Iodine nutritional status in pregnant women is important for neuronal development of the fetus, and may vary depending on the geographic area. Thyroid function and urinary iodine excretion were therefore assessed in pregnant women from three different provinces of a large Spanish autonomous community.
Patients and methodsA descriptive study was conducted in the three healthcare areas of Burgos, Avila, and Ponferrada on 1200 women in the first trimester of pregnancy The study consisted of a survey and thyroid hormone and urinary iodine measurements.
ResultsUse of iodized salt and iodine-containing pharmacological compounds was reported by 40% and 17% of pregnant women respectively. Median urinary iodine excretion in the total group was 121mcg/L, with lower values in Burgos (117mcg/L) and Ponferrada (118mcg/L) and higher levels in Avila (130mcg/L). Urinary iodine excretion was less than 100mcg/L in 34% of women and was undetectable in 3.3%. Excretion levels lower than 150mcg/L were found in 69.8% of women. Low thyroxine levels were detected in 1.1%, and thyrotropin levels were increased in 4.7%.
ConclusionsIodine deficiency currently exists in pregnant women from different areas of our large autonomous community. Consumption of iodized salt and iodine-containing pharmacological compounds is not widely established. It would be of great interest to conduct studies in other geographic areas and to advise an increased iodine intake in women who plan to become pregnant and in pregnant women from the very start of pregnancy.
El estado nutricional de yodo de las embarazadas es importante para el desarrollo neuronal del feto. Esta situación puede ser distinta según la zona geográfica estudiada, por lo que hemos valorado la función tiroidea y la excreción de yodo urinario en gestantes de tres provincias diferentes de una extensa comunidad autónoma.
Pacientes y métodoEstudio descriptivo, llevado a cabo en tres áreas sanitarias de Burgos, zona urbana, Ávila, zona rural y Ponferrada, zona rural valorada previamente. Se estudiaron 1.200 mujeres en el primer trimestre de la gestación, se realizo encuesta, se midieron hormonas tiroideas y contenido de yodo en orina.
ResultadosDeclararon consumir sal yodada el 40% de las embarazadas y compuestos yodados el 17%. La mediana de yoduria del grupo total fue de 121 mcg/L, con concentraciones más bajas de yodo en orina en Burgos (117 mcg/L) y Ponferrada (118 mcg/L) y mejores en Ávila (130 mcg/L). La yoduria fue inferior a 100 mcg/L en el 34% de las gestantes y presentaron niveles indetectables el 3,3%. El 69,8% de las mujeres presentaron yodurias menores de 150 mcg/L. Se constató hipotiroxinemia en un 1,1% de las gestantes y la tirotropina se encontró aumentada en un 4,7%.
ConclusionesEn la actualidad existe déficit de yodo en las embarazadas de diferentes zonas de nuestra amplia comunidad autónoma. El consumo de sal yodada y de compuestos farmacológicos de yodo no está ampliamente establecido. Es necesario suplementar el consumo de yodo en las mujeres que programen embarazo y lo antes posible en las que ya se encuentran embarazadas una vez conocida la gestación. Sería conveniente llevar a cabo estudios de otras áreas no valoradas.
It is well known that iodine nutritional status is important in pregnant women for the neurological development of the fetus and that iodine requirements increase during this time of life.1,2 Even a mild iodine deficiency has been related to neurocognitive changes in infants3,4. International organizations such as the OMS and UNICEF have devoted their efforts for decades to achieving adequate iodine intake in pregnant women.5,6 Several national epidemiological studies have shown that iodine deficiency continues to exist in pregnant women from different Spanish regions,7–9 and various scientific societies have been working for years to eradicate this situation.10
In 1992, significant iodine deficiency was found in schoolchildren from the Bierzo area in the province of Leon,11,12 but no subsequent studies conducted on this type of population are available.
Subsequently, the study on pregnant women in the same area published by us in 2002 showed a significant iodine deficiency,9 which was also reported in 2009 in another area of the community.13
The objective of this study, supported by the Directorate General of Public Health of Castile and Leon, was to assess iodine nutritional status in women in early pregnancy. To assess maternal thyroid function and hormone supply to the fetus, plasma thyroxine and thyrotropin levels and urinary iodine excretion were measured in women in their first trimester of pregnancy from three geographical areas previously selected by technicians and epidemiologists from the regional government: Avila, Burgos, and Ponferrada (Bierzo area). These were selected as representative of a rural population (Avila), an urban population of the tableland area (Burgos), and a peripheral area with a traditional risk of goiter (Ponferrada). Urinary iodine levels were measured in a group of newborns from Ponferrada as an indicator of infant status at birth.
Patients and methodsA descriptive, prospective study: Study design and strategy was devised by us in collaboration with the Health Promotion Service and with technicians from the Directorate General of Public Health of the Castile and Leon regional government, with the contribution of the Directorate General of Health Care. This study was approved by the relevant ethics committee.
Inclusion criteria and protocol: A total of 1200 women in the first trimester of pregnancy, 400 from each area, were recruited upon attendance to the health center. Midwives administered the survey, recording pregnancy week and the use of iodized salt and/or potassium iodide supplements, including the name of the preparation. Iodide contents ranged from 75 to 200mcg/g. Time of intake of the preparation was not recorded. After obtaining informed consent, thyrotropin and thyroxine measurements were included in laboratory tests of pregnant women. Urine samples frozen at −20°C were stored and subsequently sent to Hospital El Bierzo by services from each area, together with the surveys and the results of thyroid laboratory tests.
FT4 and TSH levels were measured at the reference hospital of each area.
A total of 1125 surveys were considered to be valid, 411 from women in Burgos, 403 from women in Avila, and 311 from women in Ponferrada. These were collected between weeks 2 and 14 of pregnancy. Mean age was 31 years, with a range from 15 to 44 years and a standard deviation of 5.17 years.
Exclusion criteria: Thirteen women with known prior thyroid disease or who were taking thyroid hormone were excluded from the study.
Laboratory methods: In Burgos, laboratory tests were performed by electrochemiluminescence immunoassay using an Elecsys Modular Analytics E170 analyzer (Roche Diagnostics GmbH, Mannheim, Germany). TSH measurement limits ranged from 0.005 to 100mIU/mL, with a coefficient of variation of 3.2–7.2% for the different TSH values. The laboratory reference interval for the general population was 0.3–5.0mIU/L. FT4 measurement limits ranged from 0.023 to 7.77ng/dL, with a coefficient of variation of 2.6–4.8%. The corresponding laboratory reference interval for the general population was 0.9–1.7ng/dL.
In Avila, laboratory measurements were performed by chemiluminescence immunoassay using an Advia Centaur analyzer (Siemens Healthcare Diagnostics Inc., Tarrytown, USA). TSH measurement limits ranged from 0.008 to 150mIU/mL, with a coefficient of variation of 3.6–6.6% for the different TSH values. The laboratory reference interval for the general population was 0.47–6.0mIU/L. FT4 measurement limits ranged from 0.1 to 12.0ng/dL, with a coefficient of variation of 3.4–4.2%. The corresponding laboratory reference interval for the general population was 0.7–2.0ng/dL.
In Ponferrada, TSH and FT4 levels were measured using the same method and analyzer as in the Avila hospital. The corresponding laboratory reference values in the general population were 0.35–5.5mIU/L for TSH and 0.85–1.74ng/dL for FT4. Peroxidase antibodies were measured, as TSH and FT4, at the laboratory of Hospital El Bierzo using the Anti-TPO ORG503 enzyme immunoassay (Orgentec Diagnostics GmbH, Mainz, Germany). This assay was calibrated against the reference preparation MRC 66/387 of the World Health Organization. Its measurement limits were 0–3000IU/mL, values higher than 75IU/mL were considered positive, and the coefficient of variation ranged from 1.5% to 9.7% for the different antibody values. Total T4 and TBG measurements were performed at the reference laboratory. Total T4 was measured by a chemiluminescence immunoassay using an Advia Centaur analyzer (Siemens) with a coefficient of variation of 7.6–12.3% and a reference range of 4.5–12.5mcg/dL. TBG T4 was measured by a chemiluminescence immunoassay using an Immulite 2000 analyzer (Siemens) with a coefficient of variation of 8.0–12.4% and a reference range of 13–39mcg/dL.
Urinary iodine levels were measured at the clinical laboratory of Hospital El Bierzo using the Benotti and Benotti method,14 including the classical Sandell–Kolthoff reaction15 for iodine measurement in urine. This method has a detection limit of 20mcg/L and a dilution limit of 150mcg/L. The coefficient of variation ranges from 3.5% to 6% for the different iodine levels. Iodine/creatinine ratio was calculated in all samples. To ensure reliability of results, in addition to applying internal quality controls, the laboratory participated in the external quality control for urinary iodine of the Spanish Neonatal Screening Society.
Statistical analysis: Microsoft Office Excel 2009 software was used for databases and calculations, and SPSS 14.0 software was subsequently used for descriptive statistics. Normality of distribution was calculated using a Kolmogorov–Smirnov test, and a Mann–Whitney U-test was used to compare means. Variable correlation was performed using Pearson's correlation coefficient.
ResultsA total of 411 women were surveyed in Burgos. Of these, 192 (47%) reported the use of iodized salt, and 63 (15%) were taking potassium iodide supplements.
FT4 levels were available for 251 women. Mean FT4 levels were 1.11±0.44ng/dL. Only 3 women (1.2%) had values below the normal laboratory limit.
TSH levels were available for 254 pregnant women. Mean TSH levels were 2.22±1.63mIU/L. Sixteen women (4.8%) had TSH values higher than 5mIU/L (the upper reference laboratory value). The recommended TSH levels for the first trimester of pregnancy are 2.5mIU/L,16–18 and higher values were found in 82 pregnant women (33%).
TSH levels less than 0.4mIU/mL were reported in 15 women, but only one of these had FT4 levels above the normal limit and could be considered to have hyperthyroidism.
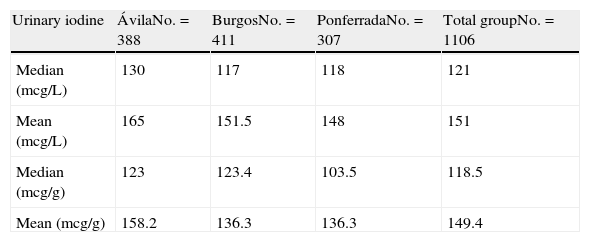
A total of 411 valid urine samples were received. Median and mean urinary iodine levels were 117mcg/L and 151.5mcg/L respectively. When iodine was expressed as mcg/g of creatinine, median and mean levels were 123.4mcg/g and 136.3mcg/g respectively (Table 1).
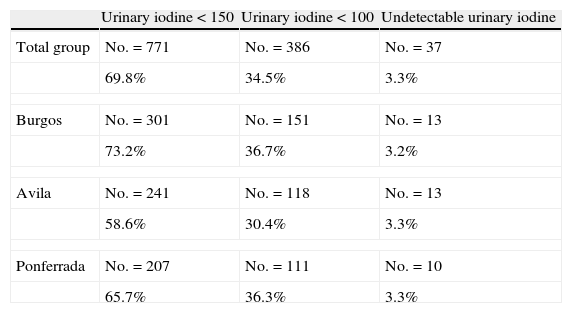
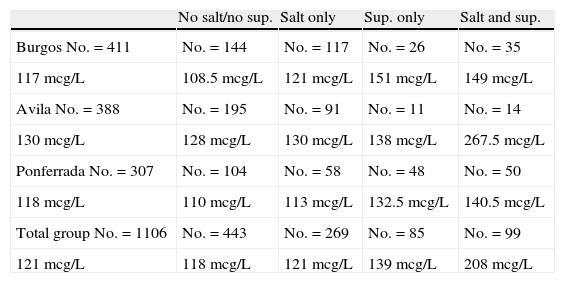
Three hundred and one women (73.2%) had urinary iodine levels lower than 150mcg/L, and 151 women (36.74%) had values lower than 100mcg/L (Table 2). The best urinary iodine levels were found in pregnant women who were taking iodide-containing supplements: 151mcg/L (Table 3).
Urinary iodine levels lower than recommended.
| Urinary iodine<150 | Urinary iodine<100 | Undetectable urinary iodine | |
| Total group | No.=771 | No.=386 | No.=37 |
| 69.8% | 34.5% | 3.3% | |
| Burgos | No.=301 | No.=151 | No.=13 |
| 73.2% | 36.7% | 3.2% | |
| Avila | No.=241 | No.=118 | No.=13 |
| 58.6% | 30.4% | 3.3% | |
| Ponferrada | No.=207 | No.=111 | No.=10 |
| 65.7% | 36.3% | 3.3% | |
Median urinary iodine levels depending on iodide intake by area and overall.
| No salt/no sup. | Salt only | Sup. only | Salt and sup. | |
| Burgos No.=411 | No.=144 | No.=117 | No.=26 | No.=35 |
| 117mcg/L | 108.5mcg/L | 121mcg/L | 151mcg/L | 149mcg/L |
| Avila No.=388 | No.=195 | No.=91 | No.=11 | No.=14 |
| 130mcg/L | 128mcg/L | 130mcg/L | 138mcg/L | 267.5mcg/L |
| Ponferrada No.=307 | No.=104 | No.=58 | No.=48 | No.=50 |
| 118mcg/L | 110mcg/L | 113mcg/L | 132.5mcg/L | 140.5mcg/L |
| Total group No.=1106 | No.=443 | No.=269 | No.=85 | No.=99 |
| 121mcg/L | 118mcg/L | 121mcg/L | 139mcg/L | 208mcg/L |
Full-size table.
Sup.: supplement.
A total of 403 women were surveyed in Avila, of whom 133 (34%) used iodized salt and 27 (7%) took potassium iodide supplements.
FT4 results were available for 341 women. Mean FT4 levels were 1.19ng/dL. Only 2 women (0.6%) were below the laboratory reference limit.
Mean TSH levels were 2.91mIU/L (in 343 valid samples). TSH values higher than 6mIU/L (the upper laboratory reference limit) were found in 14 (4%) pregnant women, while 138 women (40%) had TSH levels higher than 2.5mIU/L.
TSH levels less than 0.4mIU/mL were reported in 10 women, 3 of whom also had FT4 levels above the normal limit and could be considered to have hyperthyroidism.
A total of 388 valid urine samples were received. Median and mean urinary iodine levels were 130mcg/L and 165mcg/L respectively. When urinary iodine was expressed as mcg/g of creatinine, median and mean levels were 123mcg/g and 158.2mcg/g respectively (Table 1).
Urinary iodine levels lower than 150mcg/L were reported in 241 women (58.6%), and 118 women (30.42%) had values lower than 100mcg/L (Table 2).
As regards median urinary iodine levels depending on whether or not supplements and/or iodized salt were taken, the highest medians (267.5mcg/L) were found in pregnant women who took both salt and supplements (Table 3).
A total of 311 women were surveyed in Ponferrada. Of these, 118 women (38%) used iodized salt and 104 (34%) took potassium iodide supplements.
FT4 results were available for 305 women. Mean FT4 levels were 1.13ng/dl/dL. Only 5 women (1.63%) were below the laboratory normal limit.
Mean TSH levels were 2.18mIU/L, and valid results were available for 305 women. TSH values higher than 5.5mIU/L (the upper laboratory reference limit) were found in 11 pregnant women (3.57%), and 88 women (29%) had levels higher than 2.5mIU/L.
TSH levels less than 0.4mIU/mL were reported in 15 women, but only one of these had FT4 levels above the normal limit and could be considered to have hyperthyroidism.
Mean total T4 levels were 8.6±2.1mcg/dL (normal range, 4.5–12.5mcg/dL). Mean TBG levels were 27.2mcg/mL (normal range, 13–39mcg/mL). The TT4/TBG ratio was 3.4 (normal, 2.3–6.2).
Valid urine samples were received from 307 pregnant women. Median and mean urinary iodine levels were 118mcg/L and 148mcg/L respectively. When iodine was expressed as mcg/g of creatinine, median and mean levels were 103.5mcg/g and 136.3mcg/g respectively (Table 1).
Urinary iodine levels lower than 150mcg/L were reported in 207 women (65.7%), and 111 women (36.27%) had values lower than 100mcg/L (Table 2).
As regards median urinary iodine levels depending on whether or not supplements and/or iodized salt were taken, the highest medians (140.5mcg/L) were found in pregnant women who took both iodized salt and supplements (Table 3).
Peroxidase antibodies were measured in 108 women and were positive in 15 of them (13.9%). A statistical correlation was found with the highest TSH levels (p=0.01), but not with FT4.
Since the technique was available, urinary iodine levels were measured in 64 newborns. Mean levels found were 122mcg/L.
Overall, data from 1125 women in the first trimester of pregnancy were received. Forty percent of these (443 women) stated that they used iodized salt. Supplements containing potassium iodide were taken by 194 pregnant women (17%), and iodized salt by 103 women (9%).
FT4 results were received by 901 women. Median FT4 levels were 1.15ng/dL. Ten women (1%) were below the lower limit for each laboratory.
Median TSH levels were 1.8mIU/L (in 902 valid samples). TSH levels above the upper laboratory limit were found in 43 pregnant women (4.75%). Hyperthyroidism, with high FT4 levels and TSH levels lower than 0.4mIU/L, was detected in 5 women (0.55%). TSH levels were higher than 2.5mIU/L in 308 pregnant women (35%).
A total of 1106 valid samples were received for urinary iodine measurement. Median and mean urinary iodine levels were 121mcg/L and 151mcg/L respectively. When iodine was expressed as mcg/g of creatinine, median and mean levels were 118.5mcg/g and 149.4mcg/g respectively (Table 1). Differences in mean urinary iodine levels between provinces did not reach statistical significance.
Urinary iodine levels lower than 150mcg/L were reported in 771 women (69.8%), 37 women (3.3%) had undetectable levels, and 386 women (34.5%) had values of 100mcg/L or less (Table 2).
Better urinary iodine levels (median value, 208mcg/L) were found in pregnant women who reported the use of both iodized salt and potassium iodide as compared to those who only took iodized salt (median value, 121mcg/L) or supplements (median value, 139mcg/L). Urinary iodine levels were undetectable in 3.3% of pregnant women, with no differences between the three provinces studied: 13 women in both Burgos and Avila and 10 women in Ponferrada (Table 3).
DiscussionThe significance of iodine nutritional status in pregnant women is widely recognized today. In the Castile and Leon autonomous region, the largest in Spain, such status had only been assessed in two limited areas,9,13 and is now assessed in areas of the north tableland of Spain (the provinces of Avila, Burgos, and Leon) where it had not previously been studied. Currently ongoing studies are showing an improved iodination of the population.
In our study, women who took no iodized salt or iodine supplements had median urinary iodine levels higher than 100mcg/L. Median urinary iodine levels recommended in pregnant women ranged from 150 to 230mcg/L, and from 180 to 220mcg/g when expressed as mcg/g of creatinine.19 Median levels in the overall group of pregnant women were lower than recommended when expressed both as micrograms per liter, 121mcg/L, and as iodine contents per gram of creatinine, 118.5mcg/L. Since iodine bioavailability is estimated at 92%,21 it may be estimated that the iodine intake of these women was approximately 129mg/day, lower than recommended. Seventy percent of all pregnant women had urinary iodine levels lower than 150mcg/L. It should be noted that one third of the pregnant women in this study (36%) had urinary iodine values of 100mcg/L or less.
In a 2009 study conducted on pregnant women from the healthcare area of Palencia, in the same autonomous region, and during the same pregnancy period, women had lower median urinary iodine levels as compared to this study, 113.7mcg/L.13 Other studies conducted in the same population group in different autonomous regions reported similar findings.7,8,22,23
No differences were found in median urinary iodine levels between women from Burgos, an urban area, and those from Ponferrada, considered as a iodine-deficient rural area (117mcg/L versus 118mcg/L), because the latter took more pharmacological supplements, probably because of a greater awareness by healthcare professionals based on prior studies in the same area. On the other hand, pregnant women from Avila, considered a rural area by epidemiologists from the Castile and Leon government, although deficient in iodine (but with a non-statistically significant difference), showed a better nutritional iodine status (130mcg/mL) (Table 1) and reported the lowest intake of potassium iodide supplements (267.5mcg/L). This leads us to wonder whether iodide supplementation in women already using iodized salt is needed in this area. There should be other sources of the trace element accounting for the difference. It is therefore necessary to assess different Spanish geographic areas, even within the same autonomous region.
An improved nutritional iodine status was found in pregnant women from the Bierzo area. While a study published by us in 20029 reported mean urinary iodine levels of 71.4mcg/L in the first trimester of pregnancy, current mean levels in women from the same area were 148mcg/L because 34% of women were already taking iodine supplements upon entry into the current study, while in 2002 their use was recommended from the first trimester of pregnancy, once women had attended the endocrinology department.
Improved FT4 levels were also found in pregnant women from Ponferrada. Thus, only 1.63% of them had low FT4 levels in our study, as compared to 9.5% in 2002.
TSH levels in the first trimester of pregnancy and in non-pregnant women are interpreted differently.20 Thirty-five women had low TSH levels with normal FT4 levels, attributable to the effect of beta-HCG during this period of pregnancy. Increased TSH levels were found in 4.7% of the overall group, if maximum values less than 4mIU/L are considered adequate.17 Since the recommended TSH levels in the first trimester of pregnancy are 2.5mIU/L,16–18 308 pregnant women (35%) were above such values.
Antithyroid antibody levels were measured in a sample of women from Ponferrada, with a positivity rate similar to that of other studies published in Spain.7 Antibody tests were positive in 14% of the women in our study, as compared to 8% in the 2002 study. By contrast, elevated TSH levels were less common in this study (3.7%) than in the 2002 study (8.2%) according to values calculated based on the upper normal limit for the general population, which were the values used in 2002.
Median urinary iodine levels in newborns were within the recommended value of 122mcg/L (recommended, 90mcg/L), but were not measured in mothers at the end of pregnancy. It may therefore be assumed that nutritional iodine status would have improved from the first trimester, when sampling was performed, to the end of pregnancy, since iodine supplements were recommended from the first visit to women who were not taking them.
We therefore conclude that iodine deficiency exists in pregnant women from a large population of the Castile and Leon autonomous region and that differences exist between the different geographic areas studied. More intense health information campaigns are needed to recommend to healthcare professionals and other people concerned the use of iodized salt by all and potassium iodide supplementation when requirements are increased, as occurs during pregnancy. The separate assessment of different geographic areas is indispensable, because differences between rural and urban areas can be found even within the same autonomous region.
FundingStudy supported by the Directorate General of Public Health of the Castile and Leon government.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: González Mateo MC, et al. Valoración del estado de nutrición yódica y niveles de tiroxinemia en mujeres embarazadas de diferentes áreas geográficas de Castilla y León. Endocrinol Nutr. 2011;58:416–21.