Treatment of Cushing's disease poses interesting dilemmas in clinical practice. The aim of our study was to analyze the outcomes of the different treatments, the control and recurrence rates, and the complications derived from them.
Material and methodsData were collected from the clinical records of 22 patients over 18 years of age (86.4% women). They had been diagnosed with Cushing's disease between 2000 and 2012, and were monitored at Complejo Hospitalario Universitario-Albacete, Hospital Virgen de la Salud-Toledo Hospital General Universitario de Ciudad Real, Hospital Virgen de la Luz-Cuenca, Hospital Nuestra Señora del Prado-Talavera de la Reina, and Complejo Hospitalario la Mancha Centro-Alcázar de San Juan.
ResultsSurgery was the treatment of choice in all patients. Biochemical cure was achieved in 72.2% of patients. Nine patients developed in the early postoperative period diabetes insipidus, which became in two patients only. Surprisingly, three patients with normal postoperative neurohypophyseal function later developed permanent diabetes insipidus. New hormone deficiencies occurred in seven patients. Seventeen patients received ketoconazole before surgery (five of them after surgery also), and 70% of them achieved normal urinary free cortisol levels. Three patients also received radiotherapy, and all of them were cured after a median follow-up of 85.5 months; they developed no tumors or other complications.
ConclusionsOur study reports the outcomes of management of Cushing's disease in non-reference centers for this disease, possibly giving a realistic picture of standard clinical practice for the condition in Spain.
El tratamiento de la enfermedad de Cushing plantea interesantes dilemas en la práctica clínica. Nuestro objetivo es analizar los resultados y complicaciones de los distintos tratamientos de esta enfermedad.
Material y métodosSe recopilaron datos mediante revisión de las historias clínicas de 22 pacientes (86,4% mujeres), mayores de 18 años, diagnosticados de enfermedad de Cushing entre los años 2000 y 2012, con seguimiento en el Complejo Hospitalario Universitario de Albacete, Hospital Virgen de la Salud (Toledo), Hospital General de Ciudad Real, Hospital Virgen de la Luz (Cuenca), Hospital Nuestra Señora del Prado (Talavera de la Reina) y en el Complejo Hospitalario la Mancha Centro (Alcázar de San Juan).
ResultadosEn todos los casos el tratamiento de elección fue el quirúrgico. Se consiguió la curación bioquímica en el 72,7%. Nueve pacientes desarrollaron diabetes insípida en el perioperatorio, de las que 2 resultaron permanentes. Tres pacientes desarrollaron diabetes insípida permanente, que no había sido identificada en el perioperatorio. Aparecieron nuevos déficits hormonales adenohipofisarios posquirúrgicos en 7 pacientes. Diecisiete pacientes recibieron tratamiento médico prequirúrgico con ketoconazol (5 también postoperatorio), consiguiéndose la normalización del cortisol libre urinario en el 70%. Tres pacientes se irradiaron por persistencia de hipersecreción y, tras una mediana de seguimiento de 85,8 meses, se ha conseguido la curación en todos; ninguno de ellos ha desarrollado tumores, alteraciones vasculares ni otra complicación.
ConclusionesNuestro estudio presenta los resultados del manejo de la enfermedad de Cushing en centros que no son de referencia nacional para esta enfermedad, lo que posiblemente refleja la práctica clínica habitual en esta enfermedad.
Cushing's disease continues to be one of the most interesting challenges in our clinical practice. The complexity of its diagnosis, combined with its insidious course, makes Cushing's disease one of the most fascinating endocrine conditions.
Once a diagnosis of Cushing's disease has been made, transsphenoidal surgery is the first-line treatment, while radiotherapy (RT), medical treatment, or adrenalectomy are reserved for recurrent or persistent disease.1–3 Ideally, treatment should achieve control of cortisol hypersecretion, remove the tumor sparing the remaining pituitary function, recover the pituitary-adrenal axis (if possible), and reverse the effects of chronic hypercortisolism.1 However, the actual situation in clinical practice greatly differs from this ideal treatment, because iatrogenic hormone deficiencies are not uncommon. Moreover, the hypercortisolism experienced by patients increases their surgical risk, and complications may occur.
This article reports the results of a descriptive study of the management of patients with Cushing's disease conducted in six hospitals in Castilla-La Mancha. It was part of a wider study of patients with pituitary tumors of all types using a single database: “Study of the results of the treatment of pituitary tumors in Castilla-La Mancha”. The primary objective was to analyze the results achieved with the different treatments in terms of cure, disease control, and subsequent recurrence, and to report on the complications found. The secondary objective was to ascertain the extent to which the different therapeutic options available were used. Although this was not a study objective, potential predictors of cure related to tumor characteristics and the perioperative period were also sought.
Patients and methodsA retrospective review was conducted of the clinical histories of patients diagnosed with Cushing's disease who met the inclusion criteria and who agreed to participate in the study by signing an informed consent. Data were collected about the different treatments received by these patients:
- -
Surgery: surgical procedures, hospitals where surgery was performed, pathological results, cures, complications in the early and late postoperative periods, and recurrence rates and management.
- -
Adjuvant treatments: indications, results, and complications of medical treatment and RT.
All patients over 18 years of age diagnosed with Cushing's disease between 2000 and 2012 followed up at the participating hospitals (Complejo Hospitalario Universitario de Albacete, Hospital Virgen de la Salud de Toledo, Hospital General Universitario de Ciudad Real, Hospital Virgen de la Luz de Cuenca, Hospital Nuestra Señora del Prado de Talavera de la Reina, and Complejo Hospitalario La Mancha Centro de Alcázar de San Juan) were enrolled into the study. Diagnosis of Cushing's disease was based on the clinical practice guidelines most widely accepted at the time.
The fact that surgery or RT was performed at a different hospital from that of the study participants was not an exclusion criterion.
Remission and recurrence after surgeryCure was defined as the occurrence of adrenal insufficiency or the normalization of urinary free cortisol (UFC) levels to <1.8mcg/dL after 1mg of dexamethasone. Recurrence was only considered to have taken place if the cure criteria had previously been met.
Statistical analysisA common database was created, and a descriptive analysis was made. Results are given as the mean and standard deviations for normally distributed variables, and as the median with interquartile range (IR) for non-normally distributed variables.
For hypothesis testing with regard to which variables could predict postoperative cure or recurrence, contingency tables were created and a Pearson's Chi-square test was used.
A value of p≤0.05 was considered statistically significant. SPSS statistical software was used for the analysis.
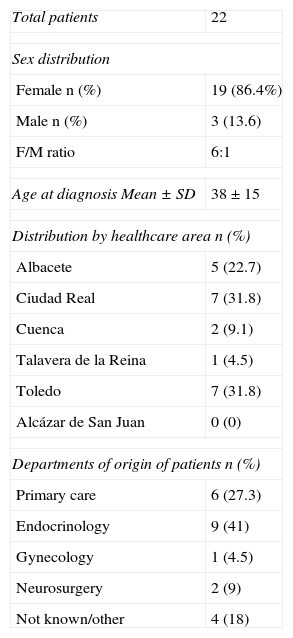
ResultsA total of 22 patients were enrolled, 86.4% females and 13.6% males (Table 1). Mean age at diagnosis was 38 years, with a standard deviation of 15. Median follow-up was 81 months (IR: 42–129 months).
Demographic data.
| Total patients | 22 |
| Sex distribution | |
| Female n (%) | 19 (86.4%) |
| Male n (%) | 3 (13.6) |
| F/M ratio | 6:1 |
| Age at diagnosis Mean±SD | 38±15 |
| Distribution by healthcare area n (%) | |
| Albacete | 5 (22.7) |
| Ciudad Real | 7 (31.8) |
| Cuenca | 2 (9.1) |
| Talavera de la Reina | 1 (4.5) |
| Toledo | 7 (31.8) |
| Alcázar de San Juan | 0 (0) |
| Departments of origin of patients n (%) | |
| Primary care | 6 (27.3) |
| Endocrinology | 9 (41) |
| Gynecology | 1 (4.5) |
| Neurosurgery | 2 (9) |
| Not known/other | 4 (18) |
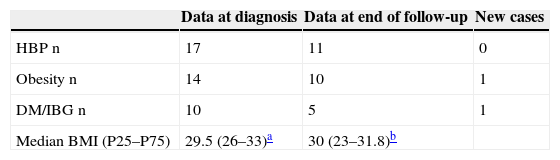
In our series, prevalence rates of HBP and obesity at diagnosis were 77% and 63% respectively (Table 2).
In preoperative tests, median UFC levels, as compared to the upper normal limit of each laboratory, were 3.73 (IR: 1.69–5). The imaging test used for diagnosis in all patients was MRI, which did not reveal tumor in six of them. Inferior petrosal sinus sampling (IPSS) was performed in two of these patients. Pathological MRI disclosed two tumors 11mm in largest diameter, while all other tumors were less than 10mm in size. Cavernous sinus invasion was not seen in any case. Six campimetries were performed, five with normal results and one revealing temporal hemianopsia, although no patient reported visual disturbances.
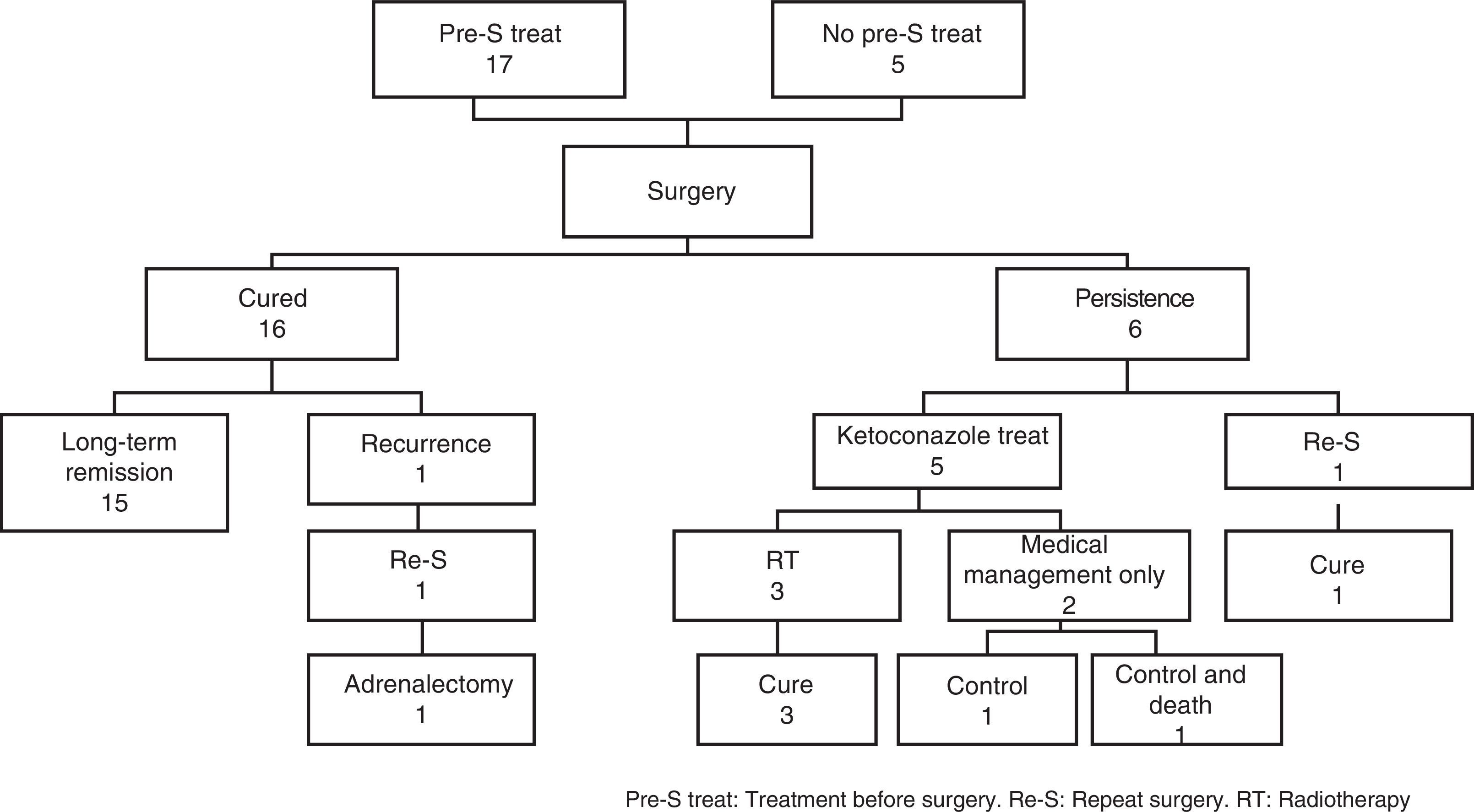
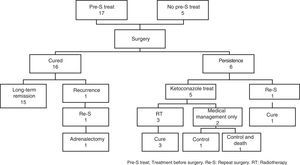
The results of treatments used in all patients are summarized in Fig. 1.
The treatment of choice in all patients was surgery through a transsphenoidal approach. Endoscopic and non-endoscopic procedures were used in five and 17 patients respectively. Tumor resection was complete according to surgical protocol in 17 patients, partial in one patient, hemihypophysectomy in two patients, and not reported in two patients.
Biochemical cure was achieved in 16 of the 22 patients (72.7%), while the disease persisted in six patients (27%). Among the cured patients, 10 (62%) developed postoperative adrenal insufficiency; all other patients were considered to be cured with no evidence of ACTH deficiency.
Eighty percent of patients with a visible image in MRI achieved cure, as compared to 50% of those with an imaging test with no findings. The difference did not reach statistical significance (p=0.16), probably because of the small sample size. IPSS was performed in two of the six patients with no evidence of adenoma in MRI before surgery. One patient underwent IPSS outside the Castilla-La Mancha region, and the result was not available, but was cured after surgery. The second patient achieved no cure despite the presence of a central-peripheral gradient, and was finally treated with RT. Among patients for whom the surgical protocol was available, a cure was achieved in 70% of those for whom complete tumor resection was reported and in 66% of those in whom the surgeon could not ensure total resection.
Eleven (68.8%) of the 16 patients with evidence of adenoma in the surgical specimen achieved a biochemical cure, as did three of the four patients (75%) whose sample was reported as normal pituitary tissue. No data concerning the histological result were available for two patients, who were both cured. Pathological examinations identified adenoma in four of the patients with no lesion evidence in MRI. Two of these patients were cured.
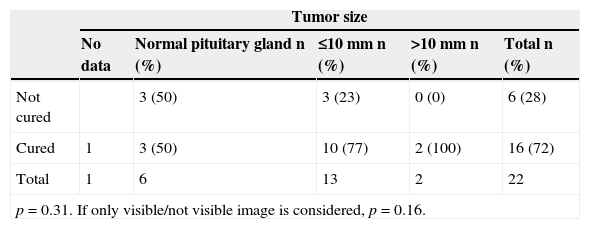
Thus, no statistically significant differences were found in the outcome of surgery when findings were compared based on preoperative MRI, the different surgical approaches, or on the evidence of adenoma in the samples sent to the pathological laboratory. A comparison of the results of the different surgical departments showed no significant differences either (Table 3).
Cured/not cured ratio as a function of different variables.
| Tumor size | |||||
|---|---|---|---|---|---|
| No data | Normal pituitary gland n (%) | ≤10mm n (%) | >10mm n (%) | Total n (%) | |
| Not cured | 3 (50) | 3 (23) | 0 (0) | 6 (28) | |
| Cured | 1 | 3 (50) | 10 (77) | 2 (100) | 16 (72) |
| Total | 1 | 6 | 13 | 2 | 22 |
| p=0.31. If only visible/not visible image is considered, p=0.16. | |||||
| Type of surgery | |||||
|---|---|---|---|---|---|
| No data | Hemihypophysectomy n (%) | Partial n (%) | Complete n (%) | Total n (%) | |
| Not cured | 1 (50) | 0 (0) | 5 (29.4) | 6 (28) | |
| Cured | 2 | 1 (50) | 1 (100) | 12 (70.6) | 16 (72) |
| Total | 2 | 2 | 1 | 17 | 22 |
| p=0.66. | |||||
| Place of surgery n (%) | |||||
|---|---|---|---|---|---|
| Madrid | Toledo | C. Real | Albacete | Total | |
| Not cured | 2 (20) | 4 (50) | 0 (0) | 0 (0) | 6 (27) |
| Cured | 8 (80) | 4 (50) | 3 (100) | 1 (100) | 16 (72) |
| Total | 10 | 8 | 3 | 1 | 22 |
| p=0.278. | |||||
| Pathology | ||||
|---|---|---|---|---|
| No data | Adenoma n (%) | Normal pituitary gland n (%) | Total v | |
| Not cured | 5 (31.3) | 1 (25) | 6 (28) | |
| Cured | 2 | 11 (68.8) | 3 (75) | 16 (72) |
| Total | 2 | 16 | 4 | 22 |
| p=1.00 (Fisher's exact test). | ||||
Nine patients developed perioperative diabetes insipidus (DI), which only became permanent in two of them. Interestingly, three patients in whom DI was not identified in the perioperative period developed permanent DI. Apart from ACTH insufficiency, new hormone deficiencies occurred after surgery in seven patients. Of these, four had panhypopituitarism and three isolated gonadotropin deficiency. Postoperative pituitary function study included the somatotropic axis in most patients. Of the six patients in whom somatotropic axis function was not tested, only one had some impaired axis (gonadotropins). The most severe complications were meningitis and pneumonia, which occurred in the same patient, the only one who had a CSF fistula. There were no thrombotic complications, bleeding, or other infections.
Adjuvant treatments (Fig. 1)Medical treatment: 17 patients received ketoconazole before surgery, and 70% of them achieved normalization of UFC levels. Treatment was discontinued in three patients due to transaminase elevation. As regards postoperative medical management, five patients were treated with ketoconazole for persistent disease.
Radiotherapy: three patients were irradiated for persistent hypersecretion. One patient was treated with Gamma Knife at a dose of 16.80Gy; the other two patients were treated with fractionated stereotactic RT: one of them received a dose of 50.40Gy, while no data are available for the other patient. Cure was achieved in all of them after follow-up times of 82, 85.8, and 115 months from RT. A single patient developed new hormone deficiencies after irradiation, and no tumors, vascular changes, or other complications occurred after RT.
Final statusControl of hypercortisolism was finally achieved in all patients. One patient with long-standing psychiatric disease before the diagnosis of Cushing's syndrome died from autolysis without developing adrenal insufficiency, but maintained at all times normal UFC levels with medical treatment.
The only patient with a recurrence of Cushing's disease underwent repeat transsphenoidal surgery. However, because of persistent hypercortisolism and transaminase elevation due to the use of ketoconazole before surgery, he finally underwent bilateral adrenalectomy without RT. The patient has no evidence of growth of the pituitary tumor after three years of follow-up.
In the last assessment of pituitary function available, six patients showed panhypopituitarism (27%) and another three patients had partial deficiency, excluding ACTH deficiency (13%: one patient with gonadotropin deficiency and two patients with TSH deficiency). Eleven of the remaining patients had a completely normal pituitary function, while ACTH deficiency alone persisted in two patients. The adrenal insufficiency developed after surgery persisted in seven of 10 patients at the end of follow-up. In other words, seven of the eight patients with ACTH deficiency at the end of follow-up had such deficiency from surgery, while one developed it after RT. At the end of follow-up, permanent DI was associated with panhypopituitarism in two patients, while it was not associated with any other deficiency (including GH study) in the remaining three patients.
In patients for whom data from the last radiographic assessment were available, a normal pituitary gland was found in more than 70%, an empty sella turcica was reported in four cases (20%), and one patient had a visible tumor residue that remains stable.
DiscussionOur study analyzed the results of the different treatments in patients with Cushing's disease in Castilla-La Mancha in terms of cure, disease control, and subsequent recurrence, as well as the complications derived from the different treatments.
The first-line treatment was transsphenoidal surgery in all patients. Although comparison of the cure rates found in different studies is difficult because of heterogeneity in the cure criteria and the inclusion of macroadenomas, the cure rate in our study was 72.7%, comparable, although in the lower limit, to the rate reported in other series from more experienced hospitals (70–90%4–8). Although postoperative adrenal insufficiency was retrospectively recorded in only 10 patients, this is probably an underestimation due to data loss, as the data came from several hospitals and, in some cases, from different regions.
The absence of aggressive macroadenomas had a favorable influence on our cure rate. Tumor size has been considered a predictor in some studies, with poorer results being found in tumors greater than 10mm. Size was not decisive in our series, possibly because the largest tumors were 11mm at maximum diameter and did not invade the cavernous sinuses, so that their behavior resembled that of microadenomas. After differentiating patients with negative MRI (50% cure rate) from those with visible tumor in MRI (80% cure rate), no statistically significant differences were found (p=0.169). This result may be explained by our small sample size. Studies on this predictor have reported conflicting results. While some of them found that visualization in preoperative MRI may be a positive predictor of a biochemical cure,9 most found no difference.6 Some series reported the presence of adenoma in the surgical specimen as a predictor6,10,11; however, our results regarding this variable are not conclusive.
Since surgical procedures were performed in various hospitals, with a low number of patients recruited in each of them, we could not analyze the influence of surgeon experience on the results.
As regards postoperative adverse events, 12 patients (54%) experienced complications. Of these, only one had CSF fistula and severe complications. As expected, the most common complication was DI. In a study conducted by Hensen et al.12 where changes in osmoregulation (polyuria and hyponatremia) were analyzed in patients who underwent transsphenoidal surgery for pituitary tumors, patients with Cushing's disease were found to have a greater incidence of both changes as compared to those with all other pituitary tumors. Nemergut et al.13 found a greater risk of transient (22%), but not permanent DI. In our study, transient DI was found in nine patients (40%). This is a frequency similar to that reported in other recent series (6–35%6,14,15). Permanent DI occurred in up to 22% of our study patients, which appears to be a strikingly high incidence as compared to other series (5%14,15).
With regard to medical treatment, 17 patients were treated with ketoconazole, 11 before surgery only and five both before and after surgery. UFC levels normalized in 70% of patients treated with ketoconazole as part of their preoperative management. Disease control was achieved in three patients treated after surgery (60%), which agrees with data reported by Castinetti et al.,16 who conducted a large retrospective study in patients with Cushing's disease treated with ketoconazole, finding normalization of UFC levels in 64% of patients operated on but not cured. The main side effect in our series was transaminase elevation, which required the discontinuation of medical treatment in three patients (17%). This side effect was reported by Castinetti et al. in 13% of patients.17
Only three patients received RT. After a median follow-up of 85.8 months, new pituitary deficiencies occurred in a single patient. New deficiencies are expected to occur in 50% of patients after RT, with no clear evidence that the Gamma Knife technique minimizes this adverse effect.1 RT is an effective treatment in patients with persistent or recurrent Cushing's disease, inducing five-year remission rates up to 90% in some studies. Many authors therefore consider RT the treatment of choice after surgery failure,18 but this view is not shared by all authors. Although the results in our series were very good, it is difficult to draw conclusions because of the low number of patients irradiated.
During the overall median follow-up of seven years in our study, disease recurrence was found in a single patient six years after surgical cure. Recurrence may occur up to 15 years after cure,11 but most of them occur in the first five years. The different criteria for defining the cure of Cushing's disease not only make cure rates of the different studies difficult to compare, but also affect recurrence rates.
As mentioned, this study was part of a wider study in patients with pituitary tumors in Castilla-La Mancha. As a single database was used, some biochemical data of interest in Cushing's disease were not included as variables in the common database. Our study had additional limitations. On the one hand, our patient sample was small. In addition, patients underwent surgery at different hospitals, a variability factor that would have been avoided if a single surgeon had performed all the procedures. Because of the retrospective and multicenter nature of this study, and the fact that surgery and follow-up of several patients were performed at different hospitals, incomplete information was available on some variables of interest, such as the ketoconazole doses needed for disease control, or the doses at which complications occurred. On the other hand, the main study interest is that it represents the current and actual status of treatment for Cushing's disease in a number of tertiary hospitals, not considered as reference hospitals for this disease. Therefore, the results may probably be extrapolated to most Spanish hospitals.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Huguet I, Aguirre M, Vicente A, Alramadan M, Quiroga I, Silva J, et al. Análisis de los resultados del tratamiento de la enfermedad de Cushing en los hospitales de Castilla-La Mancha. Endocrinol Nutr. 2015;62:217–223.