Complications of diabetes comprise the leading cause of death in Mexico. We aimed to describe the characteristics of management and achievement of therapeutic targets in Mexican patients with diabetes mellitus.
MethodsWe analyzed data from 2642 Mexican patients with type 1 (T1D, n=203, 7.7%) and type 2 diabetes (T2D, n=2439, 92.3%) included in the third wave of the International Diabetes Management Practices Study.
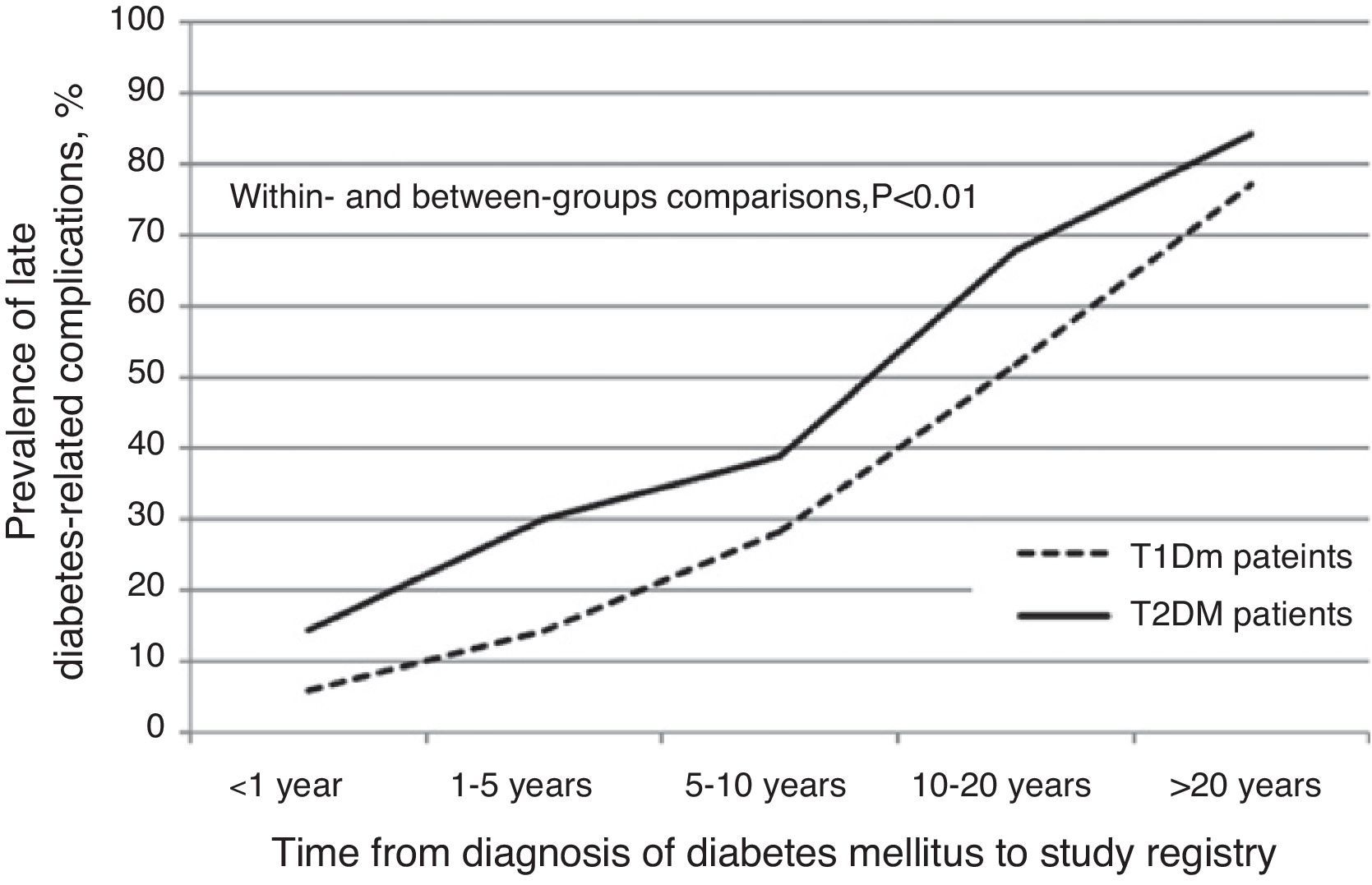
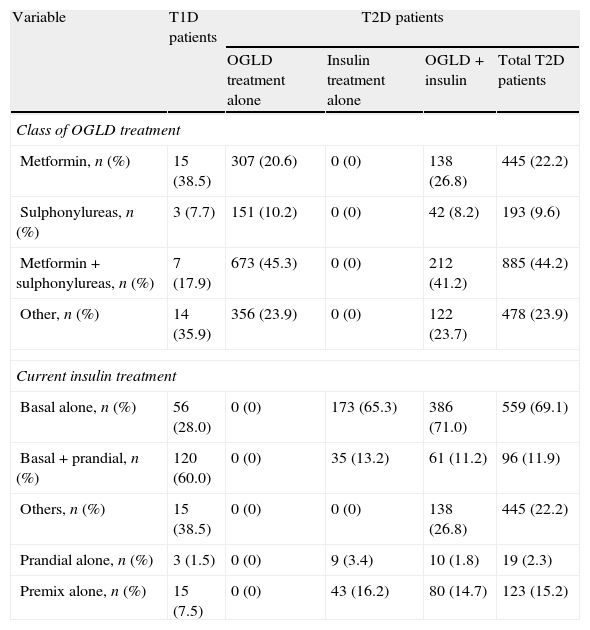
ResultsOf T2D patients, 63% were on oral glucose-lowering drugs (OGLD) exclusively (mostly metformin), 11% on insulin, 22% on OGLD plus insulin, and 4% on diet and exercise exclusively. T2D patients on insulin were more likely to be trained on diabetes, but they were older, had worse control, longer disease duration and more chronic complications than patients on OGLD only. Glycated hemoglobin (HbA1c)<7% was achieved by 21% and 37% of T1D and T2D patients, respectively. Only 5% of T1D and 3% of T2D attained the composite target of HbA1c<7%, blood pressure<130/80mmHg and low-density lipoprotein cholesterol<100mg/dl. T1D patients had less macrovascular but more microvascular complications, compared with T2D patients. Late complications increased with disease duration, so that about 80% of patients after 20 years of diagnosis have at least one late complication. Reaching the target HbA1c<7% was associated with a reduced number of microvascular but not with less macrovascular complications.
ConclusionA great proportion of these Mexican patients with diabetes did not reach therapeutic targets. Insulin was used mostly in complicated cases with advanced disease.
Las complicaciones de la diabetes suponen la primera causa de muerte en México. Nuestro propósito fue describir las características del tratamiento y el alcance de objetivos terapéuticos en mexicanos con diabetes mellitus.
MétodosAnalizamos datos de 2.642 mexicanos con diabetes mellitus tipo 1 (DT1, n=203; 7,7%) y tipo 2 (DT2, n=2.439; 92,3%), quienes fueron incluidos en la tercera fase del registro International Diabetes Management Practices Study.
ResultadosDe los pacientes con DT2, el 65% recibían tratamiento con hipoglucemiantes orales (HO) exclusivamente (principalmente metformina), el 11% insulina, el 22% HO más insulina, y el 4% dieta y ejercicio exclusivamente. Los pacientes con DT2 tratados con insulina habían recibido más educación en diabetes, pero eran más añosos, con peor control, mayor duración de la enfermedad y más complicaciones crónicas que los pacientes tratados con HO solamente. Una hemoglobina gucosilada (HbA1c)<7% fue alcanzada por el 21 y el 37% de los pacientes con DT1 y DT2, respectivamente. Solo el 5% de los pacientes con DT1 y el 3% con DT2 alcanzaron el objetivo compuesto de una HbA1c<7%, una presión arterial<130/80mmHg y colesterol ligado a lipoproteínas de baja densidad<100mg/dl. Los pacientes con DT1 tenían menos complicaciones macrovasculares, pero más microvasculares en comparación con pacientes con DT2. Las complicaciones crónicas aumentaron con la duración de la enfermedad, de tal manera que cerca del 80% de los pacientes después de 20 años de diagnóstico tenían al menos una complicación crónica. El objetivo de HbA1c<7% se asoció a una frecuencia menor de complicaciones microvasculares, pero no con menos macrovasculares.
ConclusionesUna gran proporción de estos pacientes mexicanos con diabetes no alcanzaron los objetivos terapéuticos. El tratamiento con insulina se empleó principalmente en casos complicados con enfermedad avanzada.
Diabetes mellitus is a growing health and social problem worldwide, especially in low-income countries, where the economical and cultural transition toward a lifestyle of excessive energy intake and low energy expenditure is taking place.1–7 The prevalence of diabetes mellitus in Mexican adults is 14.4%, with about 50% new cases diagnosed during population screening.8 This frequency is higher than that of the total Latin American population.6
Optimized care reduces acute and long-term complications, while improving quality of life9–17; but despite evidence-based guidelines, it is precisely in developing countries where diabetes is diagnosed late and standards of care are not completely followed as recommended.1–6 There is scarce information about contemporary clinical care delivered to patients with diabetes in developing countries,1,2 which may represent a barrier in designing co-founded efforts aimed to improve the way these nations deal with diabetes burden.5 The International Diabetes Management Practices Study (IDMPS) is an ongoing 5-year survey designed to provide information regarding clinical practice and care delivered to patients with type 1 (T1D) and type 2 diabetes mellitus (T2D) in developing countries.1,2 The main objective is to document changes in clinical practice over a 5-year period, starting in November 2005, and organizing recruitment in 5 waves (every 12 months each). The aim of the present report is to describe the characteristics of the medical care delivered to Mexican patients with diabetes mellitus included in the 2007 registry (3rd wave) of IDMPS. We also describe the prevalence of micro and macrovascular complications, according to the type of treatment.
MethodsStudy designIDMPS is an international, multicenter, prospective, observational study on patients with T1D and T2D. The design of this survey is in accordance to STROBE guidelines, as described elsewhere.1,2 Briefly, IDMPS is composed of 5 cross-sectional registries (operationally called “waves”) in a 5-year period to assess changing practices in the management of subjects with diabetes mellitus. Each wave consists of two phases: a 2-week cross-sectional registry and a 9-month longitudinal survey. A 3-month interval separates the end of the longitudinal survey and the start of the next wave. Only data on the cross-sectional registry are analyzed in the present report. The number of subjects to be recruited in each participating country is determined on a country basis. Based on the assumption that insulin is the least prescribed therapy, the sample is determined in order to establish the frequency of insulin-treated patients.1,2 Physicians were invited to participate with a maximum of 10 patients with T2D and 5 with T1D. A total of 200 Mexican physicians participated in the 2007 wave. Physicians were invited to participate if they had experience using insulin and treating both T1D and T2D patients. From five to eight physicians pertaining to each of the 31 Mexican States were invited to participate, depending on the population density, but stratification of the States population was not performed to calculate sample size. The internal Committee of Ethics of each participating center reviewed and approved patient enrollment.
Participation criteriaMale and female patients ≥18 years of age diagnosed with either T1D or T2D, visiting the physician during the recruitment period of the cross sectional phase, could be selected to enter the study. Patient selection was not randomly assigned. Written informed consent was required for all patients. Patients were excluded if they had concomitant participation in another clinical descriptive or interventional study, if they participated in a previous wave of IDMPS, or if they were under temporary insulin treatment (gestational diabetes, surgery, pancreas cancer, sepsis and other conditions).
Data collectionInformation was collected on standardized electronic and hard case report forms (CRFs) about demographics, medical history, pharmacologic and lifestyle therapy, glycemic control (fasting glucose and glycated hemoglobin (HbA1c)) and other therapeutic targets such as blood pressure, low density lipoprotein cholesterol (LDL-C), albuminuria, blood glucose self-monitoring, access to diabetes education, access to specialized care, hospitalizations, medical complications (i.e., diabetic neuropathy, cataracts, retinopathy, renal insufficiency, heart failure, myocardial infarction, stroke, peripheral artery disease and diabetic foot ulcer) and work absenteeism, among other variables. The participating physicians filled data in the paper CRF. The filled CRF was sent to the Sanofi-Aventis data management affiliate that reviewed every CRF for consistency and completeness. Every CRF was registered in a web-based data capture system. Any conflicting information and query was returned to the participating physician for clarification. Blood pressure measurements and laboratory analyses registered were those practiced locally by each participating physician with standard procedures. No central laboratory testing was utilized. Blood pressure was measured in the physician's office with a sphygmomanometer with participants seated after 5min of rest, in the right arm at the heart level. Blood pressure (BP) was measured twice, each 5min apart. A third measurement was made if the blood pressures differed by more than 10mmHg in systolic and 5mmHg in diastolic readings. Diabetes-related complications were documented by a competing specialist, depending on the particular complication (an ophthalmologist for eye complications, a cardiologist for coronary heart disease, a neurologist for cerebrovascular disease and diabetic neuropathy, and a vascular surgeon for peripheral artery disease). These specialists were invited at the discretion of the IDMPS participating physician for the evaluation of possible diabetes-related complications exclusively.
Statistical analysisParametric continuous variables are expressed as geometric means and standard deviations (SD), or minimum and maximum. Categorical variables are expressed as percentages. Student's t test was performed to compare quantitative variables parametrically distributed between two groups. Chi-square statistics were used to compare nominal variables in univariate analyses. All p values are two-sided and regarded as significant when p<0.05. Statistical analyses were conducted with the SAS Software version 8.02.
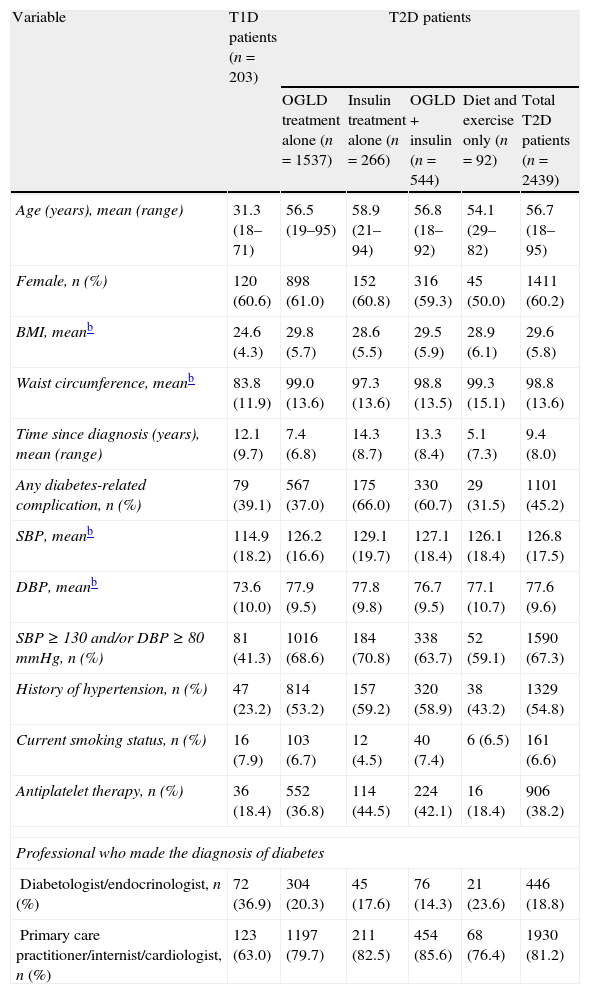
ResultsIn Mexico, 3052 patients with diabetes were recruited in 2007 (IDMPS 3rd wave) by 200 physicians: 58 endocrinologists/diabetologists, and 57 primary care practitioners/internists/cardiologists. A total of 2642 (87%) patients met the eligibility criteria: 203 T1D (60.6% women, mean age 31.26, range 18–71; 76.8% aged<40 years) and 2439 T2D patients (60.2% women, mean age 56.7, range 18–95; 9.3% aged<40 years) (Table 1). A total of 91% of T1D and 89% of T2D patients pertained to urban areas. The characteristics of drug therapy are shown in Table 2.
General characteristics of type 1 and type 2 diabetic patients included in the IDMPS 3rd wave (n=2642) according to type of treatment.a
| Variable | T1D patients (n=203) | T2D patients | ||||
| OGLD treatment alone (n=1537) | Insulin treatment alone (n=266) | OGLD+insulin (n=544) | Diet and exercise only (n=92) | Total T2D patients (n=2439) | ||
| Age (years), mean (range) | 31.3 (18–71) | 56.5 (19–95) | 58.9 (21–94) | 56.8 (18–92) | 54.1 (29–82) | 56.7 (18–95) |
| Female, n (%) | 120 (60.6) | 898 (61.0) | 152 (60.8) | 316 (59.3) | 45 (50.0) | 1411 (60.2) |
| BMI, meanb | 24.6 (4.3) | 29.8 (5.7) | 28.6 (5.5) | 29.5 (5.9) | 28.9 (6.1) | 29.6 (5.8) |
| Waist circumference, meanb | 83.8 (11.9) | 99.0 (13.6) | 97.3 (13.6) | 98.8 (13.5) | 99.3 (15.1) | 98.8 (13.6) |
| Time since diagnosis (years), mean (range) | 12.1 (9.7) | 7.4 (6.8) | 14.3 (8.7) | 13.3 (8.4) | 5.1 (7.3) | 9.4 (8.0) |
| Any diabetes-related complication, n (%) | 79 (39.1) | 567 (37.0) | 175 (66.0) | 330 (60.7) | 29 (31.5) | 1101 (45.2) |
| SBP, meanb | 114.9 (18.2) | 126.2 (16.6) | 129.1 (19.7) | 127.1 (18.4) | 126.1 (18.4) | 126.8 (17.5) |
| DBP, meanb | 73.6 (10.0) | 77.9 (9.5) | 77.8 (9.8) | 76.7 (9.5) | 77.1 (10.7) | 77.6 (9.6) |
| SBP≥130 and/or DBP≥80mmHg, n (%) | 81 (41.3) | 1016 (68.6) | 184 (70.8) | 338 (63.7) | 52 (59.1) | 1590 (67.3) |
| History of hypertension, n (%) | 47 (23.2) | 814 (53.2) | 157 (59.2) | 320 (58.9) | 38 (43.2) | 1329 (54.8) |
| Current smoking status, n (%) | 16 (7.9) | 103 (6.7) | 12 (4.5) | 40 (7.4) | 6 (6.5) | 161 (6.6) |
| Antiplatelet therapy, n (%) | 36 (18.4) | 552 (36.8) | 114 (44.5) | 224 (42.1) | 16 (18.4) | 906 (38.2) |
| Professional who made the diagnosis of diabetes | ||||||
| Diabetologist/endocrinologist, n (%) | 72 (36.9) | 304 (20.3) | 45 (17.6) | 76 (14.3) | 21 (23.6) | 446 (18.8) |
| Primary care practitioner/internist/cardiologist, n (%) | 123 (63.0) | 1197 (79.7) | 211 (82.5) | 454 (85.6) | 68 (76.4) | 1930 (81.2) |
BMI, body mass index; DBP, diastolic blood pressure; OGLD, oral glucose lowering drugs; SBP, systolic blood pressure; T1D, type 1 diabetes mellitus; T2D, type 2 diabetes mellitus.
Drug therapy of type 1 and type 2 diabetic patients included in the IDMPS 3rd wave (n=2642).a
| Variable | T1D patients | T2D patients | |||
| OGLD treatment alone | Insulin treatment alone | OGLD+insulin | Total T2D patients | ||
| Class of OGLD treatment | |||||
| Metformin, n (%) | 15 (38.5) | 307 (20.6) | 0 (0) | 138 (26.8) | 445 (22.2) |
| Sulphonylureas, n (%) | 3 (7.7) | 151 (10.2) | 0 (0) | 42 (8.2) | 193 (9.6) |
| Metformin+sulphonylureas, n (%) | 7 (17.9) | 673 (45.3) | 0 (0) | 212 (41.2) | 885 (44.2) |
| Other, n (%) | 14 (35.9) | 356 (23.9) | 0 (0) | 122 (23.7) | 478 (23.9) |
| Current insulin treatment | |||||
| Basal alone, n (%) | 56 (28.0) | 0 (0) | 173 (65.3) | 386 (71.0) | 559 (69.1) |
| Basal+prandial, n (%) | 120 (60.0) | 0 (0) | 35 (13.2) | 61 (11.2) | 96 (11.9) |
| Others, n (%) | 15 (38.5) | 0 (0) | 0 (0) | 138 (26.8) | 445 (22.2) |
| Prandial alone, n (%) | 3 (1.5) | 0 (0) | 9 (3.4) | 10 (1.8) | 19 (2.3) |
| Premix alone, n (%) | 15 (7.5) | 0 (0) | 43 (16.2) | 80 (14.7) | 123 (15.2) |
NPH, neutral protamine Hagedorn; OGLD, oral glucose lowering drugs; T1D, type 1 diabetes mellitus; T2D, type 2 diabetes mellitus.
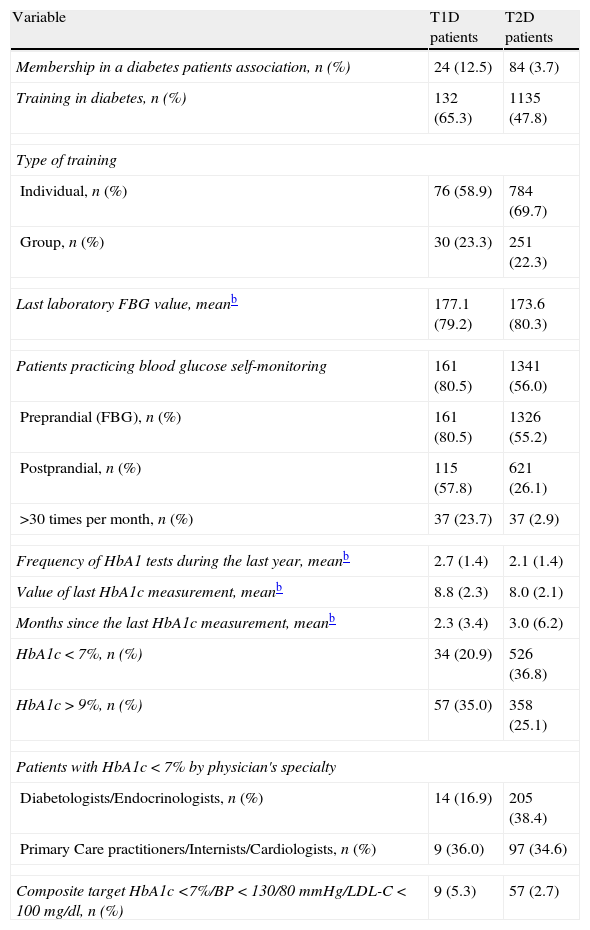
T2D patients under insulin treatment were more frequently trained on diabetes than patients on OGLD alone, and more frequently trained than patients managed with diet and exercise only (Table 3). Moreover, T1D patients were more likely to have formal education on diabetes than did T2D patients (p<0.05). T1D patients had a mean (SD) of 6 (3.5) laboratory testings for fasting blood glucose (FBG), while T2D patients had a mean (SD) of 5.5 (7.5) measurements. Among T1D patients, 84% had a personal glucometer at home as compared with 56.9% of T2D patients (p<0.001). T2D patients treated with diet and exercise exclusively had the lower rate of self-monitoring. Only 20.9% of T1D patients and 36.8% of T2D patients had attained the target value of HbA1c<7% at the time of the registry (Table 3). Only 4% of the whole population had attained the 3-goal target of HbA1c<7% plus BP<130/80mmHg plus LDL-C<100mg/dl (2.7% in T2D and 5.3% in T1D patients, p<0.001).
Patients’ education on diabetes, screening for complications and achievement of therapeutic goals according to the type of diabetes mellitus.a
| Variable | T1D patients | T2D patients |
| Membership in a diabetes patients association, n (%) | 24 (12.5) | 84 (3.7) |
| Training in diabetes, n (%) | 132 (65.3) | 1135 (47.8) |
| Type of training | ||
| Individual, n (%) | 76 (58.9) | 784 (69.7) |
| Group, n (%) | 30 (23.3) | 251 (22.3) |
| Last laboratory FBG value, meanb | 177.1 (79.2) | 173.6 (80.3) |
| Patients practicing blood glucose self-monitoring | 161 (80.5) | 1341 (56.0) |
| Preprandial (FBG), n (%) | 161 (80.5) | 1326 (55.2) |
| Postprandial, n (%) | 115 (57.8) | 621 (26.1) |
| >30 times per month, n (%) | 37 (23.7) | 37 (2.9) |
| Frequency of HbA1 tests during the last year, meanb | 2.7 (1.4) | 2.1 (1.4) |
| Value of last HbA1c measurement, meanb | 8.8 (2.3) | 8.0 (2.1) |
| Months since the last HbA1c measurement, meanb | 2.3 (3.4) | 3.0 (6.2) |
| HbA1c<7%, n (%) | 34 (20.9) | 526 (36.8) |
| HbA1c>9%, n (%) | 57 (35.0) | 358 (25.1) |
| Patients with HbA1c<7% by physician's specialty | ||
| Diabetologists/Endocrinologists, n (%) | 14 (16.9) | 205 (38.4) |
| Primary Care practitioners/Internists/Cardiologists, n (%) | 9 (36.0) | 97 (34.6) |
| Composite target HbA1c <7%/BP<130/80mmHg/LDL-C<100mg/dl, n (%) | 9 (5.3) | 57 (2.7) |
BP, blood pressure; FBG, fasting blood glucose; HbA1c, glycosylated hemoglobin A1c; LDL-C, low-density lipoprotein cholesterol; T1D, type 1 diabetes mellitus; T2D, type 2 diabetes mellitus.
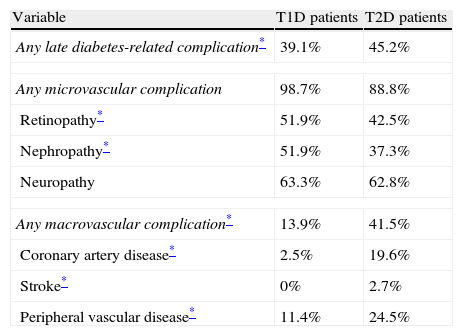
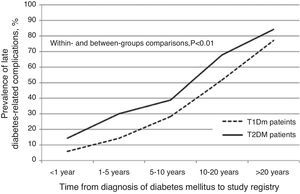
Any late diabetes-related complication was registered for 39.1% of T1D patients and 45.2% of T2D cases (p=0.01). Among T1D patients with ≥1 late complication, 98.7% had at least one microvascular and 13.9% at least one macrovascular complication. In contrast, among T2D patients who had at least one late complication, 88.8% had at least one microvascular and 41.5% at least one macrovascular complication (Table 4). There was a direct relationship between the number of late complications and time since diagnosis of diabetes (Fig. 1). In T1D patients, no significant differences were observed in the prevalence of micro or macrovascular complications grouped or analyzed separately with respect to a target HbA1c (all late complications: 26.5% vs. 43.4%, for patients with HbA1c<7% or ≥7%, respectively; p=0.17). On the other hand, in T2D patients, both micro and macrovascular complications were more frequent among patients not reaching the HbA1c target, than in those attaining this goal (all complications: 49.4% vs. 34.0%, for patients with HbA1c<7% or ≥7%, respectively; p<0.001). Furthermore, microvascular complications were significantly less frequent in T2D patients achieving the HbA1c target than those uncontrolled (84.9% vs. 91.2%, for patients with HbA1c<7% or ≥7%, respectively; p=0.02); however, the number of macrovascular complications did not differ between patients reaching or not reaching the target of HbA1c<7% (37.4% vs. 39.3%, for patients with HbA1c<7% or ≥7%, respectively; p=0.66).
Late complications in type 1 and type 2 diabetic patients (n=2527).
| Variable | T1D patients | T2D patients |
| Any late diabetes-related complication* | 39.1% | 45.2% |
| Any microvascular complication | 98.7% | 88.8% |
| Retinopathy* | 51.9% | 42.5% |
| Nephropathy* | 51.9% | 37.3% |
| Neuropathy | 63.3% | 62.8% |
| Any macrovascular complication* | 13.9% | 41.5% |
| Coronary artery disease* | 2.5% | 19.6% |
| Stroke* | 0% | 2.7% |
| Peripheral vascular disease* | 11.4% | 24.5% |
T1D, type 1 diabetes mellitus; T2D, type 2 diabetes mellitus.
We confirmed previous observations about the wide gap between current standards and care delivered to Mexican patients with diabetes mellitus.4,5 Even when IDMPS included mostly physicians familiarized with insulin therapy, in T2D patients this option is still reserved for long-lasting and complicated cases, mainly patients in whom lifestyle modifications and OGLD therapy had failed. And worryingly, a significant proportion of patients with T1D were treated with OGLD in combination with insulin, a strategy not supported in current recommendations. In this study only a minority of patients with diabetes mellitus had the recommended target value of HbA1c<7%. In contrast, in high-income nations a transition toward better practice and quality of care delivered to patients with diabetes has been observed in the last years.18 A USA study on 1334 T1D and T2D patients included in the National Health and Nutrition Examination Survey (NHANES) 1999–2004 documented that in the period 1999–2000 an unadjusted 37% of this population had HbA1c<7%, increasing to 56.8% in the period 2003–2004.17 A similar picture is observed in European countries.19,20 For example, the 10-year Spanish observational study RedGEDAPS has clearly shown an improvement in patient control and achievement of therapeutic goals with a significant reduction in late complication from 1996 to 2007. In contrast, low-income nations from Latin America, Eastern Europe and Asia have a frequency of patients being at therapeutic goals that is comparable with the figures provided in the present Mexican report.1 In general, in low-income countries insulin therapy and cardiovascular disease prevention are installed late and management of non-glycemic goals (chiefly lipids and blood pressure) are usually reserved for a “second step” after glycemic control is achieved. Unfortunately, the latter objective is never achieved in many cases.
Current scientific evidence has shown a direct relationship between HbA1c and microvascular complications.16 However, randomized trials have failed in demonstrating that stringent glycemic control reduces the risk of macrovascular complications.13–15 This emphasizes the need for a better management of non-glycemic therapeutic goals. Very similar conclusions have been obtained for the case of tight blood pressure control in two recent studies on patients with diabetes who already have coronary artery disease.21,22 Less stringent goals may be appropriate for certain subgroups of patients.23 That cardiovascular disease is not sufficiently delayed in most patients with diabetes only demonstrates the necessity of action in early stages, before irreversible vascular injuries accrue.24–26 This notion is in part supported by the observation that primary prevention of arterial thrombotic disease with antiplatelet therapy (an strategy that prevents thrombosis in an already damaged endothelium) provides no net clinical benefit in diabetic patients without other cardiovascular risk factors.26 Therefore, redoubled efforts are needed to reduce the immense health, social and economical burden that is imposed by diabetes around the world.27–30
The main limitations of this study are the cross-sectional design, the lack of standardized laboratory assays29, lack of standardized assessments of diabetes-related complications and the lack of random selection for both participating physicians and their patients. Nevertheless, this study highlights the need for a more aggressive attitude in delivering of care to patients with diabetes in Mexico. These data provide important basis for immediate institutional actions toward improvement of management of patients with the most important chronic disease in Mexico. There is a need for more studies evaluating international recommendations adequacy in developing countries.28
Conflicts of interestJulieta de la Luz, MD: employee of Sanofi-Aventis, Medical Area.
This registry received unrestricted funds from Sanofi-Aventis. The company designed and partially conducted and monitored the study; nonetheless, the company did not participate in the selection of patients, data capture, data analysis, manuscript draft or the decision to summit for publication.
The authors are indebted to all IDMPS-3W collaborators in Mexico (in alphabetic order) as follows: Acevedo G., Acosta I., Alpízar M., Altamirano E., Álvarez A., Álvarez P., Anaya C., Arellano S., Arreola M., Arroyo A., Arteaga V., Ascensión D., Baeza B., Bancalari C., Baqueiro J., Barón D., Barragán A., Barrientos M., Bastidas M., Bautista J., Beltrán L., Blanco A., Caballero S., Calarco E., Calderón R., Camacho L., Cano R., Caracas N., Cardoso S., Carrillo P., Carvajal M., Casco S., Castañeda R., Castelán F., Castillo O., Cerda I., Cervantes A., Chávez M., Chávez L., Chavira I., Cilia J., Cisneros H., Colín M., Collado E., Colome J., Conrado S., Correa A., Covarrubias M., Cruz E., Dávila O., De la garza N., Del pozo J., Díaz E., Domínguez C., Encinas E., Escalante A., Escalante J., Escalante M., Escudero I., Espinoza J., Estrada A., Estrada K., Fabián M., Fanghanel G., Farjat J., Fernández A., Flores M., Flores V., Franco M., Franco V., Gallardo V., Gamboa F., Garcia H., Garcia J., Garcia L., Garcia J., García P., Garza R., Gomez V., Gonzalez A., Gonzalez G., Gonzalez I., González A., Granillo M., Grover F., Guajardo M., Guerrero J., Gutierrez M., Guzmán J., Guzmán A., Hall J., Hamilton L., Handall V., Hernandez A., Hernandez F., Hernández A., Hernández J., Herrera L., Herrera M., Hinojos L., Ibáñez M., Ibarra A., Ibarra M., Jiménez M., Jurado M., Lavalle F., Lechuga D., Llanas D., Lopez S., López H., López R., Lozano J., Lucio F., Luna R., Macedo N., Macías A., Magallanes F., Maldonado D., Maldonado J., Mancillas L., Mar F., Marquez E., Martínez A., Martínez R., Martínez R., Matildes M., Mauricio G., Mejía A., Mejía J., Mejía L., Mejía M., Mendoza E., Mendoza P., Mercado F., Meza E., Moctezuma J., Moleres J., Monreal R., Montemayor D., Monterrubio N., Montoya J., Mora F., Morales D., Morales F., Morales M., Moreno F., Moreno L., Moreno M., Muñoz A., Muñoz T., Navalles E., Nevares L., Nevarez L., Niño J., Núñez A., Ochoa A., Olmedo V., Ortega A., Osorio D., Ovando R., Parra F., Pascoe S., Pérez C., Pérez H., Pérez N., Quezada M., Radillo P., Rajme V., Ramírez B., Ramírez J., Ramos L., Ramos M., Ríos E., Rivera E., Robles J., Rodriguez H., Rodriguez J., Rodriguez J., Rodriguez J., Rodríguez H., Rodríguez R., Romero A., Rosado C., Rosas M., Rosiles S., Rubio Y., Ruiz D., Ruiz E., Saavedra E., Salas R., Salazar H., Salinas S., Sanchez B., Sanchez H., Sanchez L., Sanchez R., Sanchez S., Sanchez S., Sanchez B., Sandoval R., Sandoval B., Santibáñez M., Seamanduras L., Secchi N., Solís T., Sosa A., Taméz H., Tapia M., Téllez J., Torres J., Torres E., Torres P., Trasviña K., Trejo M., Triano A., Triano M., Uribe A., Vadillo M., Valdez M., Valdovinos S., Valencia H., Vales M., Valladares Z., Vargas M., Vázquez J., Vázquez J., Vázquez J., Vázquez P., Vidrio M., Villanueva S., Wakida H., Yamamoto J., Zamora A., Zayas F.