Rhabdomyolysis may be secondary to trauma, excessive muscle activity, hereditary muscle enzyme defects and other medical causes. Primary hyperaldosteronism is characterised by hypertension, hypokalemia, suppressed plasma renin activity, and increased aldosterone excretion. Rhabdomyolysis is not common in primary hyperaldosteronism. We report here a 42-year-old woman presenting with rhabdomyolysis as heralding symptom of primary hyperaldosteronism. We also carried out a search of the literature to identify all cases of rhabdomyolysis as the firstrecognized expression of a primary hyperaldosteronism. Sixteen cases met the criteria for inclusion. When rhabdomyolysis occurs in a patient with hypokalemia and metabolic alkalosis, primary hyperaldosteronism has to be suspected: if confirmed, an aldosterone-producing adenoma is the most probable cause.
La rabdomiólisis puede ser secundaria a traumatismos, excesiva actividad muscular, enfermedades musculares hereditarias y otras causas médicas. El hiperaldosteronismo primario se caracteriza por hipertensión, hipopotasemia, actividad de renina plasmática suprimida y secreción aumentada de aldosterona. La rabdomiólisis no es frecuente en el hiperaldosteronismo primario. Presentamos el caso de una mujer de 42 años que sufrió una rabdomiólisis como manifestación inicial de un hiperaldosteronismo primario. También realizamos una búsqueda bibliográfica para identificar casos de rabdomiólisis como primera manifestación de hiperaldosteronismo primario; 16 casos cumplieron criterios de inclusión. Cuando aparece rabdomiólisis en un paciente con hipopotasemia y alcalosis metabólica debe sospecharse un hiperaldosteronismo primario: si se confirma, la causa más probable será un adenoma productor de aldosterona.
The word rhabdomyolysis is generally used to include the clinical and laboratory syndrome resulting from muscle injury and release of potentially dangerous substances into the circulation1. Rhabdomyolysis may be secondary to trauma, excessive muscle activity, hereditary muscle enzyme defects and other medical causes including drugs, metabolic disorders (such as hypokalemia, hypophosphatemia, hypernatremia and hyperosmolar state) and endocrine diseases (such us hypothyroidism, hyperthyroidism, diabetic ketoacidosis, and pheochromocytoma)1.
Primary hyperaldosteronism (PA) was reported by Conn more than fifty years ago2, and hypertension, hypokalemia, suppressed plasma renin activity (PRA), and increased aldosterone excretion characterise classically this syndrome3.
Although the first reports of primary hyperaldosteronism included weakness among the symptoms of this syndrome4, and myopathy related to hyperaldosteronism have been reported in several cases, rhabdomyolysis is not common in primary hyperaldosteronism. Here we report a new case of rhabdomyolysis due to primary hyperaldosteronism and review the patients reported in the literature that showed rhabdomyolysis as the opening manifestation of the syndrome.
CASE REPORTA 42-year old women was admitted to hospital because she complained of generalized weakness and muscular pain. She had not been diagnosed of hypertension, although she said she had had elevated blood pressure sometimes in the past. She did not take any medical or herbal treatment, and she denied to take any kind of liquorice. She had had 3 progressive weakness since one month prior to admission although she had suffered similar symptoms several times in the past. Physical examination revealed a well orientated, alert patient, a blood pressure of 166/108 mm Hg, and flaccid quadriparesis with hyporeflexia.
Laboratory data included the following serum values: sodium 138 mEq/L [normal range (NR): 135–145], bicarbonate 38.8 mEq/L [NR: 20–24], potassium 1.3 mEq/L [NR: 3.5-5], pH 7.536 [NR: 7.350-7.450], creatinine 0.9 mg/dL [NR: 0.5-0.9], creatine phosphokinase (CPK) 21000 IU/L [NR: 26–140], calcium 7.4 mg/dL [NR: 8.6-10.2], and magnesium 1,8 mEq/L [NR: 1.58-2.55]. An electrocardiogram (ECG) showed plain T waves. Urinary potassium at admission was 9.3 mEq/L.
The patient was treated with intravenous potassium, and muscular strenght and CPK gradually normalised, and blood pressure remained high.
Endocrinologic investigation showed intact parathyroid hormone (PTHi) 184 pg/mL [NR: 10–65]; 25-OH-vitamin D 47.7 ng/mL [NR: 12–80]; cortisol after 1 mg of dexametasone 0.2 μg/dL; resting aldosterone 96.6 ng/dL [NR: 1–10.5]; PRA undetectable [NR: 0.4-1.9 ng/mL/h]; 24-hour urinary aldosterone excretion after 3 days salt overload 23.73 μg; aldosterone before infusion of 2 litres of normal saline 52.4 ng/dL [NR: 1–10.5], and after the infusion 116.4 ng/dL, resting aldosterone before 4 hours upright 77.6 ng/dL [NR: 1-10.5], and after being upright 32.2 ng/dL. An abdominal computed tomography (CT) showed a 20×10 mm mass located in the right adrenal gland. Bilateral adrenal venous sampling localized aldosterone production in the right adrenal gland (right adrenal aldosterone/cortisol quotient 98; left adrenal aldosterone/cortisol quotient 3.76; peripheral vein aldosterone/cortisol quotient 13.9) and confirmed the diagnosis of Conn's syndrome. Patient was on spironolactone treatment until a laparoscopic right adrenalectomy was performed. Pathological examination of the gland confirmed a 20 mm adrenal adenoma. Postoperatively the patient was normokaliemic without spironolactone, resting PRA was 0.52 ng/mL/h and aldosterone was 1.3 ng/dL, although hypertension persisted.
REVIEW OF THE LITERATUREWe performed a computer-assisted search of the literature to identify cases with rhabdomyolysis caused by primary hyperaldosteronism. We used the PubMed website for journals indexed in Index Medicus and Google Scholar (http://scholar.google.com) for not-indexed journals. One of the cases was reported by one of us5. The main search keywords were rhabdomyolysis, Conn and hyperaldosteronism. We considered exclusively cases with primary hyperaldosteronism. Then, the references of computer-assisted search results helped us to find more cases. There is not a consensus about CPK concentrations used as a marker of rhabdomyolysis1, so we consider a CPK equal or higher than 1500 IU/ml as marker of rhabdomyolysis when the authors did not diagnose it specifically.
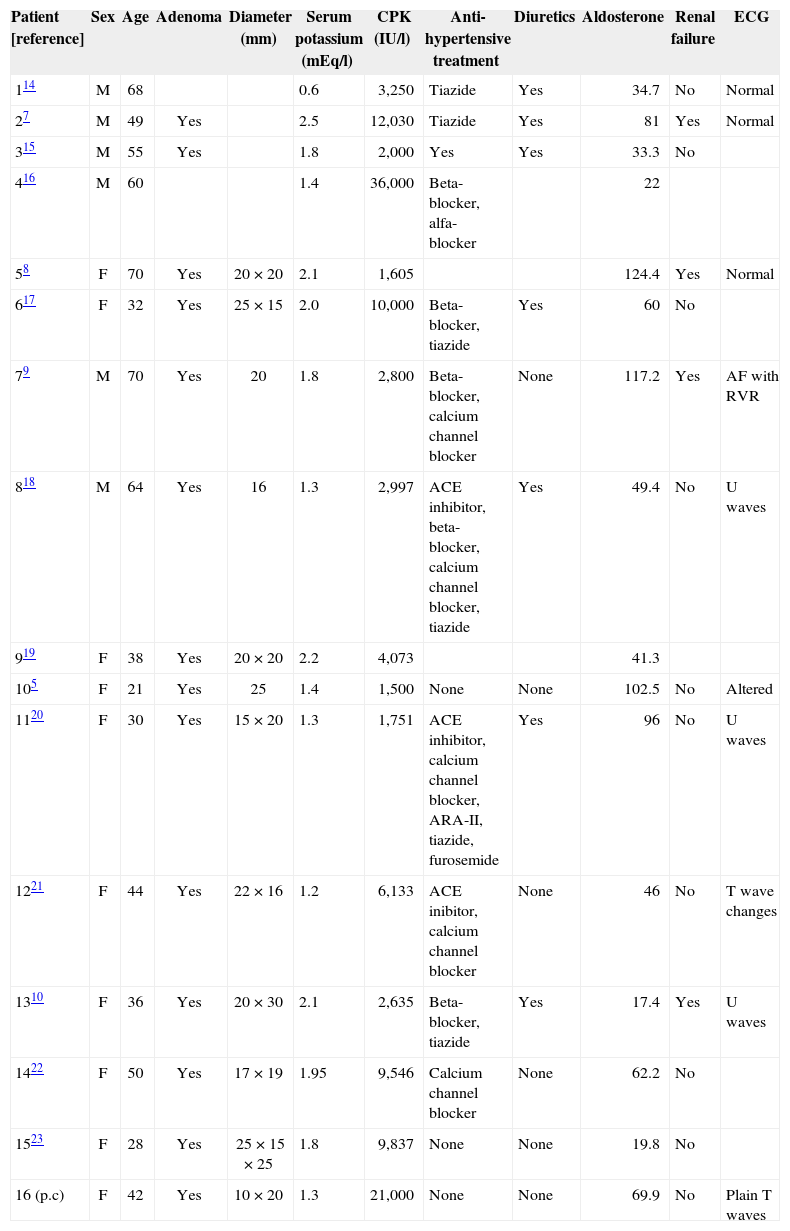
Sixteen cases met the criteria for inclusion. One of them, in Czech language6, was not accessible for us and it was not included in this review. Gender, age, adrenal adenoma as the cause of hyperaldosteronism, previous treatment with anti-hypertensive drugs and diuretics, biochemical and endocrine features and ECG alterations were considered.
Table 114–23 summarises clinical and main laboratory characteristics of patients with rhabdomyolysis and primary hyperaldosteronism, including the present report. There were 7 males and 9 females (including the one from this case study). The mean age of the patients was 47.3±16.0 years (range 21–70 years) but women were significantly younger (mean 39.1±13.7 years vs 61.0±8.0 years, p<0.05). An adrenal adenoma was found in 14 cases with a mean diameter of 19.83±3.16 mm (range 15–25 mm) and the etiology of hyperaldosteronism was not mentioned in the two other cases. The mean serum potassium was 1.67±0.48 mEq/L (range 0.6-2.5 mEq/L). The median CPK was 3662 IU/ L (range 1500–36000 IU/L, 25th percentile 2476 IU/L, 75th percentile 9878 IU/L).
Review of the literature
| Patient [reference] | Sex | Age | Adenoma | Diameter (mm) | Serum potassium (mEq/l) | CPK (IU/l) | Anti-hypertensive treatment | Diuretics | Aldosterone | Renal failure | ECG |
| 114 | M | 68 | 0.6 | 3,250 | Tiazide | Yes | 34.7 | No | Normal | ||
| 27 | M | 49 | Yes | 2.5 | 12,030 | Tiazide | Yes | 81 | Yes | Normal | |
| 315 | M | 55 | Yes | 1.8 | 2,000 | Yes | Yes | 33.3 | No | ||
| 416 | M | 60 | 1.4 | 36,000 | Beta-blocker, alfa-blocker | 22 | |||||
| 58 | F | 70 | Yes | 20 × 20 | 2.1 | 1,605 | 124.4 | Yes | Normal | ||
| 617 | F | 32 | Yes | 25 × 15 | 2.0 | 10,000 | Beta-blocker, tiazide | Yes | 60 | No | |
| 79 | M | 70 | Yes | 20 | 1.8 | 2,800 | Beta-blocker, calcium channel blocker | None | 117.2 | Yes | AF with RVR |
| 818 | M | 64 | Yes | 16 | 1.3 | 2,997 | ACE inhibitor, beta-blocker, calcium channel blocker, tiazide | Yes | 49.4 | No | U waves |
| 919 | F | 38 | Yes | 20 × 20 | 2.2 | 4,073 | 41.3 | ||||
| 105 | F | 21 | Yes | 25 | 1.4 | 1,500 | None | None | 102.5 | No | Altered |
| 1120 | F | 30 | Yes | 15 × 20 | 1.3 | 1,751 | ACE inhibitor, calcium channel blocker, ARA-II, tiazide, furosemide | Yes | 96 | No | U waves |
| 1221 | F | 44 | Yes | 22 × 16 | 1.2 | 6,133 | ACE inibitor, calcium channel blocker | None | 46 | No | T wave changes |
| 1310 | F | 36 | Yes | 20 × 30 | 2.1 | 2,635 | Beta-blocker, tiazide | Yes | 17.4 | Yes | U waves |
| 1422 | F | 50 | Yes | 17 × 19 | 1.95 | 9,546 | Calcium channel blocker | None | 62.2 | No | |
| 1523 | F | 28 | Yes | 25 × 15 × 25 | 1.8 | 9,837 | None | None | 19.8 | No | |
| 16 (p.c) | F | 42 | Yes | 10 × 20 | 1.3 | 21,000 | None | None | 69.9 | No | Plain T waves |
ACE: angiotensin converting enzyme; AF with RVR: atrial fibrillation with rapid ventricular response; CPK: creatine phosphokinase; ECG: electrocardiogram; (p.c): present case.
The median aldosterone was 54.7 ng/dL (range 17.4-124.4 ng/dL, 25th percentile 34.4 ng/dL, 75th percentile 84.8 ng/dL).
Eleven patients were treated with anti-hypertensive drugs (7 of them with diuretics), three patients did not receive any drugs and there was no information about pharmacological treatment in two cases. Four patients had renal failure (defined as elevated serum creatinine): one of them had serum creatinine 23 mg/dL and needed peritoneal dialysis7, and three patients (two of them 70-year old) had mild elevations of creatinine8–10. ECG was normal in 3 patients, there were U waves in 3 patients, changes in T waves in 2 patients, atrial fibrillation with rapid ventricular response in 1 patient and alterations reported as characteristics of hypokalemia in 1 patient.
DISCUSSIONPA is characterised by hypertension, hypokalemia, suppressed PRA, and increased aldosterone excretion. Bilateral idiopathic hyperaldosteronism (IHA) and aldosterone producing adenoma (APA) are the most common subtypes of primary aldosteronism.
Unilateral hyperplasia and familial hyperaldosteronism are much less common3. The first description of PA included muscular symptoms such us spams, weakness and paralysis2 and one of the first series of primary hyperaldosteronism, that included 103 patients, reported muscle weakness in 73% of patients, intermittent paralysis in 21%, tetany in 21% and muscle discomfort in 16%4.
Causes of rhabdomyolysis include trauma, excessive muscle activity, and hereditary muscle enzyme defects, and a variety of medical causes, including drugs and toxins, muscle hypoxia, metabolic and endocrine disorders, infections, temperature alterations, and other entities. Hypokalemia is a recognised cause of rhabdomyolysis. When serum concentrations fall below 3 mEq/L, malaise, muscular weakness, fatigability, the restless leg syndrome, and myalgia may occur. However, muscle enzyme elevations are usually not seen until potassium concentrations fall below 2.5 mEq/L. Frank rhabdomyolysis with myoglobinuria is usually observed only when serum potassium values are below 2 mEq/L1.
Potassium is the major intracellular cation (150 mEq/L) and its concentration is much higher than in extracellular fluid. Such a high concentration of intracellular potassium is critical for activity of certain enzymes, electrical phenomena, muscle cell contraction, blood flow during exercise, and structural integrity. Hypokalemia may potentially cause rhabdomyolysis by 3 mechanisms. First, increased blood flow to the anaerobic muscle is mediated by release of intracellular potassium into the extravascular spaces; with hypokalemia, release of potassium may be inadequate to vasodilate arterioles and capillaries that perfuse the exercising muscle. Second, hypokalemia has been shown to suppress the synthesis and storage of glycogen, an intracellular store of energy substrate for the exercising muscle. Finally, deranged ion transport across the cell membrane has been demonstrated1.
Microscopic study of muscle biopsies of patients with hyperaldosteronism or pseudohyperaldosteronism and myopathy11 demonstrated difuse necrosis and vacuolitation of muscle fibres, infiltration of phagocytes and basophilic regenerating fibres in an acute stage of muscular weakness. Histological reactions revealed both type 1 and 2 muscular fibres damaged. Electron microscopic findings of necrotic muscle fibres were complete dissolution of myofilaments with disappearance of sarcoplasmic reticulum and T-tubules. Ultraestructures of non-necrotic muscle fibres demonstrated membrane-bound vacuoles, and dilatation of sarcoplasmic reticulum and widening of the T-tubules. These findings are similar to those found in a experimental study with potassium depleted dogs12.
Our patient had hypertension, hypokalemia, suppressed PRA, and increased aldosterone excretion, not suppressible by oral or intravenous salt overload, so the diagnosis of primary hyperaldosteronism was established. She did not respond to bipedestation with a physiological elevation of aldosterone and she had a 20×10 mm right adrenal mass, suggesting the existence of a APA. Anyway, she was 42-year old, and non-functioning unilateral adrenal macroadenomas are not uncommon, especially in patients older than 40 years3; so a bilateral adrenal venous sampling was performed to confirm that the origin of hyperaldosteronism was an APA. Correction of hypokalemia with oral and intravenous potassium supplements resolved rhabdomyolysis normalising CPK values, before hyperaldosteronism was treated with spironolactone or surgery. This support that the main cause of rhabdomyolysis was hypokalemia and not the direct effect of aldosterone. Gender and age characteristics of patients with rhabdomyolysis and primary hyperaldosteronism are similar to the ones of a recent report of primary hyperaldosteronism in hypertensive patients13, although we have found a difference in the age of presentation of rhabdomyolysis between men and women. All patients with rhabdomyolysis and primary hyperaldosteronism in whom the aetiology was reported had a APA. In contrast, one series of primary hyperaldosteronism showed an APA as the cause of PA in 42.8%, and IHA in the remaining 57.2% of patients13. Another study reported 20% of surgically confirmed APA and 8% of probable APA, while the remainder 72% were considered to have probable or confirmed IHA3. This finding is compatible with the fact that patients with APAs have more frequent hypokalemia, and higher concentrations of aldosterone, than those with IHA3. Half of the patients with rhabdomyolysis and primary hyperaldosteronism were treated with diuretics, and this could aggravate hypokalemia, precipitating rhabdomyolysis. This underlines the importance of measuring potassium levels before treating a hypertensive patient with diuretics.
Although rhabdomyolysis is not a common entity in patients with primary hyperaldosteronism, we think that CPK levels have to be determined in these patients, specially when serum potassium is lower than 2,5 mEq/L. When rhabdomyolysis occurs in a patient with hypokalemia and metabolic alkalosis, PA has to be suspected: if confirmed, an APA is the most probable cause.