The finding of a thyroid nodule is a very common occurrence in clinical practice. Management of thyroid nodules requires a multidisciplinary approach that may be eased by a high-resolution thyroid nodule clinic. We report our clinical experience and outcomes in a high-resolution thyroid nodule clinic.
Patients and methodsAll patients referred to Virgen de la Victoria Hospital (Málaga) from 2005 to 2007 were evaluated following thyroid nodule guidelines. Statistical analysis was performed using SPSS software.
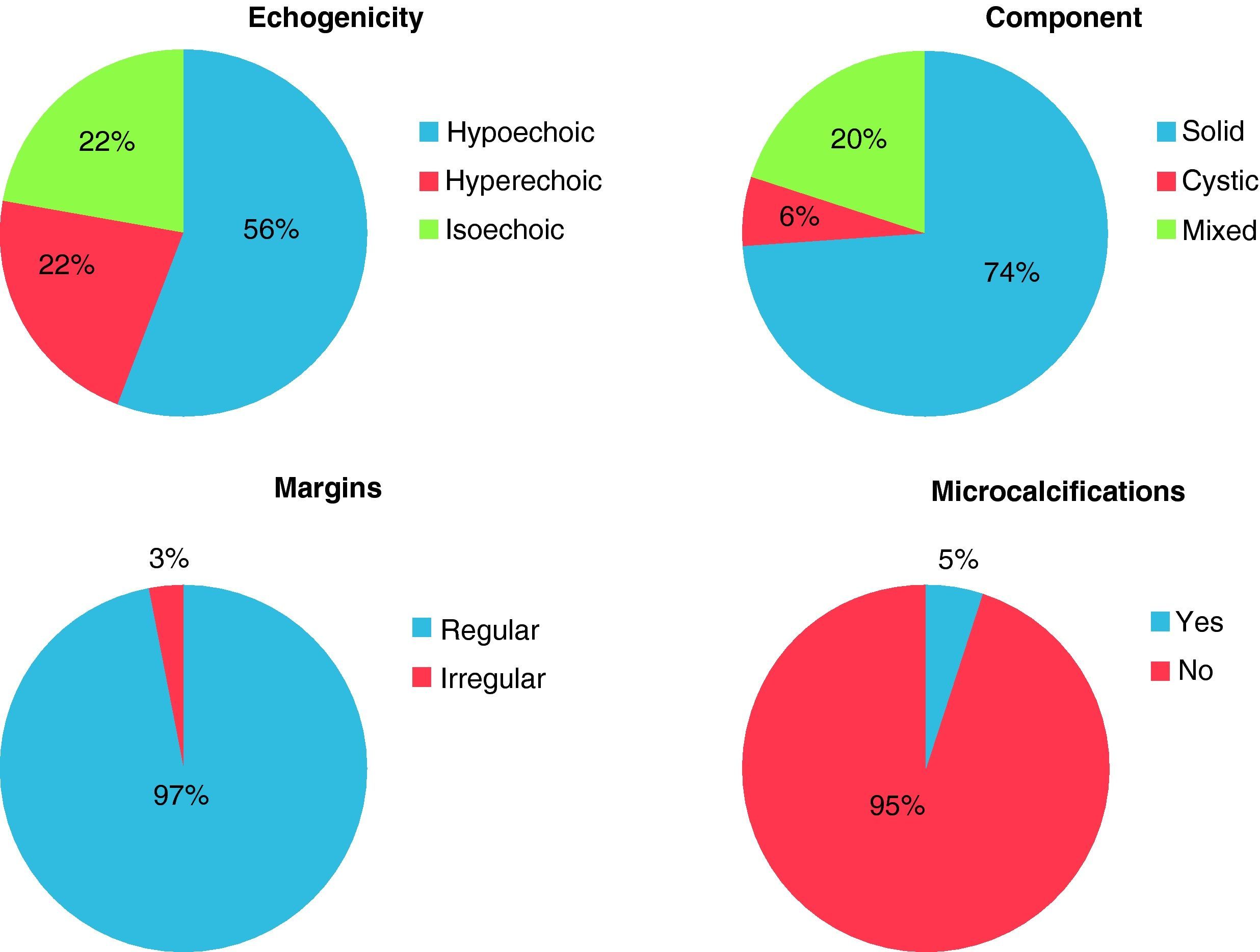
ResultsIn the study period, 658 patients (mean age 48.6 years, 89.8% females) were seen at the thyroid nodule clinic. Thyroid nodules were discovered in 85.5% of patients. Mean nodule diameter was 1.96cm. Of these nodules, 74.2% were solid, 55.8% hypoechogenic, and 4.7% showed microcalcifications. Fine needle aspiration (FNA) was performed in 475 patients (76.5% of all cytological samples were benign, 19.1% had suspected malignancy, 2.1% were malignant, and 2.3% inadequate). Referral for surgery was required in 23.3% of patients (mainly because of nodule size or suspected malignancy). Malignancy was confirmed in 24.9% of nodules. Sensitivity and specificity of cytology (considering biopsy as gold standard) were 81.8% and 94.7% respectively.
ConclusionsImplementation of a high-resolution thyroid nodule clinic decreases delay in diagnosis and optimizes available resources, thus providing for satisfactory clinical outcomes.
El hallazgo de un nódulo tiroideo es un hecho muy frecuente en la práctica clínica habitual. El manejo del nódulo tiroideo necesita un abordaje multidisciplinar que puede ser facilitado con la creación de unidades de alta resolución de nódulo tiroideo. Describimos la experiencia clínica y los resultados obtenidos en una consulta de alta resolución y acto único de nódulo tiroideo.
Material y métodosSe han evaluado todos los pacientes derivados a la consulta de nódulo tiroideo del Hospital Virgen de la Victoria (Málaga) desde el año 2005 al 2007. Se han seguido las guías de práctica clínica de nódulo tiroideo para la recomendación de punción aspirativa con aguja fina (PAAF) y cirugía tiroidea. Se realizó análisis estadístico con programa SPSS.
ResultadosDurante el periodo de estudio, la consulta de nódulo tiroideo atendió a 658 pacientes (edad media 48,6 años, 89,8% mujeres). Mediante ecografía se confirmó la existencia de nódulo tiroideo en el 85,5% de los pacientes. Con un diámetro medio de 1,96cm, un 74,2% de nódulos fueron sólidos, un 55,8% hipoecoicos, y un 4,7% presentaron microcalcificaciones. Se realizó la PAAF a 475 pacientes. El 76,5% de las citologías fueron benignas, el 19,1% sospechosas, el 2,1% malignas y el 2,3% insuficientes. Se derivó a cirugía al 23,3% de los pacientes (principalmente por tamaño nodular o sospecha de malignidad). Se confirmó la existencia de patología maligna (principalmente carcinoma papilar) en el 24,9% de los nódulos intervenidos. La sensibilidad/especificidad de la citología (considerando la biopsia como el gold standard) fue del 81,8 y el 94,7%, respectivamente.
ConclusionesLa instauración de una consulta monográfica de nódulo tiroideo permite la optimización de recursos y reduce la demora diagnóstica, obteniendo unos resultados clínicos ampliamente satisfactorios.
Thyroid nodule is a very common condition in clinical practice. Its prevalence increases linearly with age, radiation exposure, and iodine deficiency, and is much more common in females as compared to males (estimated ratio, 10:1).1
Most thyroid nodules are benign in nature, but approximately 5% may be malignant.2 This small but significant malignancy rate should lead to a systematic and structured work-up of all thyroid nodules found in clinical practice, always with the aim of achieving the maximum diagnostic yield with the lowest chance of iatrogeny.3
Thyroid nodule management should involve the coordinated work of several specialists, including specialists in thyroid disease, thyroid ultrasound, and thyroid cytopathological examination. The close collaboration of these experts is indispensable if the best results from thyroid nodule work-up are to be achieved.
The accumulation of diagnostic tests and medical visits sometimes causes a substantial delay in results which may impair nodule prognosis. It also involves multiple visits, work time loss, and patient discomfort. Centralization of thyroid nodule care in a monographic clinic largely obviates these disadvantages.
For this reason, a high-resolution thyroid nodule clinic was created in 2005 at Hospital Virgen de la Victoria (Malaga). Professionals involved were organized, and referral and monitoring criteria were established.
Having gained substantial clinical experience, we report the results obtained in the first 2 years of operation of this high-resolution thyroid nodule clinic.
Patients and methodsThe main objective of this study is to report the clinical results achieved at the thyroid nodule clinic of the Clinical Management Unit of Endocrinology and Nutrition of Hospital Virgen de la Victoria (Malaga) from October 2005 to December 2007 inclusive. Secondary objectives include assessment of the sensitivity and specificity of fine needle aspiration (FNA) and of the correlation between cytological atypia and histological results.
The thyroid nodule clinic, which started operation in October 2005, is designed as a high-resolution monographic clinic. It is a multidisciplinary clinic staffed by one endocrinologist, three radiologists, and two pathologists. Patients with clinically suspected thyroid nodule referred from primary or specialized care are seen at the clinic.
The first step in care for these patients was thyroid ultrasound examination by the X-ray department. Once images were obtained and the relevant ultrasonographic report was prepared, the patients underwent clinical examination at the endocrinology department. The patients provided their basic thyroid laboratory test results (requested by the referring physicians), including thyroid-stimulating hormone (TSH) and free thyroxine (T4) levels. After a complete history, physical examination, and assessment of laboratory results, together with ultrasonographic findings, a decision was taken about the suitability of FNA. Ultrasonographic criteria for performing FNA in a nodule agreed with those of the American Thyroid Association4 (ATA) and the American Association of Clinical Endocrinologists/Associazione Medici Endocrinologi5 (AACE/AME) guidelines and mainly included nodule size, the type of associated component (solid-mixed-cystic), the presence of microcalcifications, echogenicity, and nodule margin characteristics.
If FNA was advisable (and after the signature of informed consent and clarification of any potential doubts), the patient returned to the X-ray department, where ultrasound-guided FNA was performed (jointly by the pathologist and radiologist). Samples were sent to the pathology department, and cytological results were available in a week.
Once the FNA results were received, the patients received by post a complete clinical report including the ultrasonographic and cytological results, the diagnosis made, and the treatment proposed. An appointment visit (if needed) was also enclosed. If any finding suggested malignancy or if the sample was inadequate, the patients were contacted by telephone to arrange for surgery or a repeat FNA as soon as possible.
TSH and free T4 levels were measured using a chemiluminescence immunoassay method and read in a Siemens Dimension Vista 1500 autoanalyzer. Normal values: TSH 0.2–4.2μIU/mL, free T4 0.7–1.55ng/dL.
A Siemens Sonoline Sienna ultrasound system with a 7.5MHz probe was used for thyroid ultrasound examination.
Thyroiditis was diagnosed based on ultrasound when the thyroid gland showed a heterogeneous echo structure, diffuse hypoechogenicity, and fibrotic septa resembling pseudonodular images.
FNA was performed using a 21G needle (0.8mm) attached to a 20mL plastic syringe. The procedure was done under ultrasonographic guidance using a perpendicular puncture and without local anesthesia. Once the needle tip was placed in the appropriate area, aspiration was started, one sample being taken from each nodule. Once the sample was obtained, it was placed on a glass slide. For Papanicolaou staining, the smear was rapidly fixed with 95% ethanol before drying. In air-dried smears, staining was performed with one of the modified Romanowsky–Malachowsky methods using traditional (Wright, Giemsa, Leishman, MGG) or rapid panoptic (DIFF-QUICK, QCA, MGGQUICK) stains.
An adequate sample was defined as one containing at least six groups of cells with ten follicular cells each, arranged in a monolayer, and well seen in the preparation.
Statistical analysisSPSS software (version 13.0, Chicago, USA) was used for statistical data analysis.
The main variables tested were:
- -
Characteristics of the population (age, sex, prior thyroid disease, hormone function).
- -
Source of referral.
- -
Nodule finding.
- -
Ultrasonographic diagnosis (normal, nodular goiter, multinodular goiter, thyroiditis).
- -
Nodule characteristics (size, echogenicity, component type, microcalcifications, margins).
- -
Indications for FNA.
- -
Results of cytological examination (benign, malignant, suspect, inadequate)
- -
Indication for surgery.
- -
Agreement between cytology and surgical specimen biopsy.
Data are given as mean±standard deviation, and 95% confidence intervals have been calculated for quantitative variables. Qualitative variables are given as absolute numbers and percentages.
The association between the qualitative variables was analyzed using a Chi-square test. A Student's t-test was used to compare quantitative variables. Non-parametric tests were used for non-normally distributed variables. p-Values were given for associations in which statistical significance was detected. A value of p<0.05 was considered statistically significant.
The result of biopsy is considered as the gold standard for estimating the diagnostic validity values of cytology.
ResultsDuring its first 2 years of operation, the thyroid nodule clinic was attended by 658 patients, who were referred mainly for suspected nodular disease or goiter.
Most patients seen at the thyroid nodule clinic were directly referred by the department of endocrinology and nutrition (51.4%) and, to a lesser extent, by primary care (39.4%) and other hospital departments (usually internal medicine, pneumology, oncology, and neurology) (9.2%).
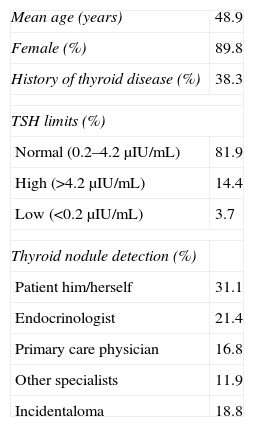
Table 1 shows the characteristics of the study population.
Characteristics of study population.
| Mean age (years) | 48.9 |
| Female (%) | 89.8 |
| History of thyroid disease (%) | 38.3 |
| TSH limits (%) | |
| Normal (0.2–4.2μIU/mL) | 81.9 |
| High (>4.2μIU/mL) | 14.4 |
| Low (<0.2μIU/mL) | 3.7 |
| Thyroid nodule detection (%) | |
| Patient him/herself | 31.1 |
| Endocrinologist | 21.4 |
| Primary care physician | 16.8 |
| Other specialists | 11.9 |
| Incidentaloma | 18.8 |
TSH: Thyroid-stimulating hormone.
Thyroid ultrasound examination was normal in 5.1% of patients (n=34), and showed non-nodular thyroid pathology in 9.2% (n=61) of patients and nodular thyroid pathology in 85.5% (n=563). Of patients with nodular pathology, 53.5% (n=301) had multinodular goiter, 26.5% (n=149) simple nodular goiter, 11.2% (n=63) nodular goiter with thyroiditis, and 8.8% (n=50) micronodules (nodules less than 1cm in size). Among patients with no nodular disease, the most common findings were thyroiditis (93.4%, n=57) and diffuse goiter (6.6%, n=4).
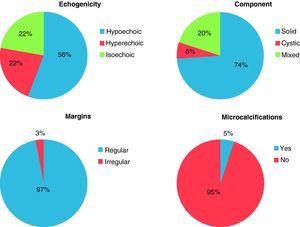
Mean thyroid nodule size was 1.96±1.04cm (95% CI 1.87–2.05cm). Most nodules were hypoechoic, solid, and with regular margins (Fig. 1).
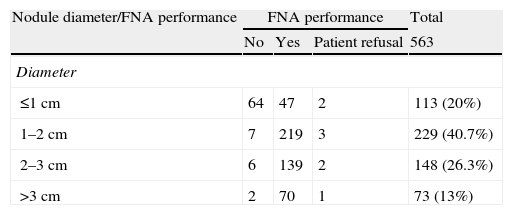
FNA was recommended for 475 nodules because of their ultrasound characteristics, size, and prior history. Less than 50% of nodules smaller than 1cm were amenable to FNA, while 95% of nodules greater than 1cm were punctured (Table 2). Solid nodules were punctured to a greater extent (94.6%) than mixed nodules (80.4%) or pure cystic nodules (66.6%). All nodules with microcalcifications or irregular margins were punctured (n=30). Echogenicity did not influence the performance of FNA.
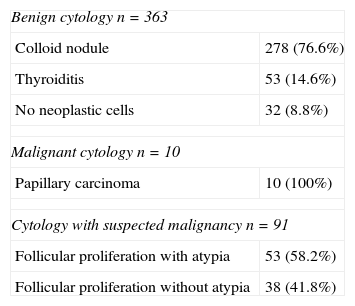
Based on the pathological study, 76.5% of cytologies were rated as benign, 19.1% as suspected malignancy, 2.1% as malignant, and 2.3% of samples as inadequate for diagnosis (Table 3).
Distribution of cytological results.
| Benign cytology n=363 | |
| Colloid nodule | 278 (76.6%) |
| Thyroiditis | 53 (14.6%) |
| No neoplastic cells | 32 (8.8%) |
| Malignant cytology n=10 | |
| Papillary carcinoma | 10 (100%) |
| Cytology with suspected malignancy n=91 | |
| Follicular proliferation with atypia | 53 (58.2%) |
| Follicular proliferation without atypia | 38 (41.8%) |
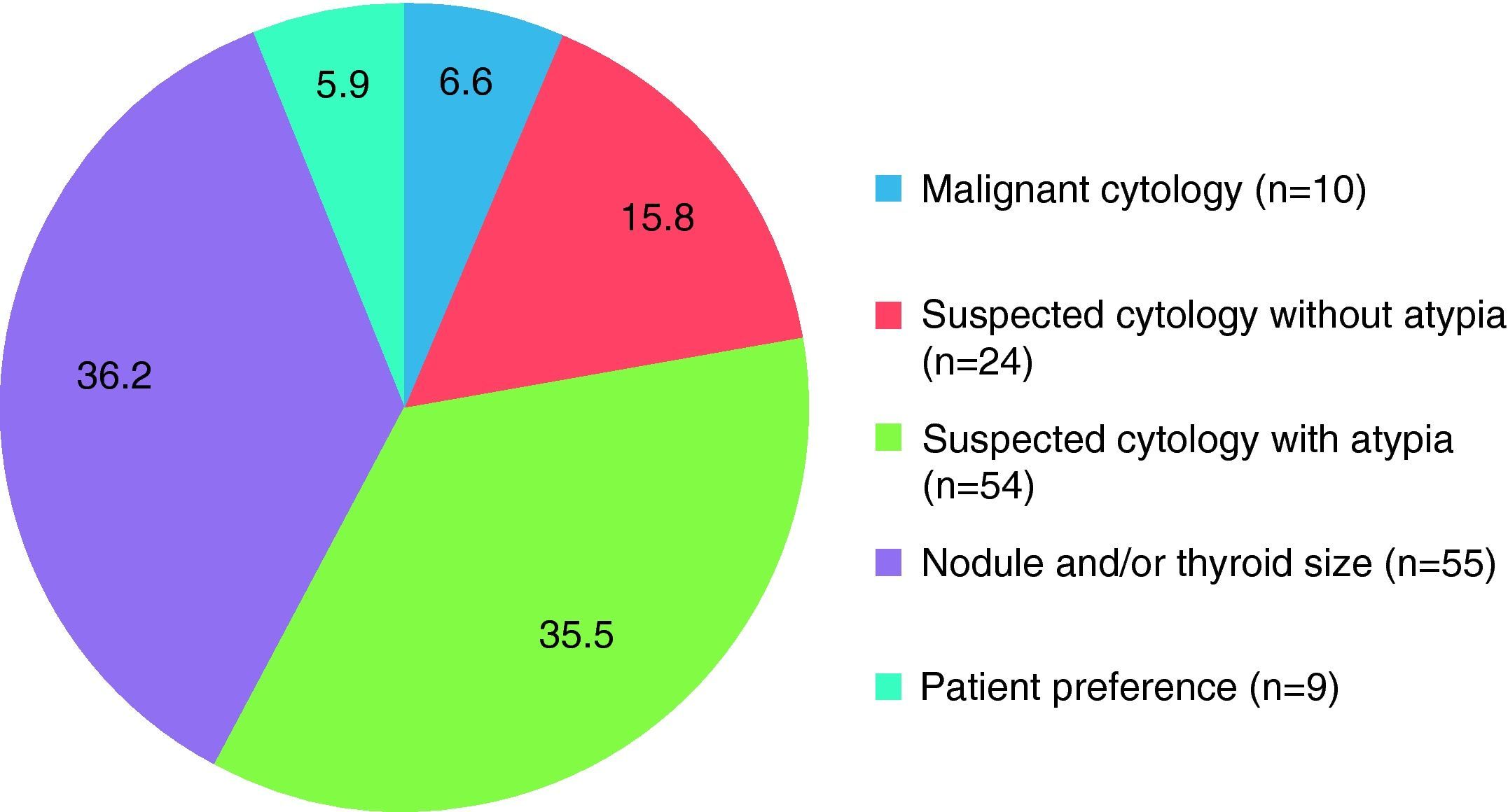
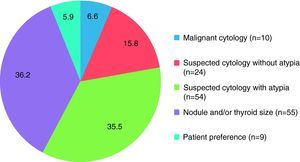
Surgery was recommended for 152 patients. The main reasons for indicating surgery were nodule size (mean size of nodules referred for surgery: 3.3±0.8cm) and malignant or suspected malignant cytology (with and without atypia) (Fig. 2).
All malignant cytologies and cytologies with suspected malignancy and atypia were referred for surgery. Seventy percent of cytologies with suspected malignancy but no atypia were referred for surgery.
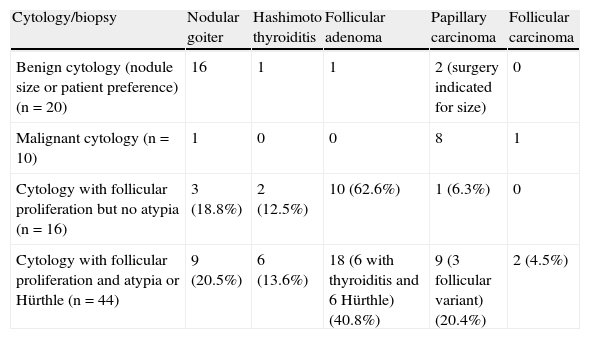
Until the last data collection date (November 2008), 91 patients had undergone surgery (60.1% of all patients referred for surgery). Surgery confirmed that 74.1% of thyroid nodules were benign and 24.9% were malignant. Table 4 shows the results of surgical specimen biopsy.
Cytology/biopsy correlation.
| Cytology/biopsy | Nodular goiter | Hashimoto thyroiditis | Follicular adenoma | Papillary carcinoma | Follicular carcinoma |
| Benign cytology (nodule size or patient preference) (n=20) | 16 | 1 | 1 | 2 (surgery indicated for size) | 0 |
| Malignant cytology (n=10) | 1 | 0 | 0 | 8 | 1 |
| Cytology with follicular proliferation but no atypia (n=16) | 3 (18.8%) | 2 (12.5%) | 10 (62.6%) | 1 (6.3%) | 0 |
| Cytology with follicular proliferation and atypia or Hürthle (n=44) | 9 (20.5%) | 6 (13.6%) | 18 (6 with thyroiditis and 6 Hürthle) (40.8%) | 9 (3 follicular variant) (20.4%) | 2 (4.5%) |
A histological result of malignancy was found in 20% of cytologies with suspected malignancy. The presence of atypia in the cytology increased the malignancy rate. Twenty-five percent of cytologies with suspected malignancy and atypia were confirmed as malignant (11/44), while only 6.2% of cytologies with suspected malignancy but no atypia were confirmed as being malignant (1/16).
A correlation was found between the results of cytology and biopsy. Taking biopsy as the gold standard, cytology had 81.8% sensitivity, 94.7% specificity, a positive predictive value of 90%, and a negative predictive value of 90%.
No association was found between the presence of microcalcifications, the type of component, and the finding of malignancy in the biopsy. However, a relationship was found between irregular margins, hypoechogenicity, and risk of malignancy (p<0.05). No association was found between nodule number and the presence of malignancy. An association was found (p=0.014) between nodules with at least one ultrasonographic malignancy criterion and subsequent confirmation of malignancy in the biopsy. If there was at least one ultrasonographic malignancy criterion, the risk of malignancy at biopsy was three-fold greater than when no malignancy criterion existed [OR=3.5; 95% CI (1.25; 10.08)]. A higher malignancy rate was found in males as compared to females (36% versus 23%, p<0.05).
Incidentalomas were found in 18.8% of cases, with a distribution of cytological diagnoses, surgical indication rate, and distribution of pathological results similar to the overall series.
DiscussionThyroid nodules are very common in the general population. In approximately 4–8% of adults, nodules are detected by palpation and in 13–67%, nodules are detected by ultrasonography, while nodule prevalence at necropsy increases to almost 50%.6,7
Various epidemiological studies have shown thyroid nodules to be more common in females as compared to males and at ages ranging from 30 to 59 years.8 They are also common in iodine-deficient areas and in patients with a history of head and neck irradiation in childhood.9
Thyroid nodule incidence has doubled in recent decades. This increase is directly related to the increased use of cervical ultrasonography and other imaging tests (CT, MRI, PET).10 In our series, approximately one fifth of all nodules detected were incidentalomas.
Because of this increased prevalence, different societies have issued clinical practice guidelines providing comprehensive discussions of thyroid nodule diagnosis, treatment, and follow-up.4,5 However, none of these guidelines addresses the creation of specific thyroid nodule clinics to achieve more specialized management and a better follow-up of patients.
In our view, monographic thyroid nodule clinics represent a step forward in patient care. There are several factors which support our position: the high (and constantly growing) prevalence of thyroid nodule; the need for periodic clinical re-evaluation; the simultaneous involvement of various specialists; patient convenience; and the results, which in our study were similar or even superior to those reported in the literature.
It is essential that specialists working at the thyroid nodule clinic (endocrinologists, radiologists specializing in thyroid ultrasonography, and pathologists with experience in thyroid cytology) maintain a continuous feedback and share a common language. The job security of these specialists involved, which allows a fixed medical team to be maintained (so increasing intraobserver agreement and allowing for consistent medical criteria) is a very important element which should be taken into consideration.
Delay in the diagnostic process is substantially reduced because the whole process is centralized and there is no chance of appointment loss (as all tests are done on the same day). Moreover, less patient visits to the hospital are required, with the resultant reductions in working hours and time lost. For the healthcare system, this type of clinic allows for a more efficient use of the available resources and avoids appointment duplicity.
The clinical results achieved are very similar to those recently reported. According to the literature,11 approximately 60–70% of thyroid aspirates are benign, 15–25% are indeterminate, 5–15% are not useful for diagnosis, and 5% are papillary carcinomas. These figures agree with our results. In this study, clear agreement was found between the results of cytology and biopsy. Taking biopsy as the gold standard, cytology showed 81.8% sensitivity and 94.7% specificity, rates which are both very similar (or even superior) to those reported by other groups.12–14
The routine use of ultrasound-guided FNA is recommended for thyroid nodules because, if cystic or necrotic areas are avoided, the rate of unsatisfactory samples decreases from 15–20% to 5%.15,16 In addition, ultrasound-guided FNA allows for diagnosis in 50–63% of initially unsatisfactory samples.17 This study routinely used ultrasound-guided FNA and had an unsatisfactory sample rate of 2.3%, much lower than that reported in the literature.18
There are a number of ultrasonographic criteria helpful for differentiating malignant from benign nodules. These criteria mainly include shape, margins, echogenicity, and the presence of calcifications.19 A recent review stated that ultrasonographic characteristics alone are not helpful for predicting malignancy or benignity, but when they are combined with cytology, the most accurate and effective results are obtained. In this review, most malignant nodules had more than two ultrasonographic characteristics of malignancy.20 According to this publication, no single ultrasonographic characteristic (size, the presence of microcalcifications, echogenicity, the regularity of margins, or the predominant type of component) was significantly associated with a risk of malignancy, but an association was found when these characteristics were grouped.
The finding of serum TSH levels in the upper limits or above the reference range has recently been associated with an increased risk of malignancy of a thyroid nodule.21 No conclusive data in this regard were found in our series.
Some limitations should be considered when interpreting the results of our study. Since this was a prospective, observational study, our population was selected during the 2 years of the study. However, the inclusion of all patients assessed for thyroid nodule disease at our clinic minimized the risk of any selection bias. Some of our results were only obtained from patients undergoing surgery, and should therefore be interpreted with caution before they are applied to the general population of patients with thyroid nodules. It should be noted that only patients undergoing thyroidectomy were considered in assessing the sensitivity and specificity of diagnostic tests. In addition, in most studies patients with negative cytological results do not necessarily undergo surgery, and are often not considered for statistical analysis. This may represent a bias in the sensitivity of cytology. In our study, the inclusion of only a patient subgroup with negative cytological results (those with a large nodule or thyroid size and those with a personal preference for surgery) may have increased and decreased respectively the sensitivity and specificity of cytology for thyroid cancer detection.
Based on the clinical results achieved (superimposable to those reported in most medical series) and on the improvement seen in clinical care, implementation of a thyroid nodule high-resolution clinical is a highly recommended option for improving the care of patients with thyroid nodules.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Sebastián-Ochoa N, et al. Experiencia clínica en una consulta de alta resolución de nódulo tiroideo. Endocrinol Nutr. 2011;58:409–15.