Resident physicians’ proper use of nutritional support and knowledge about Clinical Nutrition is essential to ensuring that their patients receive suitable nutritional care.
Materials and methodAn online survey was sent to resident physicians at our hospital in specialisations with hospital beds. The survey featured 20 multiple-choice questions scored from 1 to 10 (1 being “completely disagree” and 10 being “completely agree”) across the following themes: nutritional assessment, diets, oral nutritional supplements, enteral nutrition and perception of the Nutrition Unit.
ResultsThe survey was completed by 69% of resident physicians in medical specialisations and 70% of those in surgical specialisations. Overall, the average survey score was 6.28, with higher scores among medical residents than surgical residents (6.86 versus 5.38; p < 0.001), especially in the sections on nutritional assessment, diets and oral nutritional supplements. The respondents had a positive perception of the Nutrition Unit (mean score 7.6).
DiscussionResidents in medical specialisations afford greater importance to their patients’ nutrition than residents in surgical specialisations, although in both groups the average score was rather low. There is much room for improvement in the training in Clinical Nutrition of this group, and it is important to include topics in Clinical Nutrition in training programmes for all residents in hospital specialisations.
La correcta aplicación del soporte nutricional y el conocimiento sobre Nutrición Clínica de los médicos internos residentes (MIR) de un hospital son fundamentales para garantizar una adecuada atención nutricional en los pacientes.
Material y métodoSe envió una encuesta online a todos los MIR de nuestro centro, cuyas especialidades poseen camas de hospitalización. El cuestionario incluía 20 preguntas de elección múltiple puntuadas del 1 al 10 (1 totalmente en desacuerdo y 10 totalmente de acuerdo), distribuidas en estas materias: valoración nutricional, dietas, suplementos nutricionales orales, nutrición enteral y percepción de la Unidad de Nutrición.
ResultadosContestó el 69% de MIR de especialidades médicas y 70% de quirúrgicas. En el conjunto de la encuesta, la puntuación de todos los MIR fue de 6,28 siendo mayor en los de especialidades médicas que en los de especialidades quirúrgicas (6,86 vs. 5,38; p < 0,001), destacando especialmente la superioridad de puntuación de MIR de médicas vs. quirúrgicas en los apartados de valoración nutricional, dietas y suplementos nutricionales orales. La percepción de la Unidad de Nutrición fue positiva para los encuestados (puntuación media 7,6).
DiscusiónLos residentes de especialidades médicas dan mayor importancia a la nutrición de los pacientes hospitalizados que los de especialidades quirúrgicas, sin embargo, las medias de puntuación fueron bajas en todos los casos. Existen oportunidades de mejora en la formación en Nutrición Clínica de este colectivo, y sería importante incluir en los programas formativos de todos los MIR de especialidades hospitalarias aspectos sobre Nutrición Clínica.
Undernutrition is a problem with a high prevalence in hospital settings, since one out of every four patients in Spanish hospitals is undernourished or at nutritional risk, as revealed by the Prevalencia de la desnutrición hospitalaria y costes asociados en España [Prevalence of Hospital Undernutrition and Associated Costs in Spain] (PREDyCES) study.1 This study evaluated the prevalence of undernutrition/nutritional risk in Spanish hospitals, on admission and on discharge, through nutritional screening. In addition, this condition was seen to be related to an excessively long hospital stay and an increase in associated costs, especially in patients undernourished during admission.
The importance of nutrition in general, and undernutrition and the treatment thereof in particular, at a hospital makes plain the importance of knowledge of undernutrition among physicians in hospital settings.
Resident physicians are essential in hospital care. There is very close contact between the physician in training and the patient, and residents’ perceptions about certain clinical aspects of patients that are not directly related to the patients’ reason for admission could influence the management of hospitalised patients. Basic knowledge of hospital Clinical Nutrition offers a clear example of this.
There are precedents in the evaluation of resident physicians’ perceptions of the management of diabetes mellitus in hospitalised patients.2 However, the same is not true of hospital Clinical Nutrition, since no studies have evaluated the perception of basic knowledge of hospital Clinical Nutrition among resident physicians at a hospital, with the exception of residents in endocrinology and nutrition,3–5 as well as the Intensive Care Unit.6
Thus, the objective of our study was to evaluate resident physicians’ perceptions of basic knowledge of hospital Clinical Nutrition at a university tertiary hospital.
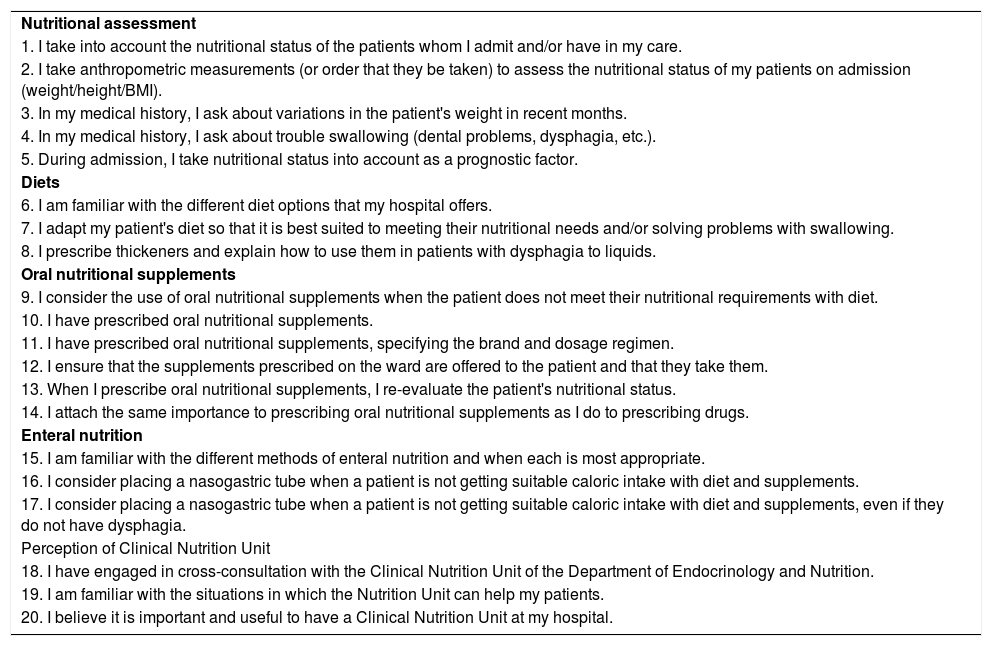
Materials and methodsAn online survey was sent out between November 2019 and January 2020 to resident physicians at the Complejo Hospitalario Universitario de Albacete [Albacete University Hospital Complex] whose specialisations, whether medical or surgical, had hospital beds. The questionnaire included 20 statements that could be scored from 1 to 10, where 1 meant “completely disagree” and 10 meant “completely agree”, distributed across five subjects: nutritional assessment, diets, oral nutritional supplements, enteral nutrition and perception of the Clinical Nutrition Unit (Table 1). A section on parenteral nutrition was not included, since at our centre, save for Intensive Care Unit physicians, only physicians and residents in the Department of Endocrinology and Nutrition prescribe and adjust parenteral nutrition.
List of survey questions.
| Nutritional assessment |
| 1. I take into account the nutritional status of the patients whom I admit and/or have in my care. |
| 2. I take anthropometric measurements (or order that they be taken) to assess the nutritional status of my patients on admission (weight/height/BMI). |
| 3. In my medical history, I ask about variations in the patient's weight in recent months. |
| 4. In my medical history, I ask about trouble swallowing (dental problems, dysphagia, etc.). |
| 5. During admission, I take nutritional status into account as a prognostic factor. |
| Diets |
| 6. I am familiar with the different diet options that my hospital offers. |
| 7. I adapt my patient's diet so that it is best suited to meeting their nutritional needs and/or solving problems with swallowing. |
| 8. I prescribe thickeners and explain how to use them in patients with dysphagia to liquids. |
| Oral nutritional supplements |
| 9. I consider the use of oral nutritional supplements when the patient does not meet their nutritional requirements with diet. |
| 10. I have prescribed oral nutritional supplements. |
| 11. I have prescribed oral nutritional supplements, specifying the brand and dosage regimen. |
| 12. I ensure that the supplements prescribed on the ward are offered to the patient and that they take them. |
| 13. When I prescribe oral nutritional supplements, I re-evaluate the patient's nutritional status. |
| 14. I attach the same importance to prescribing oral nutritional supplements as I do to prescribing drugs. |
| Enteral nutrition |
| 15. I am familiar with the different methods of enteral nutrition and when each is most appropriate. |
| 16. I consider placing a nasogastric tube when a patient is not getting suitable caloric intake with diet and supplements. |
| 17. I consider placing a nasogastric tube when a patient is not getting suitable caloric intake with diet and supplements, even if they do not have dysphagia. |
| Perception of Clinical Nutrition Unit |
| 18. I have engaged in cross-consultation with the Clinical Nutrition Unit of the Department of Endocrinology and Nutrition. |
| 19. I am familiar with the situations in which the Nutrition Unit can help my patients. |
| 20. I believe it is important and useful to have a Clinical Nutrition Unit at my hospital. |
The nutritional assessment section included perception of the importance of the nutritional status of patients on admission and its significance as a prognostic factor, recording of anthropometric measures on admission to assess nutritional status, and investigation of the presence or absence of weight loss in recent months and dysphagia.
On the subject of diets, the residents were asked about their knowledge of the hospital diet code; prescribing a diet adapted to the patient's needs and clinical situation; and, in the specific case of dysphagia, prescribing thickeners.
Regarding nutritional supplements, whether residents prescribed oral nutritional supplements when diet was insufficient and, if so, whether this prescription was made specifying the brand and dosage regimen were evaluated. In addition, efforts made by responsible physicians to determine patients’ adherence to treatment and re-evaluate their nutritional status after providing this nutritional support was assessed. The importance assigned by the residents to the use of nutritional supplements and whether they considered prescribing nutritional supplements of equal value to prescribing drugs were scored as well.
In enteral nutrition, sections such as perception of knowledge about the variety of non-oral enteral nutrition methods and when to use each of them were included.
Finally, the hospital residents’ assessment of the Clinical Nutrition Unit, its usefulness and access to the unit figured in the survey.
A statistical analysis of the scores obtained for each question was performed by calculating mean and standard deviation, both for the group as a whole and for each subgroup (medical and surgical), and analysing whether the difference between the scores for these two groups was statistically significant using Student’s t test. In addition, for each question, the existence of a correlation between the score assigned by the resident physician and their year of residency at the time of their participation in the study was analysed by the Pearson correlation test. The p value was adjusted for multiple comparisons and a p < 0.05 was considered statistically significant.
Statistical analysis was performed using the R software programme, version 4.0.2, in the RStudio integrated development environment (RStudio Team [2020]. RStudio: Integrated Development for R. RStudio, PBC, Boston, MA. URL: http://rstudio.com).
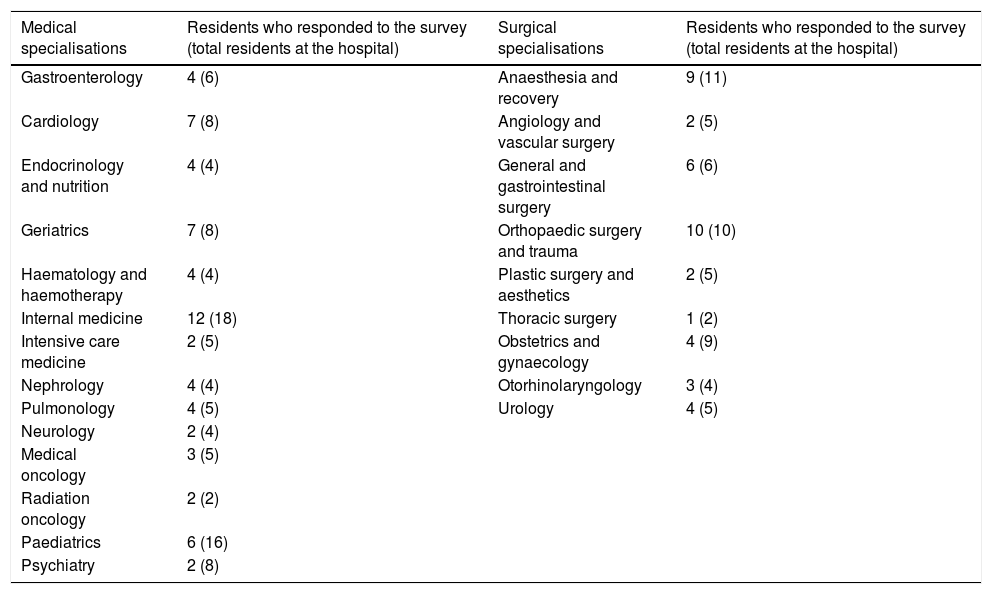
ResultsA total of 154 surveys were sent out, and 104 (68%) were completed. Of those resident physicians who completed the survey, 63 belonged to medical specialisations (69% of all medical residents at our hospital) and 41 belonged to surgical specialisations (70% of all surgical residents at our hospital) (Table 2). By year of residency, 26% were first-year residents, 29% were second-year residents, 20% were in their third year and 20% were in their fourth year. Just 5% of the survey respondents were fifth-year residents.
Distribution of survey respondents by specialization.
| Medical specialisations | Residents who responded to the survey (total residents at the hospital) | Surgical specialisations | Residents who responded to the survey (total residents at the hospital) |
|---|---|---|---|
| Gastroenterology | 4 (6) | Anaesthesia and recovery | 9 (11) |
| Cardiology | 7 (8) | Angiology and vascular surgery | 2 (5) |
| Endocrinology and nutrition | 4 (4) | General and gastrointestinal surgery | 6 (6) |
| Geriatrics | 7 (8) | Orthopaedic surgery and trauma | 10 (10) |
| Haematology and haemotherapy | 4 (4) | Plastic surgery and aesthetics | 2 (5) |
| Internal medicine | 12 (18) | Thoracic surgery | 1 (2) |
| Intensive care medicine | 2 (5) | Obstetrics and gynaecology | 4 (9) |
| Nephrology | 4 (4) | Otorhinolaryngology | 3 (4) |
| Pulmonology | 4 (5) | Urology | 4 (5) |
| Neurology | 2 (4) | ||
| Medical oncology | 3 (5) | ||
| Radiation oncology | 2 (2) | ||
| Paediatrics | 6 (16) | ||
| Psychiatry | 2 (8) |
The total number of residents from each specialisation is specified in brackets.
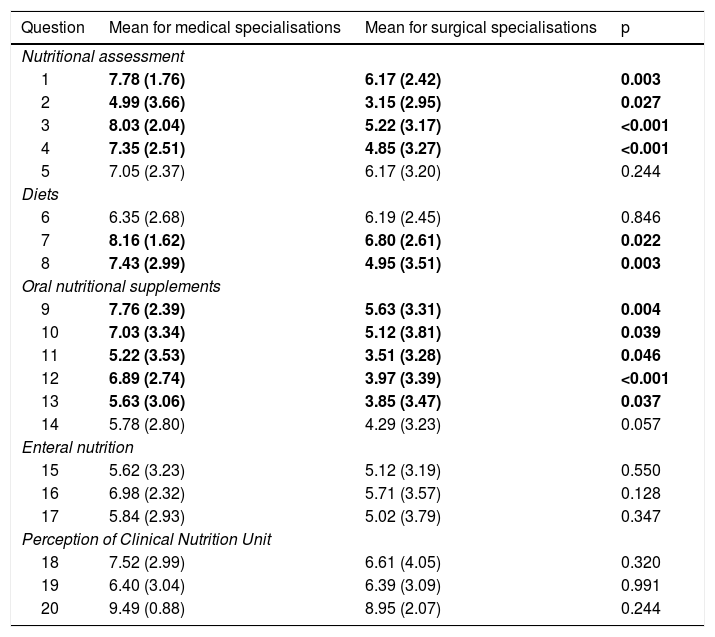
The mean score on the survey for all the residents was 6.28 points; notably, the mean score on the questions was significantly higher in the group of medical residents (6.86) versus the group of surgical residents (5.38) (p < 0.001). Table 3 shows the mean and standard deviation for the score assigned to each question by the medical and surgical residents.
Means and standard deviation of scores on each question for the medical specialisation group versus the surgical specialisation group.
| Question | Mean for medical specialisations | Mean for surgical specialisations | p |
|---|---|---|---|
| Nutritional assessment | |||
| 1 | 7.78 (1.76) | 6.17 (2.42) | 0.003 |
| 2 | 4.99 (3.66) | 3.15 (2.95) | 0.027 |
| 3 | 8.03 (2.04) | 5.22 (3.17) | <0.001 |
| 4 | 7.35 (2.51) | 4.85 (3.27) | <0.001 |
| 5 | 7.05 (2.37) | 6.17 (3.20) | 0.244 |
| Diets | |||
| 6 | 6.35 (2.68) | 6.19 (2.45) | 0.846 |
| 7 | 8.16 (1.62) | 6.80 (2.61) | 0.022 |
| 8 | 7.43 (2.99) | 4.95 (3.51) | 0.003 |
| Oral nutritional supplements | |||
| 9 | 7.76 (2.39) | 5.63 (3.31) | 0.004 |
| 10 | 7.03 (3.34) | 5.12 (3.81) | 0.039 |
| 11 | 5.22 (3.53) | 3.51 (3.28) | 0.046 |
| 12 | 6.89 (2.74) | 3.97 (3.39) | <0.001 |
| 13 | 5.63 (3.06) | 3.85 (3.47) | 0.037 |
| 14 | 5.78 (2.80) | 4.29 (3.23) | 0.057 |
| Enteral nutrition | |||
| 15 | 5.62 (3.23) | 5.12 (3.19) | 0.550 |
| 16 | 6.98 (2.32) | 5.71 (3.57) | 0.128 |
| 17 | 5.84 (2.93) | 5.02 (3.79) | 0.347 |
| Perception of Clinical Nutrition Unit | |||
| 18 | 7.52 (2.99) | 6.61 (4.05) | 0.320 |
| 19 | 6.40 (3.04) | 6.39 (3.09) | 0.991 |
| 20 | 9.49 (0.88) | 8.95 (2.07) | 0.244 |
Significant results (p < 0.05) are shown in bold.
The mean score for all the residents on the nutritional assessment section was 6.27 points. A statistically significant number of medical resident physicians stated that they more often paid attention to patients' nutritional status; recording of anthropometric measurements; and investigation of problems with swallowing on admission, as well as weight variation in the months prior to admission, compared to surgical residents.
In the diets area, the overall mean was 6.78; with medical residents stating more often than their surgical counterparts that they adapted diets to patients' characteristics and more often prescribed and explained the use of thickeners in patients with dysphagia.
On the subject of oral nutritional supplements, the mean score for the entire sample of residents was 5.59. However, with respect to prescribing nutritional supplements, specifying the brand and dosage regimen, the results were superior among medical residents, who furthermore stated that they ensured patients’ adherence to treatment and re-evaluated nutritional their status after prescribing nutritional supplements more often than surgical residents.
With respect to enteral nutrition, the mean for the group as a whole was 5.8 points.
The assessment of the staff in training of the Clinical Nutrition Unit was the highest score on the questionnaire, with a mean of 7.6. When the medical residents’ score was compared to the surgical residents’, no statistically significant differences were seen on the items corresponding to enteral nutrition and perception of the Clinical Nutrition Unit.
In addition, no statistically significant differences were found when the responses were analysed taking into account year of residence at the time of the survey, regardless of specialisation.
DiscussionOur results showed that attitudes and perceptions among hospital residents could be improved. This was true regardless of the number of years of residency completed; however, there were differences by specialisation group; notable among them was the greater importance attached to nutrition by professionals from medical disciplines compared to surgical ones. At the time when the study was conducted, only endocrinology and nutrition residents rotated through the Clinical Nutrition Unit; therefore, a statistical analysis based on whether or not the physician in training had previously rotated through the Clinical Nutrition Unit could not be performed.
At a statistically significantly higher rate, medical residents stated that they conducted nutritional assessments of their patients, adapted diets to patients’ individual characteristics, prescribed thickeners in dysphagia, prescribed oral nutritional supplements, ensured adherence and subsequently re-evaluated nutritional status more often than surgical residents. Despite this, we detected room for improvement in scores for both groups in relation to oral nutritional supplements and enteral nutrition, as well as nutritional assessment. Finally, it should be noted that the highest score for both groups (medical and surgical specialisations) was achieved in the section on perception of the usefulness and importance of the Clinical Nutrition Unit, demonstrating the high opinion of the work done by the staff on this unit for all the other hospital departments. This undoubtedly represents an incentive to maintain the quality and care provided to our patients.
Strikingly, the score on the diets section was comparatively higher than the score on other survey topics, since the perception of training in this subject has historically been rated as lacking, even among endocrinology residents, for whom nutrition is an integral part of training.5 Moreover, the Clinical Nutrition Unit team has a subjective perception that there are major opportunities for improvement in hospital diet prescription by the different departments. This might have been due to the fact that the questions in our survey evaluated knowledge of (in this case) diets according to resident physicians’ impressions, not knowledge per se, with these resident physicians believing that they had a better command of this aspect of hospital treatment than they really did.
A Likert scale was used. This is the most commonly used type of scale in research in the social sciences and education, and the most accurate in the study of population attitudes, opinions and perceptions. This improved the sensitivity of the scale and facilitated comparison of the results, both to other population groups and to the same sample in the future. In addition, the use of a numerical scale avoided bias and increased the accuracy of the responses, unlike the use of a categorical scale.7
The general results of the survey supported the findings of other studies, however few in number, that have pointed to room for improvement in resident physicians’ training in nutrition. In Spain, most survey studies of nutrition aimed at this group were conducted with the objective of analysing the country's resident physician training programme, and therefore included residents from departments of endocrinology and nutrition.3–5 Those studies found a gradual improvement over time in resident physicians' assessment of the extent of the training received in this subject, but with gaps in some areas such as dietetics. Outside of this group, the degree of knowledge of Clinical Nutrition has been evaluated only in intensive care unit physicians, both attending and resident,6 with the findings pointing to incomplete training and insufficient knowledge of nutrition in critically ill patients, especially among residents in said departments. Similarly, surveys have been conducted on personal perception of nutritional knowledge in relation to promotion of healthy lifestyles, and as an approach to obesity and diabetes mellitus, in resident physicians in primary care and several hospital departments. However, none of them has focused on undernutrition or artificial nutritional support in hospital settings. All of them found deficiencies in the knowledge of physicians in training in this subject, despite their positive perception of the nutritional approach, both in the clinic and in primary care in general.8–10
Our study surveyed all hospital residents. Notably, surgical residents had a lower assessment in the subject of Clinical Nutrition. This group gradually acquires awareness of the importance of nutrition in surgical patients with the use of protocols for enhanced recovery after surgery (ERAS). Across countless studies and systematic reviews, such protocols have yielded very positive results in terms of recovery and morbidity in surgical patients. Therefore, it is important for all healthcare professionals whose work heavily involves surgical approaches to disease to have a good foundation of knowledge of Clinical Nutrition so that they may make proper use of said protocols. This means that including hospital Clinical Nutrition subjects in their training should be a priority.
This study had a number of limitations, the most significant of which was the fact that the survey evaluated the opinions and perceptions of physicians in training rather than knowledge or clinical practice in relation to hospital Clinical Nutrition. Under such circumstances, biases easily arise, especially in sections more subject to debate such as the above-mentioned diets section. It must be added that, due to this limitation, even though statistically significant differences were found between the two groups of residents, we could not determine whether said differences were significant in daily clinical practice. Another limitation of this study was that it was a single-centre study, rendering extrapolation of the results difficult. Therefore, it would be very interesting to conduct a multicentre study, be it in our region of Spain or at centres elsewhere in the country. Another limitation was that the survey centred solely on resident physicians in hospital specialisations and did not include family and community medicine residents. Such residents comprise the most extensive group of professionals in training and are in close contact with patients and their families and carers. Thus they represent a very important professional group in detecting undernutrition not related to disease as well as following up patients who receive nutritional support and monitoring them for changes over time in nutritional status, as they may be able to identify nutritional problems early and report them to physicians in hospital settings. Despite this, with regard to undernutrition and artificial nutritional support, there are no studies in physicians in training in this specialisation. There are only studies in attending physicians which have demonstrated limited knowledge of enteral nutrition and a great deal of interest on the part of this group in expanding and improving said knowledge.11 It would be useful to broaden the survey to resident physicians in this specialisation in order to gather their opinions and determine the margin for improvement in their knowledge of Clinical Nutrition and nutritional support to improve outpatient care quality. The last limitation was the low number of resident physicians in their final years of residency who took part in this study. However, with the larger volume of residency positions offered in recent years in practically all the specialisations represented in the survey, the number of physicians in later versus earlier years of training was limited, which made it difficult to achieve significant differences between the two groups.
Despite its limitations, the study is novel in that, to our knowledge, it is the only one to date to evaluate perceived knowledge of Clinical Nutrition among resident physicians at a tertiary hospital.
In conclusion, there is a great deal of room for improvement in matters of Clinical Nutrition among physicians in training in hospital settings. This lays bare the importance of reviewing the training plans for the different specialisations and taking a cross-cutting approach to training in this subject.
FundingThis research has not received specific funding from public sector agencies, the commercial sector or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Moya-Moya AJ, López García MC, Sirvent Segovia AE, Jiménez Martínez CM, Ruiz de Assín Valverde A, Madrona Marcos FM, et al. Percepción de conocimiento sobre Nutrición Clínica hospitalaria en los médicos residentes de un hospital terciario. Endocrinol Diabetes Nutr. 2022;69:247–253.