Since the onset of cross hormone therapy (CHT) in transsexual individuals, there has been concern about possible chronic side effects. Our objective was to assess baseline differences in lipid profile in individuals with gender identity disorder in relation to prior CHT, and changes in the lipid profile and other cardiovascular (CV) risk factors after 24 months of treatment.
MethodsRetrospective longitudinal study including all individuals assisted for the first time in the Gender Identity Unit of Catalonia from 2006 to 2010. Socio-demographical, anthropometric and laboratory data were collected.
ResultsWe evaluated 247 transsexuals, 150 male to female (MtF: 60.7%) and 97 female to male (FtM; 39.3%). At baseline, FtM transsexuals were younger and had started prior CHT less often than MtF (13.4% vs. 64.7%; p<0.001). During follow up, in MtF weight and BMI increased significantly, as well as systolic and diastolic blood pressure, though these latter remained within normal range. No significant differences in lipid profile were observed. FtM transsexuals also presented an increase in weight and BMI, without differences in blood pressure. A general worsening in lipid profile was observed in this group, with increased total cholesterol (166.0±35.1 vs. 175.6±38.2mg/dL; p=0.001), triglycerides (70.6±30.7 vs. 102.3±68.5mg/dL; p<0.001) and LDL cholesterol (103.8±28.7 vs. 112.8±30.3mg/dL; p=.013) and decreased HDL cholesterol (52.2±12.2 vs. 45.4±13.8mg/dL; p=0.001), even though final levels were all within normal range.
ConclusionThere is no detectable increase in CV risk factors in MtF transsexuals who were treated with currently prescribed estrogenic compounds, while a slight worsening in lipid profile takes place in the FtM group, though within normal limits.
Desde la introducción del tratamiento hormonal cruzado (CHT) en los individuos transexuales existe preocupación sobre sus posibles efectos secundarios a largo plazo. Nuestro objetivo fue evaluar las diferencias en el perfil lipídico basal de individuos transexuales en relación con haber realizado o no CHT previo, y los cambios en dicho perfil y en otros factores de riesgo cardiovascular (FRCV) tras 24 meses de tratamiento.
MétodosEstudio longitudinal retrospectivo incluyendo todos los pacientes atendidos como primera visita en nuestra unidad entre 2006 y 2010. Se recogieron datos socio-demográficos, antropométricos y de laboratorio.
ResultadosSe evaluaron 247 transexuales, 150 de hombre a mujer (MtF: 60.7%) y 97 de mujer a hombre (FtM: 39.3%). Basalmente, los transexuales FtM eran más jóvenes y habían realizado CHT previamente con mayor frecuencia (13.4% vs. 64.7%; p<0.001). Durante el seguimiento el peso y el IMC aumentaron en MtF de forma significativa, así como la tensión arterial sistólica y diastólica, aunque estos dos últimos se mantuvieron dentro de la normalidad. No se objetivaron diferencias significativas en el perfil lipídico. Los transexuales FtM también presentaron un incremento de peso e IMC, sin diferencias en la tensión arterial. Se observó un empeoramiento generalizado del perfil lipídico en este grupo, con aumento del colesterol total (166.0±35.1 vs. 175.6±38.2mg/dL; p=0.001), triglicéridos (70.6±30.7 vs. 102.3±68.5mg/dL; p<0.001) y colesterol LDL y empeoramiento del colesterol HDL (52.2±12.2 vs. 45.4±13.8mg/dL; p=0.001).
ConclusiónNo se produce un incremento significativo en los FRCV en los transexuales MtF tratados con los compuestos estrogénicos actuales, mientras que se observa un discreto empeoramiento en el perfil lipídico en los transexuales FtM, aunque los valores se mantienen dentro de la normalidad.
Transsexualism makes reference to a discrepancy between a person's gender identity and that person's sex assigned at birth according with his o her primary and secondary sex characteristics. This discrepancy, together with the distress it generates, leads to an irresistible urge to live in the other gender, and modify the own body by hormonal therapy and breast and genital surgery, together with legal and psychosocial adaptations. Sex-reassignment treatment is recommended to be conducted by a multidisciplinary team involving mental health professionals, endocrinologists and surgeons among others. Long term cross-sex hormone treatment (CHT) is necessary to acquire and maintain secondary sexual characteristics.
Available data related to hormonal therapy are extrapolated from other settings, such as male or female subjects with normal gonadal function, different types of sex hormone disorders, or under hormonal therapy, or obtained from historical series of estrogenic therapy in male to female (MtF) transsexuals.
In general terms, a potential protective effect of estrogens on cardiovascular system was assumed due to the lower incidence of cardiovascular (CV) disease observed in premenopausal women compared to men, together with the higher incidence in women with hyperandrogenism. However, it has been shown that postmenopausal exogenous estrogens did not provide this cardioprotective effects1; years later, increased risk of thromboembolic disease,2,3 and even of CV mortality were associated with synthetic estrogens such as ethinylestradiol4. For that reason, recent guidelines recommend avoiding ethinylestradiol and using transdermal estrogen preparations after 40 years of age.5
If we focus on MtF subjects on estrogenic therapy, some studies show an impairment of lipid profile and blood pressure on estrogenic treatment6–9; possibly, these effects are reduced if ethinylestradiol is excluded. However, results are still inconclusive due to the retrospective and limited nature of all the studies.
On the other hand, neither global mortality nor CV events have been found to be increased in female to male (FtM) transsexuals if compared with individuals of the same biological sex.4 However, lipid profile impairment (essentially triglycerides increase) has been shown by some, but not all, studies.7–11 Due to these findings, the clinical practice guideline published in 20095 recommended that transsexuals on CHT should be evaluated for cardiovascular risk factors. Previous longitudinal studies dealing with metabolic and CV effects of CHT are both scarce and referred to populations whose lifestyle differs from ours, as, it is reflected in many studies on CV risk in population from Southern Europe.12
The aim of the present work was to assess baseline differences in lipid profile in individuals with gender identity disorder (MtF and FtM) in relation to prior CHT or not, and changes along follow-up in their lipid profile and other CV risk factors after 24 months of treatment.
MethodsRetrospective longitudinal study of medical records, including all individuals attending for the first time the Gender Identity Unit (Unitat d’Identitat de Gènere (UIG)) of Catalonia (Spain) from 2006 to 2010. We evaluated 247 confirmed transsexuals, 150 MtF (60.7%) and 97 FtM (39.3%). Patients were followed for 24 months; data from the first visit and at 6, 12 and 24 months were collected (68.4% individuals at 24 months, 63.3% MtF, 76.3% FtM).
Socio-demographical and anthropometric data as age, weight, BMI, nationality, and smoker status were collected. Analytical assessment included general parameters (glycemia, hepatic profile and renal function), blood cell count, lipid profile, LH, FSH, estradiol, testosterone, free thyroxine, TSH and prolactin. Moreover, in the first assessment, we also evaluated androstendione and dehydroepiandrosterone, as well as other steroids and karyotype if suitable, in order to exclude disorders of sex development.
Prior to the visit with the endocrinologist, individuals were assessed by mental health professionals in order to confirm the diagnosis. During the first visit with the endocrinologist a complete clinical record including anamnesis, anthropometric and biochemical evaluation were performed. Other coexistent diagnosis, such as hypertension, diabetes mellitus and dyslipemia, as well as drugs prescribed for these conditions were recorded. Hypertension was considered whenever the patient was already on antihypertensive drugs at baseline, or when this diagnosis was established according with standard clinical practice either on the first visit or along follow-up. Diabetes was diagnosed following the American Diabetes Association criteria. They were asked about previous hormonal treatment either on their own or under other physician control. Afterwards, they were informed about the objectives of CHT, possible side effects and different therapeutic options available, and they signed an informed consent for CHT and to include their data in later analysis along follow-up. Then, CHT was started, or changes were made on the prior therapy, if advisable.
The patients were prescribed personalized treatment according to their characteristics and preferences. In general terms, FtM transsexuals received testosterone preparations either as transdermal gel (Testim®, Testogel®, gel 50mg/5g per day) or by intramuscular route (Reandron® – testosterone undecanoate – 1000mg every 3 months). However, initial dose was individualized according to weight and clinical characteristics and later adjusted on the basis of analytics results, aiming at testosterone serum levels within normal range for male adults, and clinical response.
MtF transsexuals not treated previously generally started with oral estrogenic compounds (conjugated equine estrogens or estradiol valerate, depending on their availability), and an antiandrogen with low progestational action (either cyproterone in most cases, or flutamide occasionally, in individualized doses). During follow up, antiandrogenic treatment was progressively removed if clinically possible. Patients older than 40 years were recommended to either start treatment with transdermal estrogens or to switch from oral to transdermal route.
Data are shown as mean (±standard deviation) or proportions. Comparisons between means were done by t-Student for paired or not paired quantitative data as appropriate and by Chi-square for qualitative variables. p≤0.05 was considered statistically significant. Statistical analysis was performed with SPSS Statistics 17.0 software (SPSS Inc., Chicago, IL). The local Ethics Committee approved the study.
ResultsWe evaluated 247 transsexuals, 150 MtF (60.7%) and 97 FtM (39.3%) between 2006 and 2010. The mean age was 30.9±9.7 years (age between 12 and 61 years). A percentage of 73.7% (182) were Spanish, while most of the remaining 26.3% were from Central or South America. Regarding smoking status, 48.6% (121) were current smokers, 10.9% (27) former smokers and 39.7% (99) were non-smokers. A total of 44.5% of patients (110) had started treatment before the first visit in our unit, in most cases with consecutive use of many different compounds.
In relation to cardiovascular risk profile at baseline in the whole cohort, BMI was 24.1±4.3kg/m2, while both blood pressure levels, and basal glucose and lipid profile were within the normal range. 23.3% of individuals were overweight (BMI>25kg/m2) and 9.7% had obesity (BMI>30kg/m2). Only 0.4% (1 individual) had hypertension and 2% (5 individuals) had diabetes (one of them had type 1 diabetes) (Table 1).
Baseline characteristics and differences between male to female (MtF) and female to male (FtM) transsexuals.
| Total cohort | MtF | FtM | p valuea | |
|---|---|---|---|---|
| Age (years) | 30.9±9.7 | 32.4±10.1 | 28.6±8.6 | .002 |
| Weight (kg) | 68.0±13.4 | 70.7±12.7 | 64.3±13.4 | <.001 |
| BMI (kg/m2) | 24.1±4.3 | 24.1±4.1 | 24.0±4.7 | ns |
| NationalitySpanish (%) | 73.7 | 64.7 | 87.6 | <.001 |
| Current smoker (%) | 48.6 | 41.3 | 59.8 | .025 |
| Previous CHT (%) | 44.5 | 64.7 | 13.4 | <.001 |
| Systolic pressure (mmHg) | 119.8±12.3 | 120.8±12.8 | 118.3±11.5 | ns |
| Diastolic pressure (mmHg) | 75.2±9.6 | 75.8±9.6 | 74.3±9.5 | ns |
| Hypertension (%) | 0.4 | 0.7 | 0 | ns |
| Total cholesterol (mg/dL) | 163.3±31.7 | 163.3±30.1 | 163.4±33.5 | ns |
| Triglycerides (mg/dL) | 83.9±60.1 | 94.4±71.6 | 67.7±29.4 | .001 |
| LDL cholesterol (mg/dL) | 100.8±26.3 | 101.6±25.5 | 99.7±27.7 | ns |
| HDL cholesterol (mg/dL) | 47.1±12.1 | 44.7±11.7 | 50.8±11.9 | <.001 |
| Diabetes (%) | 2.0 | 1.3 | 3.1 | ns |
| Overweight (%) | 23.3 | 24.8 | 21.2 | ns |
| Obesity (%) | 9.7 | 7.4 | 12.9 | ns |
CHT: cross-sex hormone treatment.
As shown in Table 1, FtM transsexuals were younger (28.6±8.6 vs. 32.4±10.1 years; p=0.002), were more often Spanish (87.6% vs. 64.7%, p<0.001), they included more current smokers (59.8% vs. 41.3%, p=.025) and had started prior CHT less often than MtF (13.4% vs. 64.7%, p<0.001). As for the lipid profile, FtM had lower triglycerides levels (67.7±29.4 vs. 94.4±71.6mg/dL; p=0.001) and higher HDL cholesterol levels (50.8±11.9 vs. 44.7±11.7mg/dL; p<0.001). There were no statistically significant differences in percentage of diabetic, hypertensive, overweight and obese individuals.
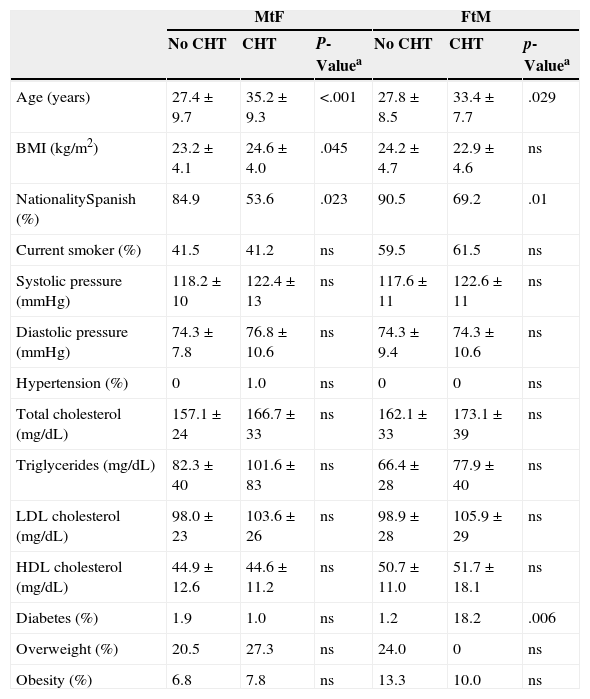
Baseline differences according to previous treatment or notAs we have said previously, CHT before our assessment was significantly more frequent among MtF than FtM. Moreover, we observed a higher percentage of individuals with previous treatment among transsexuals of foreign origin than in Spanish individuals (82.1 vs. 33.5%; p<0.001). There were no baseline differences in prevalence of obesity, hypertension, diabetes, smoking habit among these groups, but transsexuals with previous CHT had higher triglyceride concentrations and higher systolic blood pressure (99.1±80.1 vs. 72.1±33.6mg/dL; p<0.001 and 122.4±13.7 vs. 117.8±10.9mmHg; p=0.001) than naïves.
In MtF transsexual group, previously treated individuals were older than treatment-naïve subjects (35.2±9.3 vs. 27.4±9.7 y; p<0.001) (Table 4). They had higher BMI (24.6±4.0 vs. 23.2±4.1kg/m2; p=0.045) and lower testosterone and hemoglobin levels (400.5±374.2 vs. 556.1±242.2ng/dl; p=0.07 and 14.6±1.2 vs. 13.8±1.2%; p=0.01, respectively). There were no differences in lipid profile, prevalence of hypertension, diabetes nor smoking habit among these groups.
As for the FtM transsexual group, there were differences between pre-treated and treatment-naïve individuals in relation to age, which was lower in those without previous treatment (27.8±8.5 vs. 33.4±7.7 years; p=0.029), testosterone levels, lower in the same subgroup (50.6±23.9 vs. 375.7±341.2ng/dl; p=0.01) and prevalence of diabetes (1.2% vs. 18.2%; p=0.006).
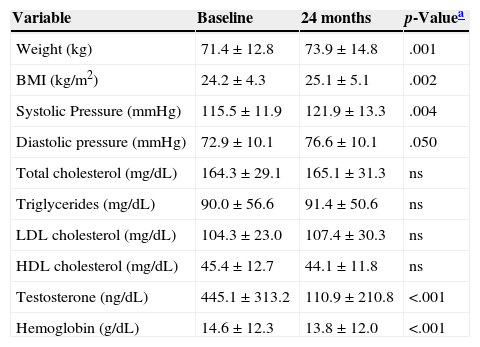
Changes during follow up in MtF transsexualsTable 2 shows an increase in weight and BMI (71.4±12.8 vs. 73.9±14.8kg; p=0.01 and 24.2±4.3 vs. 25.1±5.1kg/m2; p=0.002, respectively) during 24 months follow-up without increase in the proportion of obese individuals, as well as an increase in systolic and diastolic blood pressure (115.5±11.9 vs. 121.9±13.3mmHg; p=0.004 and 72.9±10.1 vs. 76.6±10.1mmHg; p=0.050, respectively), even though blood pressure levels remained within the normal range. No significant differences in lipid profile for any of the assessed parameters (total cholesterol – TC, triglycerides – TG, LDL and HDL cholesterol) were observed. There was a decrease in testosterone and hemoglobin levels as a consequence of estrogenic and anti-androgenic treatment.
Changes over 24 months in cardiovascular risk factors in male to female (MtF) transsexuals.
| Variable | Baseline | 24 months | p-Valuea |
|---|---|---|---|
| Weight (kg) | 71.4±12.8 | 73.9±14.8 | .001 |
| BMI (kg/m2) | 24.2±4.3 | 25.1±5.1 | .002 |
| Systolic Pressure (mmHg) | 115.5±11.9 | 121.9±13.3 | .004 |
| Diastolic pressure (mmHg) | 72.9±10.1 | 76.6±10.1 | .050 |
| Total cholesterol (mg/dL) | 164.3±29.1 | 165.1±31.3 | ns |
| Triglycerides (mg/dL) | 90.0±56.6 | 91.4±50.6 | ns |
| LDL cholesterol (mg/dL) | 104.3±23.0 | 107.4±30.3 | ns |
| HDL cholesterol (mg/dL) | 45.4±12.7 | 44.1±11.8 | ns |
| Testosterone (ng/dL) | 445.1±313.2 | 110.9±210.8 | <.001 |
| Hemoglobin (g/dL) | 14.6±12.3 | 13.8±12.0 | <.001 |
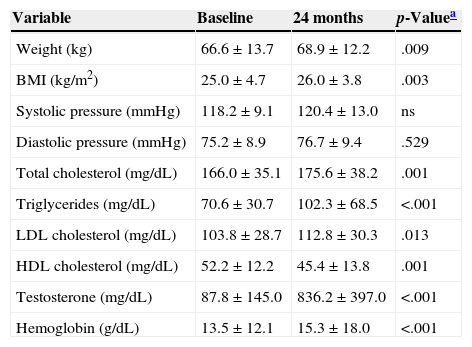
FtM transsexuals also presented an increase in weight and BMI (66.6±13.7 vs. 68.9±12.2kg; p=0.009 and 25.0±4.7 vs. 26.0±3.8kg/m2; p=0.003 respectively) during follow-up without increase in proportion of obese individuals (Table 3), in this group no differences were observed in blood pressure. In relation to lipid profile, general worsening in all the parameters was observed in this group, with increased TC (166.0±35.1 vs. 175.6±38.2mg/dL; p=0.001), triglycerides (70.6±30.7 vs. 102.3±68.5mg/dL; p<0.001) and LDL cholesterol (103.8±28.7 vs. 112.8±30.3mg/dL; p=0.013) and decreased HDL cholesterol (52.2±12.2 vs. 45.4±13.8mg/dL; p=0.001); final levels were all within laboratory reference values for males. There was also an increase in testosterone and hemoglobin levels.
Changes over 24 months in cardiovascular risk factors in female to male (FtM) transsexuals.
| Variable | Baseline | 24 months | p-Valuea |
|---|---|---|---|
| Weight (kg) | 66.6±13.7 | 68.9±12.2 | .009 |
| BMI (kg/m2) | 25.0±4.7 | 26.0±3.8 | .003 |
| Systolic pressure (mmHg) | 118.2±9.1 | 120.4±13.0 | ns |
| Diastolic pressure (mmHg) | 75.2±8.9 | 76.7±9.4 | .529 |
| Total cholesterol (mg/dL) | 166.0±35.1 | 175.6±38.2 | .001 |
| Triglycerides (mg/dL) | 70.6±30.7 | 102.3±68.5 | <.001 |
| LDL cholesterol (mg/dL) | 103.8±28.7 | 112.8±30.3 | .013 |
| HDL cholesterol (mg/dL) | 52.2±12.2 | 45.4±13.8 | .001 |
| Testosterone (mg/dL) | 87.8±145.0 | 836.2±397.0 | <.001 |
| Hemoglobin (g/dL) | 13.5±12.1 | 15.3±18.0 | <.001 |
Baseline differences between transsexuals with and without previous treatment.
| MtF | FtM | |||||
|---|---|---|---|---|---|---|
| No CHT | CHT | P-Valuea | No CHT | CHT | p-Valuea | |
| Age (years) | 27.4±9.7 | 35.2±9.3 | <.001 | 27.8±8.5 | 33.4±7.7 | .029 |
| BMI (kg/m2) | 23.2±4.1 | 24.6±4.0 | .045 | 24.2±4.7 | 22.9±4.6 | ns |
| NationalitySpanish (%) | 84.9 | 53.6 | .023 | 90.5 | 69.2 | .01 |
| Current smoker (%) | 41.5 | 41.2 | ns | 59.5 | 61.5 | ns |
| Systolic pressure (mmHg) | 118.2±10 | 122.4±13 | ns | 117.6±11 | 122.6±11 | ns |
| Diastolic pressure (mmHg) | 74.3±7.8 | 76.8±10.6 | ns | 74.3±9.4 | 74.3±10.6 | ns |
| Hypertension (%) | 0 | 1.0 | ns | 0 | 0 | ns |
| Total cholesterol (mg/dL) | 157.1±24 | 166.7±33 | ns | 162.1±33 | 173.1±39 | ns |
| Triglycerides (mg/dL) | 82.3±40 | 101.6±83 | ns | 66.4±28 | 77.9±40 | ns |
| LDL cholesterol (mg/dL) | 98.0±23 | 103.6±26 | ns | 98.9±28 | 105.9±29 | ns |
| HDL cholesterol (mg/dL) | 44.9±12.6 | 44.6±11.2 | ns | 50.7±11.0 | 51.7±18.1 | ns |
| Diabetes (%) | 1.9 | 1.0 | ns | 1.2 | 18.2 | .006 |
| Overweight (%) | 20.5 | 27.3 | ns | 24.0 | 0 | ns |
| Obesity (%) | 6.8 | 7.8 | ns | 13.3 | 10.0 | ns |
MtF: male to female transexuals.
FtM: female to male transexuals.
CHT: cross hormone therapy.
Along two years under CHT, this population of transsexual individuals of predominant Mediterranean origin or, at least, under the influence of local eating habits, has shown slight changes in some CV risk factors, although these remained within normal range.
In the first place, our study observed that nearly half of the individuals arriving to our unit for the first time have already followed previous CHT; this is specially observed in MtF transsexuals coming from other countries, while it occurs less frequently in Spanish subjects. For obvious reasons, previously treated transsexuals were also found to be older than those who are treatment-naïve for CHT.
Concerning the baseline differences between MtF and FtM they only involved TG (higher in MtF) and HDL cholesterol (higher in FtM), as has also been observed in others studies9 and in general population.
Changes at 6, 12 and 24 months were collected, even though our analysis finally considered the longest period, when more relevant differences were observed. After 2 years of follow-up, both groups increased weight and BMI significantly (but without increasing the proportion of overweight or obese subjects), as has also been described in previous studies,6,9,11 in which changes in fat distribution were observed: in MtF subcutaneous fat increases, with a decreased ratio between visceral and subcutaneous abdominal fat, while in FtM subcutaneous fat decreases and visceral fat increases, thus raising the aforementioned ratio, which confers to this group a higher CV risk. The mechanism underlying these changes is still controversial. Unfortunately, we have not evaluated the body composition in our participants.
In terms of lipid profile, changes were observed in FtM transsexual group with a significant increase in TC, TG and LDL cholesterol and a decrease in HDL cholesterol; yet clinical relevance is uncertain as all parameters remained within normal range. Previous reviews of data from a large Dutch cohort4,11 (18.5 years follow-up) also observed a decrease in HDL cholesterol and an increase in triglycerides without any changes in LDL and TC; however, no increase in CV mortality could be demonstrated. Other studies have not shown increased mortality. A meta-analyses addressing cardiovascular risk in transsexual individuals published by Elamin et al. in 2010,7 including the Dutch cohort, emphasizes the limited methodological quality of the primary studies identified, together with sparse data, limited total sample size and difficulties to evaluate some variables that influence CV risk, especially in relation to FtM transsexuals. Many studies have focused on the relationship between androgens and CV disease, but results are controversial. On the one hand, studies in healthy men suggest that low rather than high endogenous androgen levels are related to coronary heart disease,13 while, on the other hand, a higher CV risk has been observed in women with polycystic ovary syndrome probably due to changes that occur in addition to hyperandrogenism.14,15 Probably, CV risk factors at the final assessment in FtM transsexuals resemble those observed in biological men.
In MtF transsexuals, data about CV profile evolution differ widely among various studies, which have yielded an increase, a decrease or no changes in LDL and HDL cholesterol, and stability or increase in triglycerides levels.9,11,16 The meta-analyses published by Elamin in 2010 only showed a slight increase in TG levels without any changes in other parameters.7 Anyway, this variation remains within the normal range, without a clear clinical relevance in spite of its statistical significance. In our study, no changes in parameters of lipid profile in MtF were observed. Although these data reflect that there are probably no differences, we have to take into account that >60% of our MtF population had been on treatment previous to our medical control, and possible previous effects may attenuate further changes. However, results from other cohorts have not been able to consistently confirm changes. Regarding mortality data, Gooren's study showed an increase in CV cause mortality in this group; however, data subanalysis pointed out that this increase was concentrated in individuals on ethynilestradiol as estrogenic source, while not present in transsexuals treated with other compounds. Moreover, data from Sweden point out those sex-reassigned transsexuals of both genders have about three times higher risk of all-cause mortality than controls.17 Yet this increase is mainly due to suicide, and in a very lesser grade to CV disease. As it reflects a very long period of time, it can be assumed that initial therapies in the seventies were quite different from those prescribed in more recent times.
To our knowledge, this is the first study from our geographic area that analyses lipid profile and other CV risk factors in MtF and FtM transsexuals under CHT. Data seem to indicate no increase in CV risk factors in MtF transsexuals that are treated with currently used estrogenic compounds, while a slight worsening in lipid profile takes place in the FtM group, presumably of little clinical consequence.
However, the limitations of our study are several, including that almost 30% of our population came from other countries and 45% were taking CHT before our assessment, especially among MtF transsexuals; therefore our sample is less uniform than desirable for drawing relevant conclusions. Moreover, a longer follow-up, beyond 2 years, would have helped us to see whether changes in lipid profile as well as in other CV risk factors become more pronounced than those observed in this period, and to assess the appearance of CV events. In addition, we do not have a control group to compare our results, which would have increased the relevance of our results.
Thus, according with present knowledge we may conclude that CHT under medical surveillance in transsexual individuals seems to be acceptably safe regarding cardiovascular profile. Nevertheless, due to the scarcity of data in this area, well-designed, prospective studies with long term strict follow up are required to evaluate not only surrogate markers, but also the occurrence of cardiovascular events in this group of individuals.
Conflict of interestThe authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.