Stroke and type 2 diabetes mellitus (T2DM) are among the leading causes of morbidity and mortality in Europe.
ObjectiveTo describe the vascular risk factors most prevalent in the Spanish population with and without type 2 diabetes mellitus admitted to hospital for a stroke during the 2011–2013 period.
Material and methodsUsing the Spanish Minimum Basic Data Set from 2011 to 2013, a descriptive, observational epidemiological study was conducted comparing the prevalence rates of vascular risk factors in Spanish patients admitted to hospital for stroke. The sample was stratified by the presence or absence of a diagnosis of type 2 diabetes mellitus. Other variables studied included in-hospital mortality, length of hospital stay, and other clinical and sociodemographic variables.
ResultsHypertension was the most prevalent vascular risk factor in all population groups. Female sex, age, and T2DM had a statistically significant association (p<0.05) to hospital mortality in stroke.
ConclusionsHypertension was the most common vascular risk factor in the study sample, followed by hypercholesterolemia. There were no differences in prevalence of hypertension between patients with and without T2DM. However, T2DM is an independent risk factor for hospital mortality in any hospitalization for stroke.
Los accidentes cerebrovasculares (ACV) y la diabetes tipo 2 (DMT2) representan algunas de las principales causas de morbi-mortalidad en Europa.
ObjetivoDescribir los factores de riesgo vascular (FRV) de mayor prevalencia entre la población española con diabetes mellitus tipo 2 y sin diabetes que ha sufrido un ingreso hospitalario relacionado con ACV durante el periodo 2011–2013.
Material y métodoUsando los datos del Conjunto Mínimo Básico de Datos (CMBD) del periodo 2011–2013 se ha realizado un estudio epidemiológico observacional descriptivo comparando las prevalencias de los FRV de la población española hospitalizada por un ACV. La muestra se ha estratificado por la existencia o no de un diagnóstico de DMT2. Otras variables estudiadas han sido: mortalidad intrahospitalaria o MIH, duración de la estancia hospitalaria o EH y otras variables clínicas y sociodemográficas.
ResultadosLa hipertensión resultó el factor de riesgo vascular más prevalente en todos los grupos de población. El sexo femenino, la edad y la DMT2 presentaron una asociación estadísticamente significativa (p<0,05) con la MIH en los ACV.
ConclusionesLa HTA es el FRV más común seguido de la hipercolesterolemia en la muestra estudiada. Existen diferencias significativas entre las prevalencias de la HTA en la población con DMT2 y la población sin DMT2. Además, la DMT2 es un factor independiente de riesgo de la MIH en cualquier caso de hospitalización relacionada con ACV.
According to data published by the Spanish National Statistics Institute (Instituto Nacional de Estadística [INE]) in the 2013 National Morbidity Survey, circulatory disease represents the main cause of hospital admission in the Spanish male population.1 Stroke and cardiovascular complications are the most common causes of admission among the Spanish population with type 2 diabetes mellitus (DM2).2 Furthermore, stroke is one of the leading causes of mortality among the European female population.3
With regard to diabetes, the number of diagnosed cases has increased significantly worldwide according to data provided by government agencies such as the International Diabetes Federation (IDF).4 In Spain, the di@bet.es study reported a prevalence of 14%.5 These data indicate the large number of patients that may be influenced by research findings in DM2 and stroke.
The purpose of this study was to describe the most prevalent vascular risk factors among the Spanish population with and without DM2 undergoing hospital admission related to stroke according to the 2011–2013 admissions registry used in this study. In addition, an analysis was made of the diagnostic and surgical techniques used during hospitalization, as well as of the duration of hospital stay (defined as the period between the date of admission and the date of discharge) and in-hospital mortality (determined as cases where the reason for discharge was stated as “death”) in the two population groups. The influence of the statistically significant variables upon in-hospital mortality was also studied. The Spanish Minimum Basic Data Set on Hospital Discharges (Conjunto Mínimo Básico de Datos de Altas Hospitalarias [CMBD-AH]) was used for the study.
Material and methodsA retrospective, descriptive observational epidemiological study was conducted based on the CMBD-AH provided by the Spanish Ministry of Health, Social Services and Equality (Ministerio de Salud, Servicios Sociales e Igualdad [MSSSI]). This database compiles hospital discharge information compulsorily supplied by 98% of the public and private hospitals in the healthcare system. The database includes demographic data (date of birth, gender), clinical information (14 diagnostic fields and 20 fields referring to procedures performed during hospital admission), and administrative data (date of admission, date of discharge, type of admission, etc.).6
The diagnostic and medical procedure codes were selected based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD 9-CM), which is that used by the CMBD-AH.
Stroke is classified into two major groups according to the underlying etiology: ischemic or hemorrhagic.7 Admissions due to stroke were stratified according to the primary diagnosis into four mutually exclusive groups: ischemic, hemorrhagic, transient ischemic attack and unclassified cases. The diagnostic codes according to the ICD 9-CM used for ischemic events were 433.X and 434.X (with X being a number from 0 to 9), while those used for hemorrhagic events were 430, 431, 432.1 and 432.9. The third group comprised transient ischemic attack (TIA) using codes 435, 435.1, 435.2, 435.3, 435.8 and 435.9. The fourth group (unclassified cases) consisted of “poorly defined” cases (codes: 436, 437, 437.1, 437.2, 437.4, 437.5, 437.6, 437.8, 437.9 and 438.XX). Only the third and fourth groups were considered for the statistical analysis. In addition, the cases were grouped according to the presence or absence of a DM2 diagnosis code in any of the secondary diagnostic fields (codes 250.X0 and 250.X2).
Before statistical analysis, the database was filtered, to remove cases with no birth date, no admission data or no gender specification. Cases in which the primary diagnosis involved conditions with no acute clinical impact were also excluded (codes 437.3 and 437.7). Patients with type 1 diabetes mellitus were removed from the database (codes: 250.X1 and 250.X3), due to their low numerical relevance (<1% of the total data recorded in the database during the study period).
The incidence rates of stroke per 100,000 inhabitants were calculated for each year in both groups (cases with diabetes and without diabetes), based on the INE population as of 31 December for each year of the study period,1 and the prevalence of diabetes was estimated to be 13.8% based on the results of the di@bet.es study.5 The incidence ratio for subjects without diabetes was calculated by taking into account the total number of cases of stroke in the database among the population obtained from the INE corresponding to each year of the study period, after subtracting the estimate of the population with diabetes described in the di@bet.es study. For the population with diabetes, the numerator of the ratio included the number of cases recorded in the database of the population with DM2 and stroke, while the denominator included the percentage of the population obtained from the di@bet.es study with respect to the data from the INE in the time periods not included within the di@bet.es study.
Likewise, an analysis was made of the presence of vascular risk factors (VRFs) such as arterial hypertension (AHT) (ICD-9-CM code: 401, 401.1 and 401.9); hypercholesterolemia (ICD 9-CM code: 272.0); alcohol consumption (ICD 9-CM code: 303.90, 303.91, 303.92 and 303.93); smoking (ICD 9-CM code: 305.1 and v15.82); and obesity (ICD 9-CM code: 278.00 and 278.01). Comorbidities were analyzed, including atrial fibrillation (AF) (ICD 9-CM code: 427.31), carotid stenosis (ICD 9-CM code: 433.1) and intermittent claudication (ICD 9-CM code: 443.9).
The most frequent medical procedures were followed-up on, specifically decompression craniotomy (ICD 9-CM code: 01.24), thrombolysis (ICD 9-CM code: 99.10), computed axial tomography of the skull (brain CT) (ICD 9-CM code: 87.03), magnetic resonance imaging of the brain (brain MRI) (ICD 9-CM code: 88.91) and cerebral arteriography (ICD 9-CM code: 88.41).
The anonymity of the database was maintained, and approval of the study by the Ethics Committee of Hospital Virgen de la Salud (Toledo, Spain) was not required.
Statistical analysisA descriptive statistical analysis was made of the continuous and categorical variables. The data obtained were stratified according to the presence or absence of a diagnosis of diabetes and the type of stroke (ischemic, hemorrhagic, transient ischemic attack and “poorly defined”). In the case of continuous variables, the mean was calculated with its standard deviation (SD) and the median with the interquartile range (IQR). Categorical variables were described by proportions. A bivariate analysis was performed using the Pearson chi-squared test for evaluating possible associations between qualitative variables. A multivariate analysis was performed using in-hospital mortality (IHM) as a dependent dichotomic variable (yes or no) and the following factors as independent variables: age range, DM2 (yes or no), AF (yes or no), gender (taking male gender as reference) and readmission (yes or no). Statistical significance was considered for p<0.05.
ResultsConsidering the total cases (DM2 and non-diabetics), the number of cases of stroke remained stable between 2011 and 2013 at around 96,000 cases per year. The patients with DM2 represented 29.3% of the sample. The total number of ischemic accidents increased slightly in that period from 61,605 cases in 2011 to 62,756 cases in 2013. Similarly, TIA increased slightly from 12,563 cases in 2011 to 13,342 cases in 2013. Consequently, hemorrhagic accidents decreased in that same period from 18,485 cases to 17,925 cases per year. Based only on the cases recorded during the study period in the field “principal diagnosis”, 64.1% (n=186,462) of the cases of stroke were classified as ischemic, 18.7% (n=54,401) as hemorrhagic, and 13.3% (n=38,662) as TIA. The rest comprised the group of “poorly defined” cases.
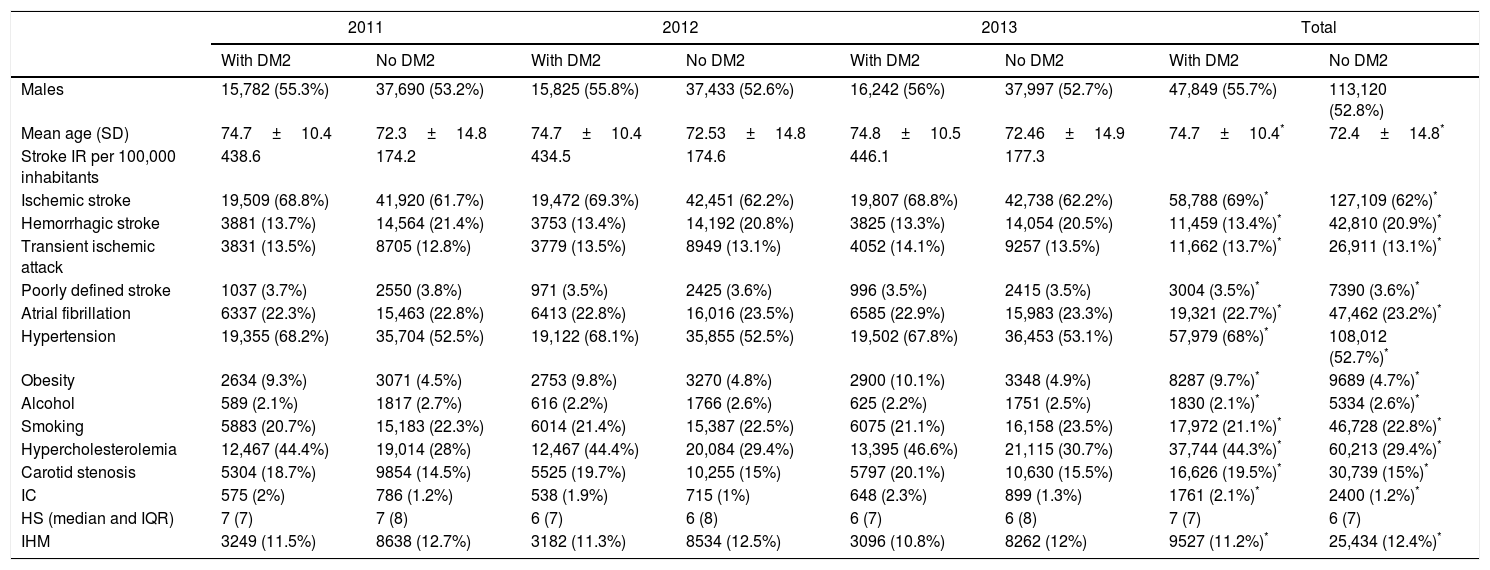
The mean age of the sample was 73.07±13.84 years, and most of the patients were males (54.3%). The patients with diabetes were slightly older than those without diabetes (74.79±10.548 years for DM2 versus 72.41±14.93 years in the non-diabetic population; p<0.05). Table 1 shows the socio-demographic characteristics and provides a descriptive analysis of the different clinical and sociodemographic variables by year and population group (with and without DM2).
Characteristics of patient admissions due to stroke in the Spanish population with and without DM2, 2011–2013.
| 2011 | 2012 | 2013 | Total | |||||
|---|---|---|---|---|---|---|---|---|
| With DM2 | No DM2 | With DM2 | No DM2 | With DM2 | No DM2 | With DM2 | No DM2 | |
| Males | 15,782 (55.3%) | 37,690 (53.2%) | 15,825 (55.8%) | 37,433 (52.6%) | 16,242 (56%) | 37,997 (52.7%) | 47,849 (55.7%) | 113,120 (52.8%) |
| Mean age (SD) | 74.7±10.4 | 72.3±14.8 | 74.7±10.4 | 72.53±14.8 | 74.8±10.5 | 72.46±14.9 | 74.7±10.4* | 72.4±14.8* |
| Stroke IR per 100,000 inhabitants | 438.6 | 174.2 | 434.5 | 174.6 | 446.1 | 177.3 | ||
| Ischemic stroke | 19,509 (68.8%) | 41,920 (61.7%) | 19,472 (69.3%) | 42,451 (62.2%) | 19,807 (68.8%) | 42,738 (62.2%) | 58,788 (69%)* | 127,109 (62%)* |
| Hemorrhagic stroke | 3881 (13.7%) | 14,564 (21.4%) | 3753 (13.4%) | 14,192 (20.8%) | 3825 (13.3%) | 14,054 (20.5%) | 11,459 (13.4%)* | 42,810 (20.9%)* |
| Transient ischemic attack | 3831 (13.5%) | 8705 (12.8%) | 3779 (13.5%) | 8949 (13.1%) | 4052 (14.1%) | 9257 (13.5%) | 11,662 (13.7%)* | 26,911 (13.1%)* |
| Poorly defined stroke | 1037 (3.7%) | 2550 (3.8%) | 971 (3.5%) | 2425 (3.6%) | 996 (3.5%) | 2415 (3.5%) | 3004 (3.5%)* | 7390 (3.6%)* |
| Atrial fibrillation | 6337 (22.3%) | 15,463 (22.8%) | 6413 (22.8%) | 16,016 (23.5%) | 6585 (22.9%) | 15,983 (23.3%) | 19,321 (22.7%)* | 47,462 (23.2%)* |
| Hypertension | 19,355 (68.2%) | 35,704 (52.5%) | 19,122 (68.1%) | 35,855 (52.5%) | 19,502 (67.8%) | 36,453 (53.1%) | 57,979 (68%)* | 108,012 (52.7%)* |
| Obesity | 2634 (9.3%) | 3071 (4.5%) | 2753 (9.8%) | 3270 (4.8%) | 2900 (10.1%) | 3348 (4.9%) | 8287 (9.7%)* | 9689 (4.7%)* |
| Alcohol | 589 (2.1%) | 1817 (2.7%) | 616 (2.2%) | 1766 (2.6%) | 625 (2.2%) | 1751 (2.5%) | 1830 (2.1%)* | 5334 (2.6%)* |
| Smoking | 5883 (20.7%) | 15,183 (22.3%) | 6014 (21.4%) | 15,387 (22.5%) | 6075 (21.1%) | 16,158 (23.5%) | 17,972 (21.1%)* | 46,728 (22.8%)* |
| Hypercholesterolemia | 12,467 (44.4%) | 19,014 (28%) | 12,467 (44.4%) | 20,084 (29.4%) | 13,395 (46.6%) | 21,115 (30.7%) | 37,744 (44.3%)* | 60,213 (29.4%)* |
| Carotid stenosis | 5304 (18.7%) | 9854 (14.5%) | 5525 (19.7%) | 10,255 (15%) | 5797 (20.1%) | 10,630 (15.5%) | 16,626 (19.5%)* | 30,739 (15%)* |
| IC | 575 (2%) | 786 (1.2%) | 538 (1.9%) | 715 (1%) | 648 (2.3%) | 899 (1.3%) | 1761 (2.1%)* | 2400 (1.2%)* |
| HS (median and IQR) | 7 (7) | 7 (8) | 6 (7) | 6 (8) | 6 (7) | 6 (8) | 7 (7) | 6 (7) |
| IHM | 3249 (11.5%) | 8638 (12.7%) | 3182 (11.3%) | 8534 (12.5%) | 3096 (10.8%) | 8262 (12%) | 9527 (11.2%)* | 25,434 (12.4%)* |
The above-mentioned table shows the incidence of stroke by study year (per 100,000 inhabitants) in both the diabetic and the non-diabetic populations. The incidence rate ratio of the DM2 population versus the non-diabetic population showed the proportion of stroke in the diabetic population to be 2.5 times higher than in the non-diabetic population in all the years studied. The chi-squared test confirmed the presence of a probabilistic association between the different stroke groups and DM2 in all cases except the “poorly defined” group (p<0.05). With regard to the frequencies of stroke, ischemic stroke was seen to be the most common presentation, followed by hemorrhagic stroke and TIA.
As shown in Table 1, the most prevalent VRFs in both patients with and without DM2 were AHT followed by hypercholesterolemia. Both VRFs (AHT and hypercholesterolemia) were more prevalent in the DM2 population than in the non-diabetic population (p<0.05), in contrast to smoking. Likewise, an increased prevalence of obesity was found in the patients with DM2. In terms of gender, the male population showed a higher prevalence of alcohol consumption (4.1% vs. 0.5%; p<0.05) and smoking (35% vs. 7.3%; p<0.05). In the female population, the most prevalent VRFs were AHT (59.8% vs. 55%; p<0.05) and obesity (7.4% vs. 5.2%; p<0.05).
No significant differences were observed with regard to the diagnostic procedures performed according to the ischemic or hemorrhagic origin of stroke, the most common technique being a brain CT scan (76.2%) followed by brain MRI (25.8%).
Regarding the medical procedures in ischemic accidents, thrombolysis was the most commonly adopted measure, mainly in patients without diabetes (4.4% vs. 3.0%; p<0.05), followed by endarterectomy, which proved more common in patients with DM2 (2.0% in non-diabetics vs. 2.8% in diabetics; p<0.05).
In hemorrhagic accidents the main medical procedure was embolization, especially in patients without diabetes (5.7% in non-diabetics vs. 1.0% in diabetics; p<0.05).
Evaluation of the evolution of the diagnostic and medical procedures during the study period revealed no significant variations over time.
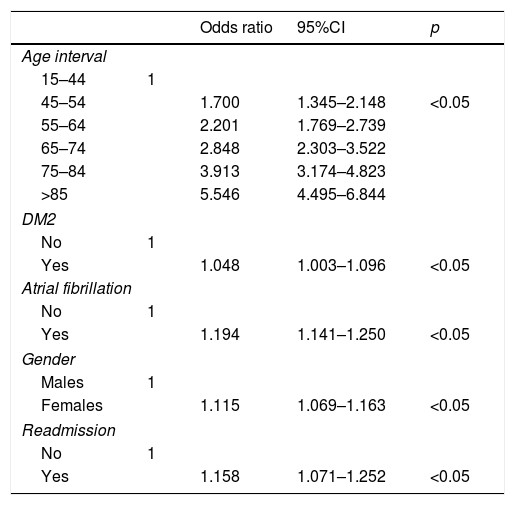
The binary multivariate analysis (Table 2) showed in-hospital mortality (IHM) to increase substantially with advancing age, DM2, atrial fibrillation, the female gender and hospital readmission.
Binary multivariate logistic regression analysis of factors associated with in-hospital mortality related to any type of stroke in the Spanish population, 2011–2013.
| Odds ratio | 95%CI | p | ||
|---|---|---|---|---|
| Age interval | ||||
| 15–44 | 1 | |||
| 45–54 | 1.700 | 1.345–2.148 | <0.05 | |
| 55–64 | 2.201 | 1.769–2.739 | ||
| 65–74 | 2.848 | 2.303–3.522 | ||
| 75–84 | 3.913 | 3.174–4.823 | ||
| >85 | 5.546 | 4.495–6.844 | ||
| DM2 | ||||
| No | 1 | |||
| Yes | 1.048 | 1.003–1.096 | <0.05 | |
| Atrial fibrillation | ||||
| No | 1 | |||
| Yes | 1.194 | 1.141–1.250 | <0.05 | |
| Gender | ||||
| Males | 1 | |||
| Females | 1.115 | 1.069–1.163 | <0.05 | |
| Readmission | ||||
| No | 1 | |||
| Yes | 1.158 | 1.071–1.252 | <0.05 | |
The results of this study indicate stability in the number of cases of hospital admission due to stroke and its associated IHM during the period studied. These findings are in contrast to the decreasing trend described in other Spanish national publications8,9 and the changes in incidence they predict. On the other hand, the stability of the number of cases of stroke among patients without diabetes reported in our study is consistent with the observations of a German study.10
This study found ischemic accidents to be the main cause of admission due to stroke in the Spanish population during the study period, in concordance with other both national11 and international publications.12
Among the different VRFs, the most prevalent was seen to be AHT, particularly among patients with DM2. This agrees with the data reported by previous studies conducted in Spain and in other European countries.13,14 As a result, the control of hypertension in patients with DM2 has been emphasized as a preventive strategy in view of the risk of death from chronic complications in stroke patients.15 This is consistent with the recommendation of the American Diabetes Association (ADA) to maintain “blood pressure below 140/90mmHg in all patients with diabetes”.16
The prevalence of certain VRFs (AHT, obesity and hypercholesterolemia) was higher in the DM2 population (p<0.05), in concordance with the study published by Miguel-Yanes et al.6 However, in contrast to the above-mentioned study, we did not find the prevalence of VRFs to increase during the study period. Nevertheless, both studies are complementary in this regard, because Miguel-Yanes studied the years 2002, 2006, 2010 and 2014, and on comparing their results between 2002 and 2014 they effectively recorded an increase in prevalence, though this trend faded between 2010 and 2014. We studied the same period (2011–2013), and our results are therefore complementary. In this regard it may be stated that although there was an increase in the prevalence of VRFs from 2002, the variations in prevalence were less than 5% in all cases from the year 2010 onwards. This is consistent with Navarro-Vidal et al., who described the poor control of certain VRFs in the Spanish population with DM2 despite treatment.17
The observed higher prevalence of obesity in subjects with diabetes is consistent with the recommendations on the importance of improving modifiable VRFs in the DM2 population.18 The proportion of obesity and hypercholesterolemia among the patients diagnosed with diabetes was higher than in the patients without diabetes (p<0.05). This fact supports the association between hypercholesterolemia and DM2 and the high risk of cardiovascular accidents reported some decades ago by the Framingham study.19
The results of this study indicate that the number of cases of stroke in the Spanish population with DM2 is 2.5-fold higher than in the population without diabetes. This confirms the increased risk (2–4-fold20 or 1.5–3-fold21) of stroke in individuals with DM2 compared with the non-diabetic population described by other European authors. These observations may be related to the changes in brain vessels and brain structure caused by diabetes.22
The use of thrombolysis mainly in patients without diabetes is in contrast to the data reported by another European study23 suggesting that diabetes is not a contraindication to thrombolysis in ischemic stroke. On the other hand, endarterectomy was more common in patients with diabetes because, as reported by Mizuhashi et al., the quality of the outcomes of the procedure is not influenced by the presence of diabetes even when such patients have a more frequent history of coronary artery disease.24
The association between gender and stroke-related mortality detected by the logistic regression analysis has also been reported by other authors. Some investigators indicate high ratios and reduced survival among the female population.25,26 However, Koton et al., support the idea that the factors influencing subsequent survival are patient characteristics and the severity of the vascular accident.27 In our study, female gender was significantly associated with IHM (odds ratio [OR]: 1.115; 95% confidence interval [95%CI]: 1.069–1.163; p<0.05).
The importance of our study is that the database used for the analysis was of a considerable size, thereby making it possible for reliable statistical conclusions to be drawn. The methodology used was similar to that employed in previous studies on diabetes.2 The database used was the CMBD-AH, which is an administrative clinical registry compiling discharge reports and regulated by law (Spanish Royal Decree 69/2015 of 6 February).
The limitations of the study are the lack of information on the duration of diabetes and the level of control of the VRFs. As a result, the variables used in the study were treated as binary variables, thereby limiting the statistical study options.
ConclusionsAccording to the data obtained from the Spanish national registry of hospital discharges regarding ischemic and hemorrhagic accidents in the period 2011–2013, the most prevalent VRFs among the populations with and without DM2 are AHT and hypercholesterolemia. Computed axial tomography is the most widely used diagnostic technique in both population groups. The risk of IHM significantly increases with age, with the presence of atrial fibrillation, female gender, hospital readmission, and DM2 as independent factors. In addition, the DM2 population shows a 2.5-fold greater number of stroke-related hospital admissions than the non-diabetic population.
Conflicts of interestThe authors state that they have no conflicts of interest.
Dr. Barea has collaborated in the analysis of the data, as well as in the revision and approval of the manuscript. Dr. González-Pascual has collaborated in the conception and design of the manuscript, data collection and writing, as well as in the revision and subsequent approval of the manuscript.
Please cite this article as: González-Pascual M, Barea R. Prevalencia de los factores de riesgo vascular entre los casos con diabetes mellitus tipo 2 y sin diabetes hospitalizados de 2011 a 2013 por accidentes cerebrovasculares. Endocrinol Diabetes Nutr. 2019;66:150–156.