Early diagnosis of diabetes mellitus complications reduces their progression and therefore improves quality of life and decreases cardiovascular mortality.
ObjectivesTo evaluate the efficiency of a unit for detection of chronic complications of diabetes, and to analyze the incidence and prevalence of complications in a sample of patients from our area of interest and concern.
MethodsA cross-sectional study performing routine screening of all diabetes complications in patients aged 18–80 years diagnosed with type 1 or type 2 diabetes mellitus at least 6 months before. Anthropometric variables were measured and data on drug treatment and the most recent lipid profile were collected.
Results460 patients were included in the study. The prevalence and incidence rates of chronic complications of diabetes were 57% and 35.4% respectively. Glycosylated hemoglobin values≤7% were found in 42% of patients, blood pressure levels below 130/80mmHg in 20% of patients, and LDL cholesterol levels less than 2.59mmol/L in 46% of patients. Patients with new complications were older and had higher BMI and hip circumference values, as well as higher systolic blood pressure levels and greater use of antihypertensive drugs.
ConclusionA unit for routine screening of chronic complications of diabetes would allow for detection of macroangiopathy and microangiopathy in a single annual visit, increasing visit compliance, and for implementation of measures to prevent its progression.
El diagnóstico precoz de las complicaciones crónicas de la diabetes mellitus permite reducir la progresión de las mismas y, por tanto, mejorar la calidad de vida y disminuir la mortalidad cardiovascular.
ObjetivosEvaluar la eficiencia de una unidad de detección de complicaciones crónicas de la diabetes y analizar la incidencia y prevalencia de las mismas en una muestra de pacientes de nuestra área de referencia.
Material y métodosEstudio transversal en el que se realizó un despistaje de todas las complicaciones de la diabetes a pacientes de entre 18 y 80 años con diabetes mellitus tipo 1 o 2 diagnosticadas más de 6 meses antes. Se midieron variables antropométricas y se recogieron datos sobre el tratamiento farmacológico y el último perfil lipídico.
ResultadosSe incluyeron 460 pacientes. La prevalencia de complicaciones crónicas fue del 57%. La incidencia fue de un 35,4%. Un 42% de los pacientes presentaron una hemoglobina glucosilada ≤7%, un 20% de pacientes presentaron niveles de presión arterial inferiores a 130/80mmHg y un 46% presentaron niveles de LDL colesterol <2,59mmol/L. Los pacientes con complicaciones nuevas presentaron una edad más avanzada, mayor IMC, mayor perímetro de cadera y valores más elevados de presión arterial sistólica, así como un mayor consumo de fármacos hipotensores.
ConclusiónLa creación de una unidad de detección de complicaciones crónicas de la diabetes permite detectar micro o macroangiopatía en una sola visita anual, aumentando el cumplimiento de visitas, y en consecuencia establecer las medidas preventivas para su progresión.
The quality of life of patients with diabetes depends on the course of chronic microvascular and macrovascular complications.1 Microvascular complications (retinopathy, nephropathy, and neuropathy) cause disability and loss of quality of life, while macrovascular complications cause death in 80% of patients with type 2 diabetes mellitus (T2DM).
Since the United Kingdom Prospective Diabetes Study (UKPDS) was published, it is accepted that 50% of patients with T2DM have microvascular and macrovascular complications at diagnosis.2 However, there have been significant changes in the diagnosis and monitoring of these patients in recent years. Thus, cross-sectional population studies in Catalonia showed that microvascular complication rates could be lower: retinopathy 12%, microalbuminuria 16%.3
According to the current recommendations of the American Diabetes Association (ADA), all patients with T2DM should be assessed for macroangiopathy and microangiopathy at diagnosis, as should all patients with type 1 diabetes mellitus (T1DM) diagnosed more than five years before. Patients with diabetes are usually required to attend different hospital clinics, laboratories, primary care centers, and so on to undergo the tests required. This increases the risk of visit non-compliance and, as a result, also increases the chance of underdiagnosing the chronic complications related to diabetes and other cardiovascular risk factors. Different studies have shown that the early detection of microangiopathy and macroangiopathy allows for decreasing their progression, and thus for improving the quality of life in patients with diabetes and decreasing cardiovascular mortality.
Based on the foregoing, we decided to conduct a study to assess the efficiency in detecting chronic complications of diabetes in a unit where the full screening for these conditions could be performed at a single visit.
Patients and methodsPatientsA cohort study was conducted to assess the prevalence and incidence of chronic complications of diabetes and cardiovascular risk factors in patients diagnosed with diabetes in our reference area (132,000 inhabitants).
Patients aged 18–80 years diagnosed T1DM or T2DM more than six months before from the reference primary care centers or the outpatient clinics of our hospital were enrolled into the study. Patients less than 18 years of age were excluded. The study protocol was approved by the Ethics Committee of the hospital.
Patients who met the inclusion criteria were referred to the endocrinology day hospital from February 2010 to September 2011, and were assessed by an endocrinologist and a nurse.
Data collected included age, sex, year of diagnosis of diabetes, type of diabetes, anthropometric data (weight, height, body mass index [BMI]), and abdominal circumference (measured at the broadest part of both buttocks, between the last rib and iliac crest).
MeasurementsBlood pressure was measured using a standardized method. Measurement was always done by the same examiner after the participant had rested for 10min sitting in a quiet room. Blood pressure was measured in the left arm, with the elbow flexed at heart level, using a sphygmomanometer OMRON M6 (HEM-7001-E). Three consecutive readings were taken, and the mean of the last two readings was used for analysis.
The last lipid profile obtained after fasting for 12h, including triglyceride, total cholesterol, HDL cholesterol, and LDL cholesterol levels, was recorded. Triglyceride and HDL cholesterol levels were measured using molecular absorption spectrophotometry (enzymatic method). Total cholesterol levels were measured using molecular absorption spectrophotometry (esterase/cholesterol oxidase/peroxidase method). LDL levels were calculated using Friedewald formula if the triglyceride level was less than 4.6mmol/L.
Patients were also asked about their smoking habits.
Data regarding the use of antiaggregant, lipid lowering, antihypertensive, and hypoglycemic drugs and insulin (daily number of injections and total daily dose) were collected.
A DCA 2000 device was used for measuring glycosylated hemoglobin (HbA1c).
ExaminationsDiabetic retinopathy was diagnosed on the same day of examination by eye fundus examination by an ophthalmologist from the unit who was an expert on this condition.
Diabetic nephropathy was assessed using the albumin/creatinine ratio in a first measurement, which was confirmed by a second determination three months later. The absence of nephropathy was defined as normal urinary albumin (albumin/creatinine ratio<30mg/g), and incipient nephropathy was defined as the presence of microalbuminuria (albumin/creatinine ratio 30–299mg/g). Frank nephropathy was defined as the presence of macroalbuminuria (albumin/creatinine ratio>300mg/g).
To assess neuropathy, patients were asked about symptoms suggesting neuropathy (loss of sensitivity in lower limbs, paresthesia, dysesthesia). Perception of vibration was measured using a 128Hz tuning fork and the feeling of pressure of a 10g monofilament in the distal plantar aspect of both big toes and the metatarsal joints. Neuropathy was diagnosed if changes were found in two or more of the three items evaluated.
To screen for peripheral vasculopathy, patients were asked about the presence of intermittent claudication, and the ankle-arm index was measured using bi-directional Doppler of the lower limbs. Peripheral vasculopathy was defined as the presence of intermittent claudication and/or an ankle-arm index≤0.9 or ≥1.3.
All patients were asked about a history of ulcers or amputation.
Data on any history of major cardiovascular events (acute myocardial infarction, history of myocardial revascularization, angioplasty, stroke, transient ischemic attack) were collected. All patients with no history of cardiovascular disease were asked about potential symptoms suggesting cardiac ischemia and were given a baseline electrocardiogram. Patients with ECG symptoms and changes suggesting ischemic heart disease were evaluated by a cardiologist.
Prevalence was defined as any previously documented microvascular or macrovascular complication at the time of evaluation by the endocrinologist. Incidence was defined as de novo diagnosis of any microvascular or macrovascular complication.
High blood pressure was defined as systolic blood pressure (SBP)≥130mmHg and/or diastolic blood pressure (DBP)≥80mmHg or the use of antihypertensive drugs.
Hypercholesterolemia was defined as the use of lipid lowering drugs or the following serum levels: total cholesterol≥5.17mmol/L, triglycerides≥3.88mmol/L, HDL cholesterol≤1.29mmol/L in females or ≤1.16mmol/L in males, or LDL cholesterol≥2.59mmol/L.
Statistical analysisA Student's t test was used to compare means, and a Chi-square test was used to analyze categorical variables, while a Mann–Whitney U test was used for variables not normally distributed. Results were analyzed using SPSS statistical software, version 15.0 for Windows.
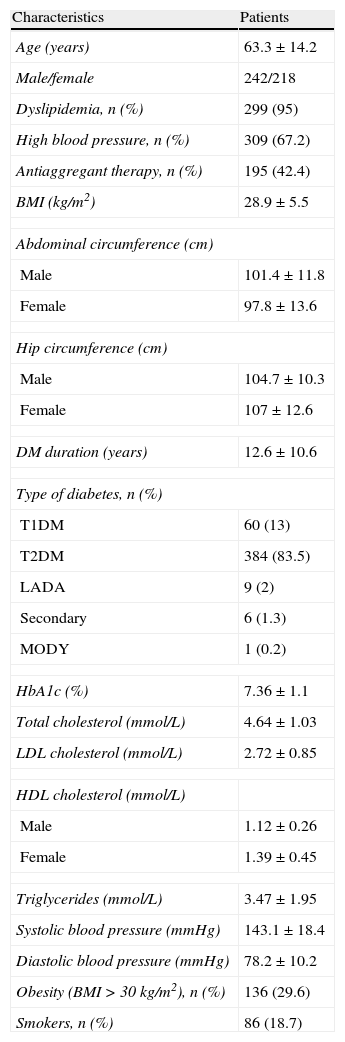
ResultsFour hundred and sixty patients seen at the endocrinology day hospital from February 2010 to September 2011 were enrolled into the study. Table 1 shows their demographic, anthropometric, and clinical characteristics.
Demographic, anthropometric, and clinical characteristics.
| Characteristics | Patients |
| Age (years) | 63.3±14.2 |
| Male/female | 242/218 |
| Dyslipidemia, n (%) | 299 (95) |
| High blood pressure, n (%) | 309 (67.2) |
| Antiaggregant therapy, n (%) | 195 (42.4) |
| BMI (kg/m2) | 28.9±5.5 |
| Abdominal circumference (cm) | |
| Male | 101.4±11.8 |
| Female | 97.8±13.6 |
| Hip circumference (cm) | |
| Male | 104.7±10.3 |
| Female | 107±12.6 |
| DM duration (years) | 12.6±10.6 |
| Type of diabetes, n (%) | |
| T1DM | 60 (13) |
| T2DM | 384 (83.5) |
| LADA | 9 (2) |
| Secondary | 6 (1.3) |
| MODY | 1 (0.2) |
| HbA1c (%) | 7.36±1.1 |
| Total cholesterol (mmol/L) | 4.64±1.03 |
| LDL cholesterol (mmol/L) | 2.72±0.85 |
| HDL cholesterol (mmol/L) | |
| Male | 1.12±0.26 |
| Female | 1.39±0.45 |
| Triglycerides (mmol/L) | 3.47±1.95 |
| Systolic blood pressure (mmHg) | 143.1±18.4 |
| Diastolic blood pressure (mmHg) | 78.2±10.2 |
| Obesity (BMI>30kg/m2), n (%) | 136 (29.6) |
| Smokers, n (%) | 86 (18.7) |
Units are mean±standard deviation except as otherwise stated.
As regards the control of metabolic parameters and cardiovascular risk factors, 42% of patients had glycosylated hemoglobin (HbA1c) values≤7%, 20% had blood pressure levels less than 130/80mmHg, and 46% had LDL cholesterol levels<2.59mmol/L. Forty-five percent of patients had an optimum control of more than two cardiovascular risk factors.
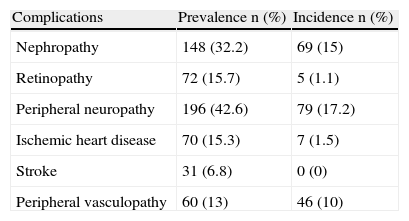
The prevalence of chronic complications, defined as the presence of one or more complications at the time of the visit, was 57%. The most common complications were peripheral neuropathy and nephropathy.
As regards the incidence of chronic complications, 163 patients (35.4%) had some unknown complication, of which peripheral neuropathy was the most common, followed by nephropathy. At least one previously undiagnosed complication was found in 27.6% of patients, while 6.3% and 1.5% of patients had two and three undiagnosed complications respectively.
Table 2 shows the relationship between previously known and de novo diagnosed chronic complications.
Prevalence and incidence of diabetes complications.
| Complications | Prevalence n (%) | Incidence n (%) |
| Nephropathy | 148 (32.2) | 69 (15) |
| Retinopathy | 72 (15.7) | 5 (1.1) |
| Peripheral neuropathy | 196 (42.6) | 79 (17.2) |
| Ischemic heart disease | 70 (15.3) | 7 (1.5) |
| Stroke | 31 (6.8) | 0 (0) |
| Peripheral vasculopathy | 60 (13) | 46 (10) |
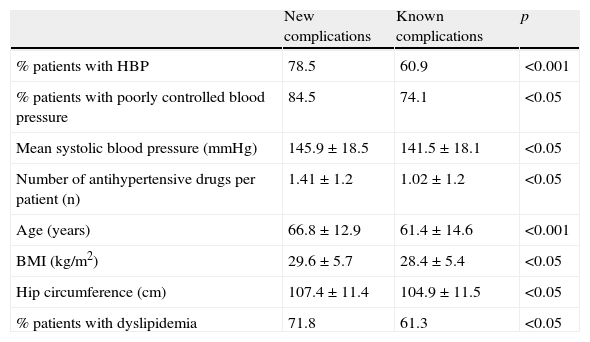
A comparison of patients with new and previously known complications (Table 3) showed that patients diagnosed with a new complication were older (61.4±14.6 years versus 66.8±12.9 years, p<0.001) and had higher BMI (28.4±5.4kg/m2 versus 29.6±5.7kg/m2, p<0.05), hip circumference (104.9±11.5cm versus 107.4±11.4cm, p<0.05), and systolic blood pressure (141.5±18.1mmHg versus 145.9±18.5mmHg, p<0.05) values. They also made greater use of antihypertensive drugs (1.02±1.2 drugs versus 1.41±1.2 drugs, p<0.05).
Differences between patients with new and previously diagnosed complications.
| New complications | Known complications | p | |
| % patients with HBP | 78.5 | 60.9 | <0.001 |
| % patients with poorly controlled blood pressure | 84.5 | 74.1 | <0.05 |
| Mean systolic blood pressure (mmHg) | 145.9±18.5 | 141.5±18.1 | <0.05 |
| Number of antihypertensive drugs per patient (n) | 1.41±1.2 | 1.02±1.2 | <0.05 |
| Age (years) | 66.8±12.9 | 61.4±14.6 | <0.001 |
| BMI (kg/m2) | 29.6±5.7 | 28.4±5.4 | <0.05 |
| Hip circumference (cm) | 107.4±11.4 | 104.9±11.5 | <0.05 |
| % patients with dyslipidemia | 71.8 | 61.3 | <0.05 |
BP values>130/80mmHg were found in 84.5% of patients with a new complication, as compared to 74.1% of patients with already known complications (p<0.05). Moreover, high blood pressure was found in 78.5% of patients with de novo diagnosed complications, as compared to 60.9% of patients with previously documented complications (p<0.001).
Of the patients who had a new complication, 71.8% were diagnosed with dyslipidemia, as compared to 61.3% of patients in the group with known complications (p<0.05).
In logistic regression analysis, age was shown to be the variable most influential regarding the risk of an occurrence of new complications of diabetes (odds ratio, 1.03; 95% CI, 1.01–1.05; p<0.001).
DiscussionIn our series of diabetic patients, 57% of patients had one or more complications related to diabetes. These data agree with those reported by the UKPDS study, where 50% of patients with T2DM had microvascular or macrovascular complications at diagnosis. It should however be noted that mean diabetes duration in our series was 12.6 years.
Studies conducted in Spain on the prevalence of chronic complications of diabetes have reported the following prevalence rates: diabetic retinopathy, 15–50%; microalbuminuria, 23%; macroalbuminuria, 5%; peripheral neuropathy, 24%; ischemic heart disease, 10–25%; and stroke, 5–15%.4
The prevalence of neuropathy and nephropathy in our series was greater than that reported in prior studies, while prevalence rates of retinopathy, ischemic heart disease, and vasculopathy were similar.
It should be noted that in 35.4% of the patients in our series a previously undiagnosed complication was found. Nephropathy and peripheral polyneuropathy were most common (15% and 17.2% respectively). These figures suggest that these complications are probably underdiagnosed in routine monitoring of diabetic patients, because they are much higher than the annual incidence seen in prospective studies with large patient samples. Emphasis should, therefore, be placed on the importance of screening for complications, at both the primary care and specialized levels, to prevent delayed diagnosis and the resultant poorer prognosis of complications.
According to the results of our series, patients with advanced age, obesity, and high blood pressure have a greater risk of experiencing a new complication, with age being the variable most influential in terms of the risk of developing a complication related to diabetes.
As regards the control of cardiovascular risk factors, only 20% of patients had blood pressure levels<130/80mmHg, and 46% had LDL levels<2.59mmol/L. These results again show the great difference between the control goals recommended in clinical practice guidelines and those seen in standard practice. In this situation, it is particularly relevant not to play down the importance of blood pressure and lipid levels and to avoid delay in treatment start or intensification and therapeutic inertia. A study conducted on a cohort of 343 diabetic patients followed up for four years showed improved blood pressure and lipid profile control with treatment intensification.5 The study ‘Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes’ (Steno-2) similarly demonstrated that a multifactorial approach to overall cardiovascular risk factors is able to decrease the incidence of microvascular and macrovascular complications by more than 50%,6 as well as cardiovascular mortality.6,7
It has also been separately shown that SBP reduction to less than 140mmHg and DBP reduction to less than 80mmHg in diabetic patients decreases the number of episodes of cardiovascular disease and stroke, as well as the incidence of neuropathy.8,9
On the other hand, several clinical trials have shown the benefits of lipid lowering drug treatment on the course of cardiovascular disease in patients with coronary disease, and for primary prevention of cardiovascular disease. Analyses of diabetic subgroups from larger studies10–14 and from those specifically conducted on diabetic patients15,16 have shown the significant value of lipid lowering drug treatment in primary and secondary prevention of cardiovascular disease events. Thus, in the CARDS study16 and the Heart Protection Study,11 statin treatment achieved 37% and 33% reductions in the risk of occurrence of a major cardiovascular event in diabetic patients as compared to placebo.
The limitations of this study are derived from its cross-sectional design. We should therefore not forget the potential temporal variability the tested parameters may experience, on the one hand, and the fact that the reported findings only represent associations and do not imply a causal relationship. Since no previous data are available, it is not possible to use the actual incidence of complications to assess how many were underdiagnosed.
In conclusion, the creation of a unit to detect chronic complications of diabetes allows for the detection of microangiopathy and macroangiopathy at a single annual visit, thus increasing visit compliance and so facilitating the taking of appropriate action to prevent their progression.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please, cite this article as: Fernández-Miró M, et al. Infradiagnóstico de complicaciones crónicas de la diabetes mellitus: utilidad de una revisión sistemática en una sola visita. Endocrinol Nutr. 2012;59:585–90.