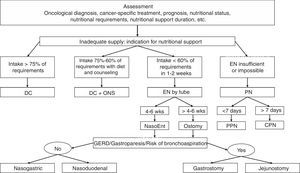
What are the objectives and indications of the different types of specialized nutritional support in cancer patients?The choice depends on the patient's current status: oncological diagnosis, cancer-specific treatment, prognosis, nutritional status, nutritional requirements, and the duration of nutritional support.13,14Fig. 1 shows the nutritional support algorithm.
Nutritional support algorithm.
DC: diet counseling; GERD: gastroesophageal reflux disease; NasoEnt: nasoenteral; EN: enteral nutrition; NP: parenteral nutrition; CPN: central parenteral nutrition; PPN: peripheral parenteral nutrition; wks: weeks; ONS: oral nutritional supplements.
Source: Adapted from Hernández et al.42
If oral food intake is inadequate, starting enteral nutrition is recommended.13–15 If enteral supply is not sufficient or possible, PN should be started.13,14
Cancer patients are prescribed nutritional support when they are malnourished or are not expected to be able to take food for one week or longer, or if their intake is less than 60% of that required for more than 10 days (grade of recommendation C).13
What are the nutritional requirements of cancer patients?In principle, if individualized measurements (indirect calorimetry) are not made, the energy requirements of cancer patients should be considered similar to those of healthy people (25–30kcal/kg/day).13
Protein requirements should range from 1 (minimum) to 1.2–1.5g/kg/day, and may be increased to 2g/kg/day if very high protein catabolism exists.13
The recommended ratio of energy expenditure to nitrogen requirements ranges from 130–100kcal/gN.14,16
The water and sodium requirements of patients also need to be taken into consideration. They should be decreased below the normal amounts.13
Are there specific nutrients with an impact on the course of cancer?Glutamine (oral and parenteral) has been the amino acid most widely researched in recent decades, but no adequate clinical data are available to support the recommendation of glutamine for preventing enteritis and mucositis induced by radiotherapy and chemotherapy.13,14,16,17
Other nutrients tested, such as branched chain amino acids, amino acid metabolites such as hydroxymethylbutyrate (HMB), leucine, vitamin D or probiotics, have given inconclusive results.13,14
When is parenteral nutrition indicated in a patient with cancer?PN is mainly indicated in cancer patients as a specific nutritional support modality when the use of the gastrointestinal tract is not possible and/or oral and/or enteral nutrition is not sufficient or possible13–15,18:
- A.
Because gastrointestinal tract access is contraindicated.
- B.
Because gastrointestinal tract access is not possible.
- C.
Because the gastrointestinal tract is ineffective.
- D.
Due to low oral and/or enteral supply.
When the estimated survival is longer than 1–3 months, and if intestinal insufficiency exists, PN may be offered if the oral/enteral routes are inadequate, there are expectations of improving quality of life and function of the patient, and at the express wish of the patient.13
What are the indications for supplemental parenteral nutrition in cancer patients?PN supplemental to inadequate oral or enteral support is indicated when a clear improvement is foreseen in the nutritional status or the quality of life of the cancer patient.13,14,19 Long-term PN is recommended for patients with severe radiation-induced mucositis or enteritis (grade of recommendation C).20
The composition of PN will depend on the supplementation needed by each patient.13,14
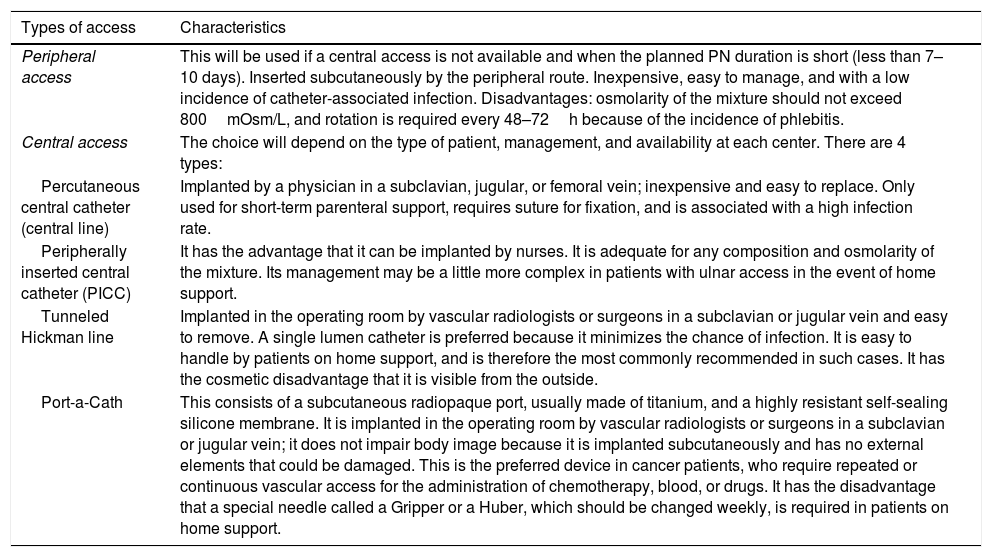
What are the different administration routes of parenteral nutrition in cancer patients?The administration routes of PN are the same in cancer patients as in all other patients (Table 3).
Different administration routes of parenteral nutrition in cancer patients.
| Types of access | Characteristics |
|---|---|
| Peripheral access | This will be used if a central access is not available and when the planned PN duration is short (less than 7–10 days). Inserted subcutaneously by the peripheral route. Inexpensive, easy to manage, and with a low incidence of catheter-associated infection. Disadvantages: osmolarity of the mixture should not exceed 800mOsm/L, and rotation is required every 48–72h because of the incidence of phlebitis. |
| Central access | The choice will depend on the type of patient, management, and availability at each center. There are 4 types: |
| Percutaneous central catheter (central line) | Implanted by a physician in a subclavian, jugular, or femoral vein; inexpensive and easy to replace. Only used for short-term parenteral support, requires suture for fixation, and is associated with a high infection rate. |
| Peripherally inserted central catheter (PICC) | It has the advantage that it can be implanted by nurses. It is adequate for any composition and osmolarity of the mixture. Its management may be a little more complex in patients with ulnar access in the event of home support. |
| Tunneled Hickman line | Implanted in the operating room by vascular radiologists or surgeons in a subclavian or jugular vein and easy to remove. A single lumen catheter is preferred because it minimizes the chance of infection. It is easy to handle by patients on home support, and is therefore the most commonly recommended in such cases. It has the cosmetic disadvantage that it is visible from the outside. |
| Port-a-Cath | This consists of a subcutaneous radiopaque port, usually made of titanium, and a highly resistant self-sealing silicone membrane. It is implanted in the operating room by vascular radiologists or surgeons in a subclavian or jugular vein; it does not impair body image because it is implanted subcutaneously and has no external elements that could be damaged. This is the preferred device in cancer patients, who require repeated or continuous vascular access for the administration of chemotherapy, blood, or drugs. It has the disadvantage that a special needle called a Gripper or a Huber, which should be changed weekly, is required in patients on home support. |
Source: Adapted from Derenski et al.21
Nutritional monitoring of cancer patients should be multidisciplinary and adapted to the characteristics of each center.
Nutritional screening should be included in the routine care of cancer patients and should be easy to perform by any member of the care team, either nursing staff or physicians.13
Monitoring of cancer patients with HNP is also multidisciplinary.
When is the discontinuation of parenteral nutrition indicated in cancer patients?PN should be discontinued when the objectives sought in each patient are achieved and when one of the following occurs:
What are the objectives of home parenteral nutrition in cancer patients?The specific goals of HPN in cancer patients are to prevent and treat malnutrition and/or cachexia, to improve compliance with the prescribed cancer treatment, reducing its interruptions, to decrease the adverse effects of treatment, and to improve patient quality of life (grade of recommendation C).13,20
It is recommended that, in addition to having metabolic stability, at hospital discharge patients should have received adequate training, have access to safe material resources required for HPN, are physically and emotionally able to manage HPN, and have an adequate home environment.30,31
A multidisciplinary team experienced in HPN and a physician-nurse team for home support should also be available.32
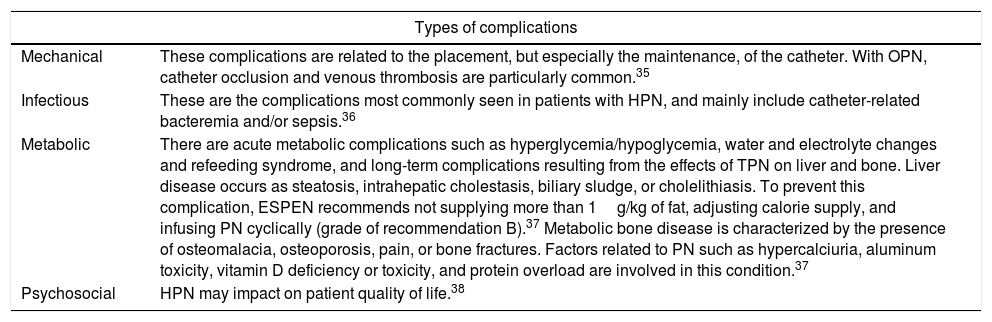
What are the complications of home parenteral nutritional in cancer patients?These comprise four major groups: mechanical, infectious, metabolic, and psychosocial complications34,35 (Table 4).
Complications of home parenteral nutritional (HPN) in cancer patients.
| Types of complications | |
|---|---|
| Mechanical | These complications are related to the placement, but especially the maintenance, of the catheter. With OPN, catheter occlusion and venous thrombosis are particularly common.35 |
| Infectious | These are the complications most commonly seen in patients with HPN, and mainly include catheter-related bacteremia and/or sepsis.36 |
| Metabolic | There are acute metabolic complications such as hyperglycemia/hypoglycemia, water and electrolyte changes and refeeding syndrome, and long-term complications resulting from the effects of TPN on liver and bone. Liver disease occurs as steatosis, intrahepatic cholestasis, biliary sludge, or cholelithiasis. To prevent this complication, ESPEN recommends not supplying more than 1g/kg of fat, adjusting calorie supply, and infusing PN cyclically (grade of recommendation B).37 Metabolic bone disease is characterized by the presence of osteomalacia, osteoporosis, pain, or bone fractures. Factors related to PN such as hypercalciuria, aluminum toxicity, vitamin D deficiency or toxicity, and protein overload are involved in this condition.37 |
| Psychosocial | HPN may impact on patient quality of life.38 |
Patients on HPN require close, individualized monitoring for treatment efficacy and safety to be assessed, and in order that any complications associated with this treatment can be detected and resolved.39,40
Monitoring should be performed by the team of professionals who prescribed HPN, usually the nutrition unit of the reference hospital, in coordination with the medical team responsible for monitoring the course of the patient.41
What information sources are available to improve our understanding of the importance to nutritional support in cancer patients?Many diverse information sources are available, including original studies, systematic reviews, etc.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Ocón Bretón MJ, Luengo Pérez LM, Virizuela JA, Álvarez Hernández J, Jiménez Fonseca P, Cervera Peris M, et al. Soporte nutricional y nutrición parenteral en el paciente oncológico: informe de consenso de un grupo de expertos. Endocrinol Diabetes Nutr. 2018;65:17–23.