Bariatric surgery has been shown to provide sustained weight loss and to decrease obesity-related mortality in most patients with morbid obesity, but its effect on cancer risk is less clear. Our aim was to review the published studies on the association between bariatric surgery and cancer risk.
MethodsA literature search for relevant articles published in English, with no limitation on the year of publication, was conducted using PubMed. Studies reporting data on preoperative cancer, case reports, and publications with no abstract available were excluded.
ResultsOverall, the published literature suggests that bariatric surgery may decrease risk of cancer, although this effect appears to be limited to women. However, two recent studies contradict these findings and state that risk of cancer has not been actually shown to decrease after surgery, and an increased risk of colorectal cancer has even been seen.
Although most studies report lower cancer risk after bariatric surgery, the main limitations include their designs, which do not achieve the highest levels of evidence. Moreover, several mechanisms have been proposed to explain the protective effect of surgery, but the exact mechanisms have not been elucidated yet, which suggests the need for further research.
ConclusionsBariatric surgery may have a protective effect from overall cancer risk, mainly in women, but additional research is needed. Further research is also required to better examine the relationship between bariatric surgery and risk of colorectal cancer before confirming or dismissing the above reported higher risk, as well as the risk of esophagogastric cancer, which has not been adequately studied to date.
La cirugía bariátrica proporciona una pérdida de peso mantenida y una reducción de la mortalidad relacionada con la obesidad en la mayoría de pacientes con obesidad mórbida, no obstante, su efecto sobre el riesgo de cáncer es menos claro. Nuestra intención fue revisar los estudios publicados hasta la fecha sobre la asociación entre cirugía bariátrica y riesgo de cáncer.
MétodosSe realizó una búsqueda bibliográfica utilizando Pubmed para artículos relevantes, publicados en inglés sin límite de fechas de publicación. Los estudios que relataban datos sobre cáncer preoperatorio, los casos clínicos y publicaciones sin resumen disponible no fueron incluidos.
ResultadosEn conjunto, los artículos publicados en la literatura sugieren que la cirugía bariátrica puede disminuir el riesgo de cáncer, aunque el efecto beneficioso parece limitado a las mujeres. No obstante, 2 estudios recientes contradicen estos hallazgos, revelando que no se ha podido comprobar realmente que mejore el riesgo de cáncer después de la cirugía bariátrica, y que incluso se ha observado un aumento del riesgo de cáncer colorrectal.
Aunque la mayoría de estudios refieren disminución del riesgo de cáncer después de la cirugía, las principales limitaciones son los diseños, que no alcanzan los niveles más elevados de evidencia. Además, se han propuesto varios mecanismos par explicar el efecto protector de la cirugía, no obstante, aún no se conocen con precisión, indicando la necesidad de más investigación.
ConclusionesLa cirugía bariátrica podría tener un efecto protector sobre el riesgo general de cáncer, principalmente en mujeres, pero se necesita más investigación para su confirmación. De la misma manera, se requiere más investigación para examinar la relación entre la cirugía bariátrica y el riesgo de cáncer de colon antes de confirmar o desmentir el aumento del riesgo referido recientemente. También son necesarios más estudios sobre el riesgo de cáncer gastroesofágico poscirugía bariátrica, ya que no se ha estudiado adecuadamente hasta la actualidad.
Obesity is considered a major health concern that has reached epidemic proportions and is growing at alarming rates around the world. More than 1.4 billion adults worldwide are overweight, more than half a billion are obese and at least 2.8 million people die each year as a consequence of being overweight or obese. The relationship between obesity and certain comorbidities, such as diabetes and cardiovascular disease, has been well documented, as well as its link with an increased risk of some cancer types.1
While several medical interventions have been used to decrease obesity, including lifestyle modification and pharmacotherapy, none have shown long-term efficacy in severely obese patients, so bariatric surgery has emerged as an alternative treatment option. It is well established that this type of surgery provides sustained weight loss and reduced obesity-related mortality, also achieving pronounced metabolic effects including diabetes resolution in the majority of morbidly obese patients,2 but it is less clear how cancer risk is affected. The purpose of this article is to review the published studies on the association between bariatric surgery and cancer risk.
MethodsA search for relevant articles was conducted on PubMed using the terms “bariatric surgery”, and “obesity surgery” along with “neoplasm”, “cancer” and “cancer risk”. Inclusion criteria were human studies relevant to the primary research question, published in English, without limitation on the year of publication. Exclusion criteria incorporated studies reporting data on preoperative cancers, case reports and also those with no abstract available.
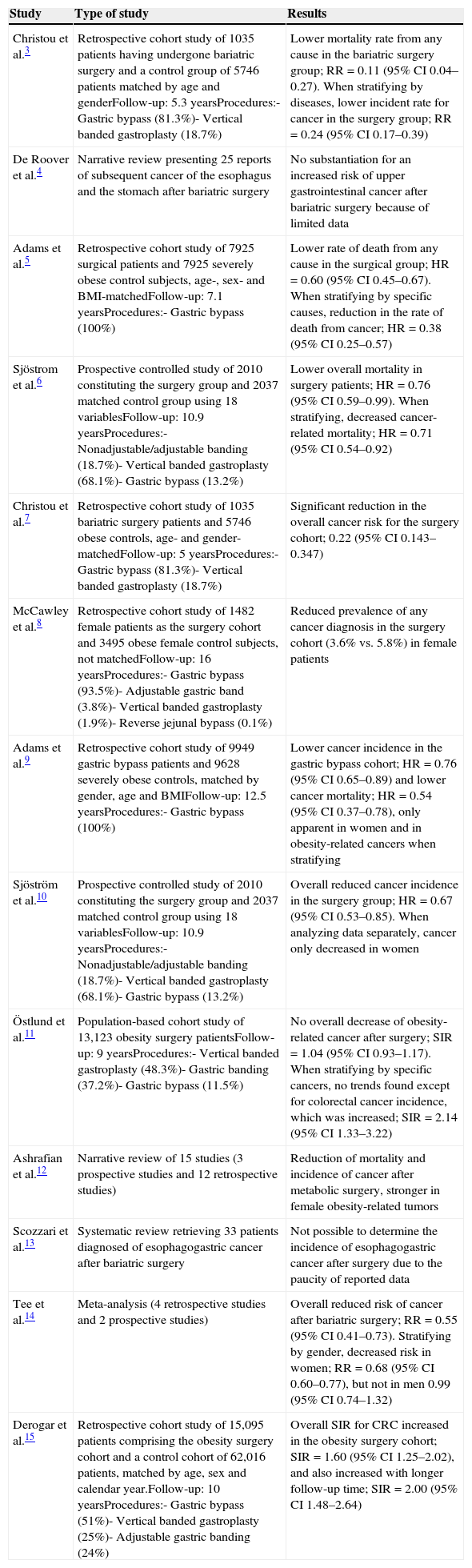
ResultsOur review identified one existing meta-analysis and three narrative reviews that reported on oncologic outcomes after bariatric surgery, along with nine published observational studies (Table 1). Of these, most studies focused on overall cancer risk, while only a few examined the risk of some specific cancers.
Summary of evidence on associations between bariatric surgery and cancer risk.
| Study | Type of study | Results |
|---|---|---|
| Christou et al.3 | Retrospective cohort study of 1035 patients having undergone bariatric surgery and a control group of 5746 patients matched by age and genderFollow-up: 5.3 yearsProcedures:- Gastric bypass (81.3%)- Vertical banded gastroplasty (18.7%) | Lower mortality rate from any cause in the bariatric surgery group; RR=0.11 (95% CI 0.04–0.27). When stratifying by diseases, lower incident rate for cancer in the surgery group; RR=0.24 (95% CI 0.17–0.39) |
| De Roover et al.4 | Narrative review presenting 25 reports of subsequent cancer of the esophagus and the stomach after bariatric surgery | No substantiation for an increased risk of upper gastrointestinal cancer after bariatric surgery because of limited data |
| Adams et al.5 | Retrospective cohort study of 7925 surgical patients and 7925 severely obese control subjects, age-, sex- and BMI-matchedFollow-up: 7.1 yearsProcedures:- Gastric bypass (100%) | Lower rate of death from any cause in the surgical group; HR=0.60 (95% CI 0.45–0.67). When stratifying by specific causes, reduction in the rate of death from cancer; HR=0.38 (95% CI 0.25–0.57) |
| Sjöstrom et al.6 | Prospective controlled study of 2010 constituting the surgery group and 2037 matched control group using 18 variablesFollow-up: 10.9 yearsProcedures:- Nonadjustable/adjustable banding (18.7%)- Vertical banded gastroplasty (68.1%)- Gastric bypass (13.2%) | Lower overall mortality in surgery patients; HR=0.76 (95% CI 0.59–0.99). When stratifying, decreased cancer-related mortality; HR=0.71 (95% CI 0.54–0.92) |
| Christou et al.7 | Retrospective cohort study of 1035 bariatric surgery patients and 5746 obese controls, age- and gender-matchedFollow-up: 5 yearsProcedures:- Gastric bypass (81.3%)- Vertical banded gastroplasty (18.7%) | Significant reduction in the overall cancer risk for the surgery cohort; 0.22 (95% CI 0.143–0.347) |
| McCawley et al.8 | Retrospective cohort study of 1482 female patients as the surgery cohort and 3495 obese female control subjects, not matchedFollow-up: 16 yearsProcedures:- Gastric bypass (93.5%)- Adjustable gastric band (3.8%)- Vertical banded gastroplasty (1.9%)- Reverse jejunal bypass (0.1%) | Reduced prevalence of any cancer diagnosis in the surgery cohort (3.6% vs. 5.8%) in female patients |
| Adams et al.9 | Retrospective cohort study of 9949 gastric bypass patients and 9628 severely obese controls, matched by gender, age and BMIFollow-up: 12.5 yearsProcedures:- Gastric bypass (100%) | Lower cancer incidence in the gastric bypass cohort; HR=0.76 (95% CI 0.65–0.89) and lower cancer mortality; HR=0.54 (95% CI 0.37–0.78), only apparent in women and in obesity-related cancers when stratifying |
| Sjöström et al.10 | Prospective controlled study of 2010 constituting the surgery group and 2037 matched control group using 18 variablesFollow-up: 10.9 yearsProcedures:- Nonadjustable/adjustable banding (18.7%)- Vertical banded gastroplasty (68.1%)- Gastric bypass (13.2%) | Overall reduced cancer incidence in the surgery group; HR=0.67 (95% CI 0.53–0.85). When analyzing data separately, cancer only decreased in women |
| Östlund et al.11 | Population-based cohort study of 13,123 obesity surgery patientsFollow-up: 9 yearsProcedures:- Vertical banded gastroplasty (48.3%)- Gastric banding (37.2%)- Gastric bypass (11.5%) | No overall decrease of obesity-related cancer after surgery; SIR=1.04 (95% CI 0.93–1.17). When stratifying by specific cancers, no trends found except for colorectal cancer incidence, which was increased; SIR=2.14 (95% CI 1.33–3.22) |
| Ashrafian et al.12 | Narrative review of 15 studies (3 prospective studies and 12 retrospective studies) | Reduction of mortality and incidence of cancer after metabolic surgery, stronger in female obesity-related tumors |
| Scozzari et al.13 | Systematic review retrieving 33 patients diagnosed of esophagogastric cancer after bariatric surgery | Not possible to determine the incidence of esophagogastric cancer after surgery due to the paucity of reported data |
| Tee et al.14 | Meta-analysis (4 retrospective studies and 2 prospective studies) | Overall reduced risk of cancer after bariatric surgery; RR=0.55 (95% CI 0.41–0.73). Stratifying by gender, decreased risk in women; RR=0.68 (95% CI 0.60–0.77), but not in men 0.99 (95% CI 0.74–1.32) |
| Derogar et al.15 | Retrospective cohort study of 15,095 patients comprising the obesity surgery cohort and a control cohort of 62,016 patients, matched by age, sex and calendar year.Follow-up: 10 yearsProcedures:- Gastric bypass (51%)- Vertical banded gastroplasty (25%)- Adjustable gastric banding (24%) | Overall SIR for CRC increased in the obesity surgery cohort; SIR=1.60 (95% CI 1.25–2.02), and also increased with longer follow-up time; SIR=2.00 (95% CI 1.48–2.64) |
Christou et al.3 conducted one of the first studies to appear on this topic. This retrospective cohort study demonstrated that bariatric surgery is associated with significant reductions in morbidity, mortality and healthcare use, which were its primary outcomes. But when stratifying by diseases, the most notable risk reduction was observed for the incidence of malignancies.
In order to expand these findings, they designed another study7 in which the main objective was to assess the differences between the two cohorts with respect to cancer in general and cancer of specific sites. Data were extracted from physician and hospital visits for a cancer-related diagnosis. The surgery patients had significantly fewer visits for all cancer diagnoses, suggesting that this type of surgery not only reduces morbidity but also decreases the incidence of malignant disease.
This finding was also supported by Adams et al., which initially designed a retrospective cohort study5 in order to examine long-term mortality after bariatric surgery and, similarly to the previous authors, once they analyzed the cause-specific mortality, they found a great reduction in the rate of death from cancer. Building upon these results, they conducted another retrospective cohort study9 with the purpose of testing whether reduced cancer mortality following bariatric surgery was due to decreased incidence. The study revealed a lower incidence of cancer in surgery patients, although the protective effect of surgery was limited to women and to obesity-related cancers. Following this principle, McCawley et al. conducted a retrospective cohort study8 that only included female subjects, and concluded that a higher percentage of control women were diagnosed with cancer. Along these lines, the SOS study10 reported reduced cancer incidence in obese women but not in obese men. A previous study6 by the same authors had shown a reduced overall mortality associated with bariatric surgery, but it was no sufficiently powered to assess mortality due to specific causes.
Contrary results were obtained in a population-based cohort study by Östlund et al.,11 in which neither the risk of all cancer nor the risk of obesity-related cancers were decreased after bariatric surgery.
To ascertain conclusively the effects of bariatric surgery on oncologic outcomes, Tee et al.14 analyzed the published literature in a recent meta-analysis which included six observational studies and concluded that the RR of cancer in obese patients after bariatric surgery was lower. Stratification by gender was also pursued, and the protective effect of bariatric surgery was only demonstrated for women. A similar conclusion was reached by Ashrafian et al. through a narrative review,12 which stated that metabolic surgery patients have lower cancer rates and mortality compared with obese patients who have not had this surgery, although the beneficial effects are stronger in female subjects.
Risk of specific cancersThe above-mentioned studies have limited data for other endpoints than the overall cancer risk, but some differences in specific cancer risk were noted in two studies. Christou et al.7 revealed that the RR of breast cancer was significantly lower in the bariatric cohort. Different results were obtained in Östlund et al. study,11 in which not only did they found that the risk of breast cancer, as well as the prostate, endometrial and kidney cancer, were not decreased in the bariatric cohort, but they also identified a statistically significantly increased risk of colorectal cancer after surgery. This unexpected finding led the authors to hypothesize that obesity surgery might be associated with increased colorectal cancer risk and they designed a nationwide retrospective cohort study,15 which concluded that the risk for colorectal cancer increased with time after surgery.
There are two review articles4,13 that also discuss the potential influence of obesity surgery on some specific cancers, focusing on the upper gastrointestinal tract. They both concluded that it is impossible to quantify esophagogastric cancer incidence after surgery because of the paucity of data. They also agreed that carefully evaluation of digestive tract symptoms is mandatory after bariatric surgery in order to prevent the delay in diagnosis.
DiscussionUntil recently, all the published articles that focused on the potential link between bariatric surgery and cancer risk had reported a protective effect,3,5–10,14 but the current controversy arose with the publication of the article by Derogar et al.,15 which showed a long-term increased risk of colorectal cancer after bariatric surgery. This study has had a significant impact on the bariatric surgery community, becoming an important matter of debate. Our task is to make judgments about the strength of the evidence and the validity of the data before reaching any conclusion.
In the first studies to appear on this topic,3,5,6 the primary outcome was designated as mortality or morbidity from any cause, not specifically from cancer. Although the results revealed a lower incidence of cancer in the surgery cohort, the probability of a chance effect was increased, since multiple statistical comparisons were performed. Therefore, those studies were only powered and monitored on the basis of the primary outcome variable.
Regarding the studies in which cancer risk constitutes the primary outcome,7–11 no randomized trials have been conducted yet. Thus, the main limitations include their designs, which do not achieve the highest levels of evidence. Even though it could not be randomized for ethical reasons, SOS study10 provides the best evidence with a robust matching of the surgery group, taking into account a richness of cardiovascular, anthropometric and biochemical parameters. This prospective cohort study included ten pre-defined visits in both surgery and control groups, so the chance for cancer detection was similar in both groups. They stated a reduced cancer incidence in obese women but not in men after a follow-up of 15 years, which persisted after the exclusion of all cancer cases that appeared during the first 3 years of intervention. However, secondary subgroup analysis showed no associations between cancer incidence and weight loss or reduced energy intake, which could have been explained by limited statistical power as a consequence of dividing into multiple subgroups. But another explanation could be the interesting possibility that the beneficial effects of bariatric surgery on cancer could be explained by mechanisms other than reduced energy intake or weight loss.
Actually, several mechanisms have been proposed to explain the potential cancer protective role of bariatric surgery, like the improvement of insulin resistance, decreased oxidative stress and inflammation, along with the beneficial modulation of sex-steroids, gut hormones, cellular energetics, adipokines and the immune system,12 but more investigation needs to be done in this field to clarify the precise metabolic mechanisms. As we acknowledged, the majority of the studies state that bariatric surgery might have a protective role in cancer risk, although its effect seems limited to women, reinforcing the importance of studying mechanisms separately by gender.
Focusing in obese women, breast and endometrial cancers remain the most common types, which are hormonally responsive tumors. As it is known, obesity results in a profound change in hormone levels, with effects on circulating peptide and steroid hormones and their binding factors, and these changes may be partially corrected with weight loss.12 In the study by McCawley et al.,8 in which only female subjects were constituting the cohorts, some limitations may disqualify drawing any reliable conclusion, like the fact of not matching the cohorts or including the cancers before the operation, as in order for a study to be valid, the control cohort needs to be as equal as possible to the experimental cohort. Taking this into account, the control group used by Östlund et al.11 was also inadequate, since the cancer risk after bariatric surgery was compared with the general population, whose body mass index surely differed from the operated patients. Subsequently, not having done a carefully control group selection may lead into some misunderstanding and this could be one of the reasons why the observed cancer risk in the surgery cohort was not decreased. Indeed, Tee et al.14 decided not to include this study in their meta-analysis since it did not meet the criteria of having an appropriate control group.
However, standardizing in order to have homogeneous groups does not exclude the influence of other factors or the existence of some biases, for example, operative candidates may have been more motivated to quit smoking, do more exercise or follow healthy diets, which could have influenced the results of the studies that showed a decreased risk. In the same way, focusing on the controversial study15 that detected an increased risk of colorectal cancer, factors like weight change, body mass distribution are known to influence its incidence, along with the type of diet or the use of protective drugs like aspirin.
Regarding this last study,15 there are some other considerations that should be taken into account. Conventionally, bariatric surgery has been subdivided into restrictive procedures and malabsorptive procedures, and this study, which included both techniques, found that the increased risk was similar for all the techniques. Some authors16 point out that it is hard to understand how cancer risk could be increased when restrictive procedures were performed since the anatomical or absorptive function of the gastrointestinal tract remained untouched. However, rectal mucosal hyperproliferation persists at least 3 years after Roux-en-Y gastric bypass, which has been associated with increased mucosal expression of the protumorigenic cytokine macrophage migration inhibitory factor,17 and recent studies have also stated alterations in the intestinal microbiota and an increased mucosal bile salt exposure,18 both implicated in long-term neoplastic risk. Moreover, the effect of postsurgical neurohormonal modulation may also play a role. In this sense, controversial findings about ghrelin levels in different stages of colon cancer cause to raise the question whether it is carcinogenic or protective against gastrointestinal malignancies.19 Also, PYY may be relevant to the development and progression of colon adenocarcinoma as pointed out in some studies.20 Taking into account that Roux-en-Y gastric bypass is increasingly performed, the hypothesis that this study suggests should not be dismissed and, considering the large sample size, the long follow-up (up to 30 years) and the validity of the data afforded by the Swedish National Registers, further research on this topic is required. In fact, the same authors have initiated a Nordic study and a separated British population study in order to confirm their findings,21 using independent databases. Nevertheless, the concept that overall cancer risk is decreased after bariatric surgery would not have to be incompatible with an increased risk of colorectal cancer, in case the last was confirmed, since different mechanisms could play a part.
Concerning upper gastrointestinal malignancies, neither observational nor experimental studies have been performed so its incidence remains unclear. Nonetheless, a delay in diagnosis is commonly observed because patients usually present with symptoms that can be mistaken with those associated with the operation itself and furthermore, the excluded distal stomach is more difficult to investigate.4,13
In summary, most of the published literature3,5–10,14 found that overall cancer risk was decreased after bariatric surgery, principally in women, but more appropriate designs would be necessary since the existing studies do not achieve the highest levels of evidence. Focusing in specific cancer risk, further research is also required before the association between colorectal cancer and bariatric surgery is dismissed or established, since there is only one study to date.15 Regarding the upper gastrointestinal tract, the paucity of the data makes impossible to determine its incidence, although the published literature agrees that the greatest concern is the delay in diagnosis.4,13
ConclusionsIt seems likely that bariatric surgery could have a protective effect for overall cancer risk, particularly in women. However, more research is needed in order to confirm these findings, which have been investigated by too few studies to date. The ideal research approach would be a randomized trial of sustained weight reduction through bariatric surgery and cancer outcomes. In addition to this, there is an understudied area concerning animal models, which could provide explanations of the implicated mechanisms.
Regarding colorectal cancer risk, there is only one study reporting an increased incidence after surgery, so more investigation must be initiated to better examine this relationship, as well as esophagogastric malignancies, which have only been described in case reports.
Conflict of interestsThe authors declare no conflict of interests.