Diseases associated with maldigestion or intestinal malabsorption may be associated to hypovitaminosis E, defined as plasma vitamin E levels less than 5μg/mL. This may cause hemolytic anemia, decreased immune response and fertility, and neuromuscular involvement, including ataxia, due to impairment of the spinocerebellar tract with variable peripheral nerve involvement. This impairment is due to loss of the protective effect of vitamin E against neurotoxic agents.1
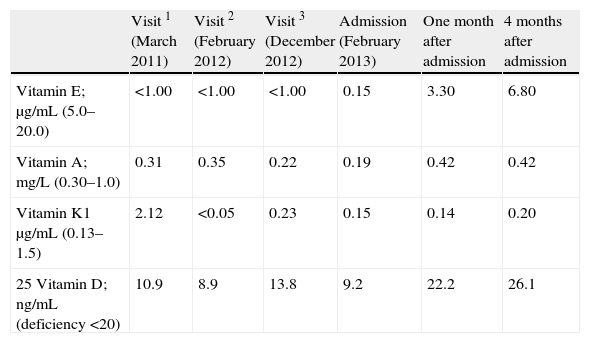
We report the case of a 38-year-old male patient with a personal history of celiac disease (pathological report of bowel biopsy: Marsh type 3c lesion) and malabsorptive syndrome probably related to chronic dietary transgression. The patient was referred to the nutrition clinic for moderate weight loss, with one to four daily episodes of diarrhea, occasional food residues in feces, dyspepsia, and abdominal distention after food intake. Laboratory test results included negative transglutaminase antibodies and decreased levels of zinc, cholesterol, and lipid soluble vitamins A, D, and E. Dietary supplements and a multivitamin preparation were therefore prescribed. The patient experienced no clinical or anthropometrical improvement, and pancreatic enzymes were added to verify diagnosis. At the next visit, patient reported clinical improvement, and other causes of maldigestion/malabsorption were ruled out. However, despite weight gain at successive visits and mild improvement in intestinal symptoms, levels of lipid soluble vitamins did not increase, and vitamin K and folate deficiency was also found. Replacement of lipid soluble vitamins and folic acid was prescribed, but at four months the patient was admitted to the neurology department for subacute gait ataxia with hemispheric cerebellar syndrome, vertical nystagmus, and signs consistent with posterior cord syndrome. Supplemental tests performed at that time showed deficiency of lipid soluble vitamins, signs of cerebellar hemispheric atrophy with normal neurophysiological study, and pathological examination of intestinal biopsy with no improvement as compared to the previous one, together with an increased inflammatory component. The etiology of the neurological picture was related to vitamin E deficiency, which had to be administered by the subcutaneous route because of failure of oral supplementation, suspected to be malabsorbed. After admission, ataxia clearly improved, which even allowed the patient to perform routine physical exercise, and paresthesia disappeared at the same time as levels of lipid soluble vitamins reached the normal range (treatment at that time: multivitamin, 16,000IU every 48h of 25-OH-vitamin D (calcifediol), 2mg PO of vitamin K (phytomenadione) every 15 days, 800mg PO of vitamin E (tocoferol) daily together with 100mg weekly by the parenteral route, and 50,000IU of vitamin A (retinol) PO every 48h). There were no clinical manifestations of the deficiency in other lipid soluble vitamins (change over time in lipid soluble vitamins in Table 1).
Change over time in serum levels of lipid soluble vitamins.
| Visit 1 (March 2011) | Visit 2 (February 2012) | Visit 3 (December 2012) | Admission (February 2013) | One month after admission | 4 months after admission | |
| Vitamin E; μg/mL (5.0–20.0) | <1.00 | <1.00 | <1.00 | 0.15 | 3.30 | 6.80 |
| Vitamin A; mg/L (0.30–1.0) | 0.31 | 0.35 | 0.22 | 0.19 | 0.42 | 0.42 |
| Vitamin K1μg/mL (0.13–1.5) | 2.12 | <0.05 | 0.23 | 0.15 | 0.14 | 0.20 |
| 25 Vitamin D; ng/mL (deficiency <20) | 10.9 | 8.9 | 13.8 | 9.2 | 22.2 | 26.1 |
Vitamin E or α-tocoferol is a lipid soluble vitamin with an antioxidant action, thus significantly decreasing oxidative stress and inflammation. It is essential in biological membrane stabilization (protects polyunsaturated fatty acids in cell membranes from peroxidation), and is involved in the platelet aggregation mechanism and hemolysis. It is naturally found in food, while the rest is provided as supplements and fortified foods. Vitamin E is absorbed in the middle portion of the small bowel in the presence of biliary salts and pancreatic lipase, and its absorption therefore depends on the capacity of the individual to absorb fat.
In addition to increased intake of food rich in the vitamin, deficiency is treated by administering vitamin E by the oral route (at doses of 800–1000mg/día or even up to 100mg/kg/day if there is coexistent severe steatorrhea), or by the parenteral route if intestinal absorption is erratic (10–300mg weekly).2
Celiac disease or gluten-sensitive enteropathy is characterized by nutrient malabsorption, lesion in small bowel mucosa, and rapid clinical and histological improvement when gluten is removed from diet.3 It is an immune disorder triggered by an environmental agent (gliadin in gluten). Patients may have classical malabsorption symptoms such as diarrhea, steatorrhea, and flatulence, which may lead to weight loss, severe anemia, and deficiency conditions due to lack of micronutrients.4 In these patients, vitamin E deficiency may cause neurological signs such as cerebellar ataxia and posterior cord syndrome, consisting of dysmetry, dysdiadochokinesia, and impaired proprioceptive sensitivity, mainly in lower limbs, and paresthesia.5 Early neurological changes (hyporeflexia, posterior cord syndrome, cerebellar ataxia, vertical nystagmus) are usually reversible with early vitamin replacement, but late changes such as dysarthria, dysphagia, ophthalmoplegia, or cognitive impairment are not reversible.1,6
On the other hand, celiac disease may be associated to exocrine pancreatic insufficiency, whose clinical signs may overlap to those of celiac disease and which may improve with a strict fat-free diet or with pancreatic enzymes. Supplemental tests such as those of fecal elastase or fat are poorly conclusive for diagnosis. Therefore, a trial of treatment with pancreatic enzymes may be done in some cases to assess response.7,8
Intestinal biopsy is essential for diagnosis and to check the effects of specific treatment. Our patient showed a poor progress in pathological results because of his poor compliance with gluten-free diet.9
Gluten-free diet is the cornerstone in treatment for celiac disease, and the main cause for lack of improvement is non-adherence to diet. This is very important, because non-compliance may lead to malabsorption and vitamin and mineral deficiencies, causing conditions such as those reported in our case and which may become permanent and require lifetime replacement therapy.10
It should be stressed that, in addition to the already discussed gastrointestinal and nutritional complications, therapeutic transgression may also promote the occurrence of neoplastic degeneration, especially intestinal T lymphomas.9
Please cite this article as: Suárez Llanos JP, González Melo E, Mora Mendoza A, Iacampo Leiva LD, Moro Miguel MA. Celiaquía y malabsorción: a propósito de un caso de ataxia secundaria a déficit de vitamina E. Endocrinol Nutr. 2014;61:389–390.