The evaluation of a morbidly obese patient is challenging and many times, frustating for both the patients and their doctors. This article reviews some important issues, which should be taken into consideration when treating patients with morbid obesity.
La evaluación del paciente con obesidad mórbida es un reto que muy a menudo resulta frustrante, tanto para pacientes como para sus médicos. Este artículo revisa algunas cuestiones importantes que deberían tenerse en cuenta al tratar a los pacientes con obesidad mórbida.
It is estimated that 30% of adults in the United States of America (USA) are obese-defined as a body mass index (BMI) ≥ 30. Obesity is an epidemic in the USA and is emerging as a major health problem worldwide1. Complications of obesity include dyslipidemia, hypertension, type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), obstructive sleep apnea (OSA), degenerative joint disease, depression, and certain types of cancer. Individuals who are obese have an increased risk of mortality. In individuals who are severely obese (BMI ≥ 40), the risk of obesity-associated morbidities and mortality is even greater2-4. Morbid obesity is a condition that affects as much as 10% of the American population. There are approximately 4.5 million women and 3.5 million men who are classified as severely or morbidly obese, and this group represents one of the fastest growing trends in obesity within the USA. In some minorities, the percentage of individuals with a BMI > 40 exceeds 10%2.
Morbid obesity is also a social and economic problem; being obese is associated with a poor quality of life, and people with morbid obesity have, in many cases, limited selection in clothing, inability to ambulate, stress incontinence, and difficulty with personal hygiene. The social stigma of their obesity often makes it difficult for these people to find employment or a spouse. A direct consequence of social bias is an economic disadvantage with decreased monetary and educational opportunities.
Unfortunately, the future does not appear promising-extreme forms of obesity are rising even faster than the overall epidemic. Between 1986 and 2000, the prevalence of morbid obesity (BMI ≥ 40) quadrupled, and super obesity (BMI ≥ 50) increased 5-fold in adults in the USA. In Europe, although the problem of obesity is not as dramatic, its rate of growth is dangerously approaching these figures. Therefore, the chance of seeing a morbidly obese patient in our clinic is becoming more and more frequent5.
EVALUATION OF A MORBIDLY OBESE PATIENTThe evaluation of a morbidly obese patient is challenging and requires extra-time and patience by the clinician. Most likely these patients have been seen by several physicians before coming to our obesity/endocrine clinic; however, rarely have they received a detailed evaluation that addresses their main problem (morbid obesity) and its comorbidities. The reasons for such suboptimal evaluations are multifactorial. On the physician's side, the barriers include: lack of time, knowledge, and trust in weight loss medications. Many physicians do not consider obesity as a significant health problem and offer dietary counselling to only 25% to 50% of patients who need it. Patients also contribute to suboptimal care: lack of motivation, unwillingness to take responsibility for their health, lack of trust in physicians MDs, use of alternative weight loss methods, financial reasons (eating healthy is expensive), and frustration due to the feeling of "I have tried everything and nothing works".
The first step in evaluating a morbidly obese patient is to address his/her motivation for losing weight and to make sure they have a good understanding of the consequences of being overweight. If a patient comes to our clinic because of pressure from a partner or physician and he/she has little interest in losing weight, our visit (and effort) is not going to be effective and should be limited. In these circumstances it is important to make sure that our patient understands the risks of being morbidly obese. We should show them that we are willing to work with them side-by-side, developing a personalized health plan to address their general health and help them to slowly lose weight over time. Basically, we need to evaluate whether the patient is willing to start working with us or just wants to go home and continue with his/her routine. We should also be quick to address whether there are signs of depression (and frustration), which precludes the patient from taking any step forward. When the patient is interested and motivated to lose weight, we need to be ready to spend time listening and formulating the right questions.
An ideal interdisciplinary approach includes, at a mínimum, representatives from 4 specialities: medicine, nutrition, psychology-psychiatry and, in many circumstances, surgery. The team should evaluate the patient's health, treat conditions that require optimization and review the different therapeutic options. Our efforts, in addition to addressing their obesity and comorbidities, should be directed at developing a nutritional and life style program-which, should help the patient lose weight over time and to reduce the risk of comorbidities. In many circumstances our efforts will help to optimize patient status before a possible bariatric operation, and contribute to postoperative education and management.
Medical historyThe scope and focus of the comprehensive medical history should be designed to identify precipitating factors of obesity (eg, recent smoking cessation), a recent bone fracture or surgery, medications, changing jobs or marital status, etc. It is important to carry out a detailed evaluation with information related to medical, social and family history of obesity (ie, genetic impact), body weight changes, weight loss efforts, food preferences, eating habits and current level of physical activity. Details of the patient's weight history should be carefully documented since morbidly obese patients typically have had a lifelong struggle with failed weight loss attempts. It is not uncommon for patients to feel guilt or shame, for having a disease that society has associated with a lack of willpower and laziness. The clinician should include a record of weight loss medications and weight loss accomplished with the different weight loss programs.
A nutritional evaluation will assess food intake and identify eating triggers (eg, times of emotional upset). It is helpful to obtain a food diary during a 72-hour period–to develop perspectives on food preferences, meal patterns (eg, how many meals, when, where, with whom, duration), the presence of compulsive eating habits or bulimic behavior, and eating binges. It is important to get a sense of patient's level of physical activity and whether he/she is able to carry out any exercise at all. We should also address their difficulties (eg, physical, economical and social limitations) in carrying out the life style changes that we are asking them to slowly develop.
Not all physicians agree that morbidly obese patients should undergo a psycho-logical/psychiatric evaluation. Some clinicians order this consultation just to comply with the necessary requirements before a patient undergoes bariatric surgery. We personally feel that given the high prevalence of depression in morbidly obese patients, a large majority of them may benefit (and even wellcome) a psychologic evaluation. The focus of this mental health examination is on evaluating the possibility of eating disorders/behaviors (eg, binge eating disorder and night time eaters in particular), uncontrolled depression, significant stress, history of physical/sexual abuse and personality disorders. Assessment of mental status should be done by a psychologist or psychiatrist who is familiar with the psychological and emotional abnormalities common to the morbidly obese. In the case that the patient is a bariatric surgery candidate, the mental health professional also needs to confirm that the patient has realistic expectations of the surgery and that fully understands and accepts the postoperative lifestyle and behavioral changes that will be required. The strength of the patient's support network is especially important, given the high rates of marital and family problems that occur after bariatric surgery. Patients usually complete tests directed to evaluate their personality (eg, Minnesota Multiphasic Personality Inventory [MMPI]), psychological state (eg, Beck Depression Inventory [BDI, BDI-II]) and quality of life scale (eg, EuroQoL Scale). The data obtained through these evaluations will be helpful to get an idea of patient's general psychological status and his/her efforts, frustrations and expectations in relation to his/her body weight.
Very importantly, we need to address comorbid conditions and the status and possible complications of these comorbidities. A complete review of systems will help to identify medical problems that the patient has not mentioned. Areas of particular importance to morbidly obese patients are symptoms suggestive of comorbidities such as coronary artery disease, hypertension, T2DM, depression, thyroid disease, hypogonadism, cranial hypertension, polycystic ovarian syndrome, osteoarthritis and OSA. The Epworth Sleepiness Scale, screens for patients who will require polysomnography for the diagnosis of suspected OSA.
In general, patients with morbid obesity have been telling their doctors the consequences of being overweight: increased fatigue, shortness of breath, getting up tired, falling sleep easily, joint pain, headaches, and other multiples issues related to their diabetes, hypertension, dyslipidemia, osteoarthritis, asthma and the long list of medications they take because of these problems. They usually have been seeing different specialists to address their comorbidities such as hypertension, T2DM, gastro-esophageal reflux disorder (GERD), osteoarthritis, fibromyalgia, dyslipidemia, CAD, OSA, urinary incontinence, etc. However, clinicians are doing a poor job of actually listening to the patient with obesity–and missing an opportunity to address possible reasons/triggers responsible for their increased body weight and factors that may be precluding them from losing weight. Some of the questions that are usually not asked include:
- –
What are the highlights of your day?
- –
What makes you happy?
- –
How do you calm your anxiety and frustrations?
- –
How do you reward your successes?
- –
Do you walk to places?
- –
How many juices, sodas and ice creams do you take daily?
- –
Do you have friends?
- –
Do you live alone?
- –
How is your libido?
- –
Are you sexually active?
- –
Have you been abused during your life?
- –
Have you thought about killing yourself?
Sooner or later–in the course of a detailed evaluation–these questions should be asked.
Physical examAfter obtaining a detailed medical history, the clinician should perform a thorough physical examination. The examination should include body weight and height–so we can determine body mass index (BMI: weight measured in kilograms, divided by the square of height in meters)–and the abdominal circumference. Our exam should be helpful to evaluate possible causes (eg, Cushing's disease, hypogonadism, hypothyroidism, insulin resistance, etc.) as well as consequences (eg, cardiac insufficiency, hyperlipemia, diabetic neuropathy, etc.) of morbid obesity. We should pay particular attention to the oropharynx, body fat distribution, and abdominal girth. The presence of android (associated with increased cardiovascular risk) vs. gynoid fat distribution should be determined. Common findings on physical examination of patients who are morbidly obese, include a crowded oropharynx (often is a predictor of sleep apnea), distant cardiac and breath sounds, abdominal striae, intertrigo, acanthosis nigricans, tibial edema, osteoarticular tenderness, and signs of venous insufficiency. The physical examination will provide information about an important factor that we usually do not talk about: the level of personal hygiene of our patient. This issue can provide important information regarding family support, social life, and the patient's level of frustration.
Diagnostic evaluationThe physical examination should be followed by several laboratory tests and possibly medical consultations. A complete blood count with differential, metabolic panel, vitamin B12 and folate concentrations, thyroid panel, iron (iron binding capacity), lipid profile, Creactive protein (inflammatory marker related to CV risk), and urinalysis should be obtained on all patients. It is not unusual to find malnutrition in patients with morbid obesity (eg, cobalamine, iron, and folate deficits). It is also important to evaluate visceral protein by measuring albumin, prealbumin, transferrin, and retinol binding protein. Other hormone determinations such as testosterone, cortisol, and insulin may be ordered dependent on findings in the history and physical examination.
Measuring glycosylated hemoglobin (HbA1C) in patients with T2DM, and a thorough review of their home glycemic control, will be helpful for optimization of the diabetes-directed therapies. Common findings in patients who are morbidly obese include fatty infiltration of the liver, cholelithiasis, hiatal hernia, and GERD. An ultrasound of the abdomen (to assess for cholelithiasis, liver size, and steatosis), is routinely performed. Esophageal manometry and pH monitoring may also be considered when alteration in esophageal motility is suspected.
Cardiology, pulmonology, gastroenterology, and psychiatry consultations should be requested, dependent on individual patient needs. Based on the health history and physical examination findings, tests such as cardiac nuclear stress testing, echocardiography, poly-somnography, and endoscopy may be indicated. The possibility of CAD should be evaluated. Cardiovascular assessment, via stress imaging study such as echocardiography or nuclear imaging, should be considered in patients older than 50 years and in those whose obesity– related comorbidities (especially T2DM, hyper-cholesterolemia, and hypertension) have been present for more than 10 years. An electrocardiogram to assess, among other things, Q-Tc interval prolongation is also performed routinely. Administration of dobutamine is often needed to achieve target heart rates in patients with limited mobility. OSA is common in the severely obese, but is often overlooked or misdiagnosed as depression, fibromyalgia, or chronic fatigue syndrome. A recent study has shown that men with T2DM have a very high prevalence of OSA, much higher than that of men in the general population. A polysomnogram should be obtained in patients with loud snoring and documented apneic episodes, significant day-time somnolence, and/or early morning headache.
Patients will spend several days to weeks carrying out the different tests, procedures and consultations that we have indicated. We ought to continue to develop a personalized therapeutic plan, which should be reviewed and negotiated with the patient, from our first visit. It is beyond the scope of this review to go in detail over the different morbid obesity treatment options; however, we will give a brief overview of the current guidelines for the treatment of morbid obesity.
TREATMENT FOR MORBID OBESITYMost obese patients are counseled to modify diets and increase physical activity. Some are treated with pharmacological agents. Yet, for the severely obese, despite the fact that these interventions have not been rigorously tested, the general opinion is that they are not effective in maintaining long-term weight loss. Bariatric surgery is believed to be the most effective therapy available to induce weight loss in patients with morbid obesity. In 1991, a National Institutes of Health (NIH) Consensus Conference established the guidelines for the treatment of morbid obesity6.
The NIH panel defined surgical candidates as those with BMI greater than 40 (obesity of Class III) or greater than 35 in conjunction with severe comorbidities such as cardiopulmonary complications or severe T2DM, hypertension, osteoarthritis, hyperlipidemia, or sleep apnea. The panel made very clear recommendations that included:
- –
In most cases, morbidly obese patients should first be considered for treatment in a nonsurgical program with integrated components of a dietary regimen, appropriate exercise, and behavioral support and modification.
- –
A judgment of failed nonsurgical therapy should be followed by a decision for nonsurgical therapy in a different kind of program or with a different therapist, for no further therapy if significant comorbidities do not exist, or for surgical therapy.
- –
Patients who are candidates for the surgical procedures should be selected carefully after evaluation by a multi-disciplinary team with access to medical, surgical, psychiatric, and nutritional expertise.
- –
Patients should have an opportunity to explore with the physician any previously unconsidered treatment options and the advantages and disadvantages of each.
- –
The need for lifelong medical surveillance after surgical therapy should be made clear. With all of these considerations, the patient should be helped to arrive at a fully informed, independent decision concerning his or her therapy.
- –
A decision for surgical therapy should be reached only after assessment of the probability that the patient will be able to tolerate surgery without excessive risk and to comply adequately with the post-operative regimen.
- –
There must be full discussion with the patient of the probable outcome of the surgery.
- –
The operation should be carried out by a surgeon substantially experienced with adequate support for all aspects of perioperative management and assessment. Post-operative care, nutritional counseling, and surveillance should continue for an indefinitely long period.
The American Society for Metabolic and Bariatric Surgery (ASBS) convened a new Consensus Conference for Obesity Surgery at the Georgetown University Conference Center (Washington, DC) in May, 20047. This Consensus Statement was prepared to update the 1991 NIH Consensus Statement on "Gastrointestinal Surgery for Severe Obesity". Findings and conclusions of the Consensus Panel included:
- –
Bariatric surgery is the most effective therapy available for morbid obesity and can result in improvement or complete resolution of obesity-related comorbidities.
- –
The number of operative procedures for morbid obesity have increased since 1991 and are continuously evolving-there are currently 4 types of procedures that can be used to achieve sustained weight loss: gastric bypass (standard, long-limb, and very-long-limb Roux), alone or in combination with vertical banded gastroplasty; laparoscopic adjustable gastric banding; vertical banded gastroplasty; and biliopancreatic diversion and duodenal switch.
- –
Both open and laparoscopic bariatric operations are effective therapies for morbid obesity and represent complementary state-of-the-art procedures.
- –
Bariatric surgery candidates should have attempted to lose weight by non-operative means, including self-directed dieting, nutritional counseling, and commercial and hospital-based weight loss programs, but should not be required to have completed formal non-operative obesity therapy as a pre-condition for the operation.
- –
While the NIH mínimum requested BMI are essentially confirmed, extending bariatric surgery to patients with Class I obesity (BMI 30 to 34.9) who have a comorbid condition that can be cured or markedly improved by substantial and sustained weight loss may be warranted.
- –
The bariatric surgery patient is best evaluated and subsequently cared for by a multidisciplinary team.
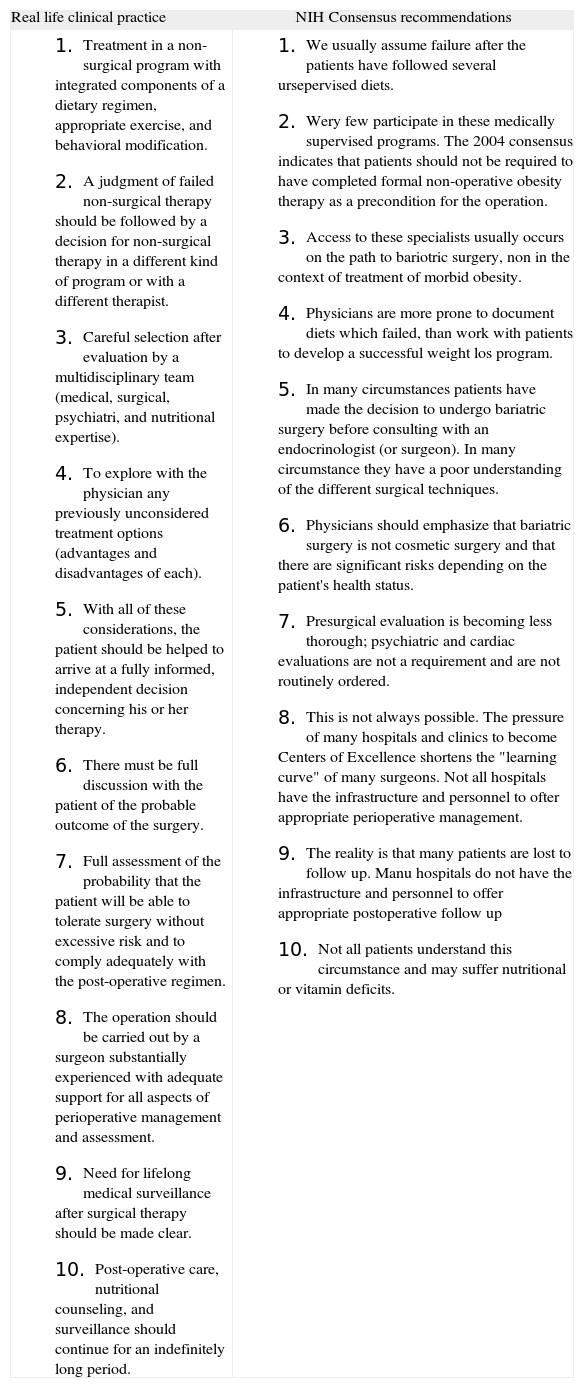
Physicians taking care of morbidly obese subjects would agree that there is poor compliance with some of these Consensus Recommendations8 (table 1). In general, the medical community believes that surgery may be/is the only effective treatment for severely obese individuals with acceptable operative risks and for moderately obese individuals, with high-risk comorbidities. The failure of medical treatment in this population is taken for granted. However, we need to keep in mind that this statement is not based on solid scientific evidence, since we lack prospective controlled studies evaluating the impact of an interdisciplinary medical weight loss treatment compared with a surgical treatment in patients with morbid obesity. In addition:
- –
The ASBS Consensus Statement itself overtly admits that few studies have specifically examined the effects of nonsurgical treatment in patients with morbid obesity, so conclusions about nonsurgical therapy in this population are based on inference.
- –
The large majority of morbidly obese patients have followed multiple types of diets. Even though we advise our patients that they should eat less and exercise more, very few of them follow a supervised interdisciplinary weight loss program including dieticians, exercise physiologist and psychiatric/psychologist and endocrinologist/ internist before being considered for bariatric surgery.
- –
In addition, few physicians have received formal training regarding treatment of obesity: only a limited number of medical professionals have acquired the knowledge necessary to prescribe nutritional regimes, behavior therapy programs or advice on physical activity and exercise. At the same time, the limited time of a medical consultation, does not make it possible to approach these topics, since they are generally deemed of minor importance, as much by the doctor as by the patient.
- –
The NIH-Consensus stated that experience with drug therapy for clinically severe obesity had been disappointing and only a short-term weight loss benefit had been shown. We need to take into account that the main drugs currently included in the obesity therapy armamentarium-and approved by Food and Drug Administration (FDA) for the treatment of obesity–were still not available in 1991 when these recommendations were outlined. It is important that a very few number of morbidly obese patients have ever tried FDA-approved weight loss medications such as orlistat or sibutramine, before undergoing bariatric surgery. The use of medications for the treatment of obesity has limited support both among patients and physicians and there are several possible explanations for this circumstance. The list of former weight loss medications such as amphetamines, thyroid hormone, and dexfenfluramine is remembered by the significant deleterious side effects associated with these medications. The current pharmacological armamentarium to treat obesity is scarce, unknow*n to many doctors and their coverage limited by medical insurances and by the Public Health Systems of many countries. These medicines, although effective in a significant number of patients, are not magic and require the association of dietary changes and increased physical activity, which patients are not eager to pursue. Also, morbidly obese patients usually take a large number of pills on a daily basis for their obesity comorbidities and are reluctant to increase the number of medications.
- –
Very few weight loss clinical trials have included patients with morbid obesity. This fact may be due in part to the morbid obesity comorbidities, which makes them less homogenous and more difficult to deal with, compared to obese patients with lower BMIs. Other reasons for the lack of clinical trials that include patients with morbid obesity, include social factors, such as reduced mobility and "fear of ridicule" that would limit the interest of morbidly obese patients in participating in a clinical trial with subsequent frequent visits to the hospital.
- –
An important issue that needs to be taken into account is that the prevalence of depression in the morbidly obese population has been reported to be ≈ 50%. However, in many circumstances clinicians that specialize in bariatric care, ask psychiatrists to evaluate these patients for bariatric surgery clearance on their path towards surgery; rather than addressing and treating their depression/anxiety in an effort to evaluate the impact of this treatment on their appetite and body weight. The 2004 ASBS Consensus Conference is even less strict and recommends that "evaluations by subspecialists such as psychiatrists, psychologists are not routinely needed but should be available if indicated". Again, the failure of nonsurgical treatment is taken for granted.
- –
In general, physicians feel quite frustrated when dealing with patients with morbid obesity. The lack of clinic time, appropriate medical tools, and qualified team support contributes to this frustration. The possibility of referring patients to bariatric surgery has served in many cases as an escape-valve for this situation. The 1991 NIH Consensus recommended "first to consider treatment in a nonsurgical program with integrated components of a dietary regimen, appropriate exercise, and behavioral support; modification and judgment of failed nonsurgical therapy should be followed by a decision for non-surgical therapy in a different kind of program or with a different therapist, for no further therapy if significant comorbidities do not exist, or for surgical therapy". However the 2004 ASBS Consensus stated that bariatric surgery candidates "should have attempted to lose weight by non-operative means, but should not be required to have completed formal nonoperative obesity therapy as a precondition for the operation". This amendment contributes to facilitating the access to bariatric surgery without a thorough medical therapy approach. We should not forget that this Consensus Conference was promoted by a surgical society. A recent consensus document by the American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery further reviews these recommendations9.
- –
In countries with socialized medicine, where the waiting list for bariatric surgery could be 6 to 24 months, the frustration is significant. Interestingly, the patients waiting for bariatric surgery theoretically offer a good opportunity to evaluate new medical strategies for morbid obesity–even if, unfortunately, little motivation towards a serious medical approach is to be expected in a patient who is waiting for surgical therapy.
- –
The NIH Consensus advised that patients should be helped to arrive at a fully informed, independent decision concerning their therapy. It seems that in many circumstances patients have a poor understanding of the different surgical techniques and how it will impact their lives after surgery. Circumstances, such as a history of previous right colon surgery, history of GERD, poor tolerance to flatulence, financial status, which could help to decide which surgery would more indicated. However, the reality is that geographic factors and surgical expertise may be the most determinants regarding which type of surgical procedure a specific patient will undergo.
- –
There is clear scientific evidence for the habits necessary for successful long-term weight loss after bariatric surgery (gastric bypass surgery). Cook and colleagues10 reported that successful patients ate 3 well-balanced meals and 2 snacks per day. They drank water and did not drink carbonated beverages. Seventy-four percent of them did not drink alcoholic beverages and 55% did not drink juices or sweetened beverages. They exercised regularly to maintain their weight; the average was 4 times a week for at least 40 min. Patients reported exercise as a key factor in their ability to maintain their weight. Patients that were successful took personal responsibility for staying in control. They took daily multiple vitamins, calcium and iron if needed and slept an average of 7 hours per night. Seventy-six percent rated their personal energy as being average or high. Surgery was only a tool they used to reach and maintain a healthy weight. These findings emphasize the need to develop medical tools which can be used in many circumstances, instead of bariatric surgery. The challenge is to provide morbidly obese patients with all the necessary support and tools to start developing healthy habits during a period of time before they undergo bariatric surgery. The question that remains unanswered is: how many of these patients would do well, without the need of undergoing bariatric surgery?
National Institutes of Health Consensus Recommendations before undergoing bariatric surgery vs real life clinical practice
| Real life clinical practice | NIH Consensus recommendations |
|
|
Fondo de Investigación Sanitaria (FIS -PI071250-), Instituto de Salud Carlos III, Ministerio de Ciencia e Innovación and Mutua Madrileña Medical Foundation.