Systemic sclerosis (SS) is a multisystemic autoimmune disease of connective tissue that causes vascular damage and fibrosis. The incidence of thyroid dysfunction is significantly higher in patients with SS as compared to the general population,1 and thyroid gland fibrosis has been reported in up to 14% of patients in autopsy studies.2 However, only two cases of hypoparathyroidism (HP) have been reported to date in patients with SS,3,4 and the two diseases were simultaneously diagnosed in both. An autopsy of the first patient showed fibrosis of all four parathyroid glands,3 while computed tomography (CT) of the brain of the second patient disclosed bilateral, symmetrical calcifications in the basal ganglia and cerebellum,4 a condition also known as Fahr's disease (FD), whose association with HP was first reported by Eaton et al. in 1939.5
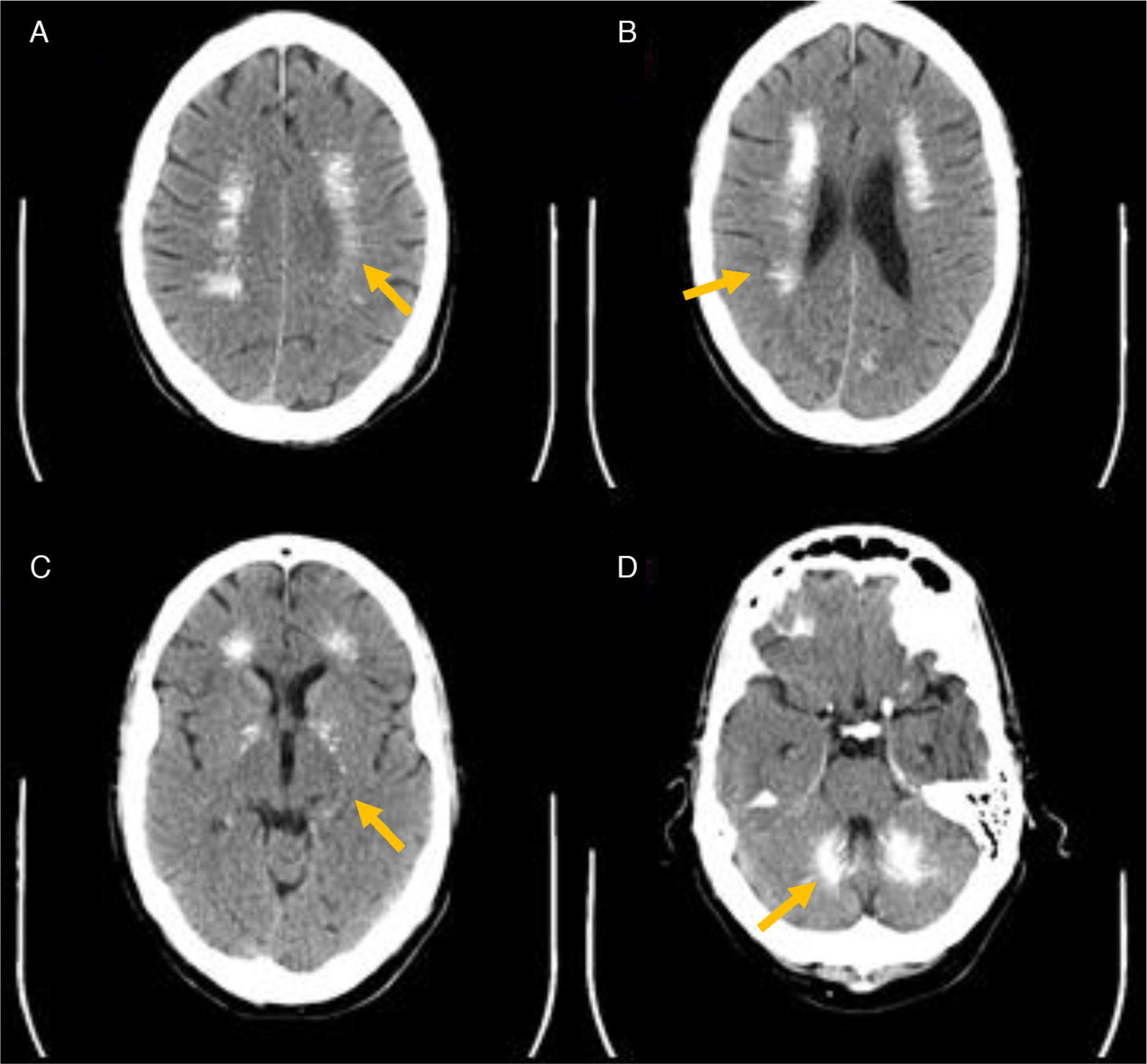
We report here the case of a 57-year-old male patient diagnosed 17 years before with HP and SS with cutaneous, esophageal, and pulmonary involvement for which he was receiving treatment, who attended the emergency room for paresthesia, tremor, coldness and cramps in all four limbs, associated with memory loss and behavioral changes over the previous year. The patient's history included high blood pressure (HBP), chronic obstructive pulmonary disease (COPD), superficial gastritis, macrocytic anemia, calcific tendinopathy, and subcapsular cataract. Current treatment consisted of methotrexate 5mg: 1comp/8h (Wednesday and Thursday), prednisone 7.5mg: 1comp/day, nifedipine retard 20mg: 1comp/day, acfol 1comp weekly, Ideos-20 vitamin D 1comp/8h, magnesium 1comp/8h. A physical examination showed, in addition to tremor and coldness, sclerodactily and cyanosis in all four limbs, associated with bradypsychia and depressive mood. Laboratory test results included: total calcium 6.6mg/dL (8.4–10.2); ionic calcium 0.85mmol/L (1.12–1.32), phosphate 5.6mg/dL (2.7–4.5), magnesium 1.62mg/dL (1.80–2.60), C-reactive protein (CRP) 22.2mg/L (0–5), PTH <3pg/mL (12–65), (25(OH)) vitamin D 51ng/mL (30–100), TSH 2.02, and T4 1.01. CT of the head revealed multiple bilateral, symmetrical intracerebral calcifications (Fig. 1). Six days after the start of treatment with calcium (oral and intravenous), magnesium, and 25-OH vitamin D, biochemical normalization and symptomatic improvement were achieved. A neurological study, including an examination of cerebrospinal fluid, allowed for a diagnosis of cortical-subcortical mild to moderate dementia. Alzheimer's disease, demyelinating diseases, and tuberculosis were ruled out. Three cerebral aneurysms were incidentally found. After hospital discharge, low thyroxine levels were detected (TSH 2.60, T4 0.80), and a neck ultrasound examination showed a slight increase in thyroid size (an AP diameter of 18mm) with no evidence of focal lesions or parathyroid glands. Treatment was started with levothyroxine sodium 50μg daily. An immunological study ruled out the presence of peroxidase antibodies (<2.00IU/mL), thyroglobulin (<2.00IU/mL), and parathyroid antibodies (undetectable). Both the patient and his family stated that they were unaware of the importance of adequate compliance with calcium and 25-OH vitamin D treatment, and reported intolerance to the various preparations prescribed, with frequent treatment noncompliance.
FD was initially described by Delacour en 1850.6 FD is usually due to phosphorus and calcium metabolism disorders, occurring in up to 73–78% of patients with idiopathic HP,7 but may also be induced by other metabolic, infectious, or genetic causes (such as diabetes mellitus, AIDS or osteopetrosis). Today, the term “Fahr's syndrome” tends to be used for congenital forms of the disease only. The differential expression of various osteogenic molecules in the caudate nucleus and gray matter of the brain appears to account for the preferential location of intracerebral calcifications in these areas.8 Their occurrence correlates to the duration of hypocalcemia and the presence of choroid plexus calcification, seizures, and cataract, and progression depends on the serum calcium/phosphorus ratio during follow-up.9 The reported patient had, in addition to subcapsular cataract, a long-standing history (17 years) of HP, and probably also of hypocalcemia because of erratic treatment compliance (with a low calcium/phosphorus ratio).
On the other hand, neuropsychological impairment occurs in up to one third of patients with HP, and has been correlated to the duration of symptoms of hypocalcemia, serum calcium levels, and the serum calcium/phosphorus ratio.10 In elderly patients, it also appears to be associated with the volume, number, and location of calcifications through its impact on blood flow and synaptic transmission. In our patient, FD due to long-standing HP was considered to be the most probable cause of cognitive impairment, as well as chronic hypocalcemia due to treatment noncompliance. However, the degree of dementia appeared to be more severe than would normally be expected for classical FD, and the extensive calcification found in the patient was also striking, as he had a greater number and volume of intracerebral calcifications than usually reported in FD and than a patient previously reported with SS, HP, and FD.4 It should be noted that neurocognitive impairment may affect activities of daily living, promoting drug noncompliance, as suspected in our patient.
The detection of HP at 41 years of age and in parallel with SS diagnosis, the absence of prior surgery or radiation therapy in the neck area, and the findings of the immunological study suggest, by exclusion, a possible infiltrative origin of HP in this patient. Since SS may induce parathyroid gland fibrosis and HP,3 the prevalence of subclinical parathyroid changes in patients with SS is probably higher than that found to date. It is therefore advisable to increase the index of suspicion and to perform regular monitoring of phosphorus and calcium metabolism in patients with SS, especially in those with cognitive impairment, behavioral changes, or cerebral calcifications. Once HP is diagnosed, it is essential to inform both patients and their families about the importance of good treatment compliance and the potential risks of inadequate medication intake. Noncompliance may be both the cause and the consequence of cognitive impairment associated with HP,10 as it promotes the occurrence and progression of FD through a long-term maintenance of hypocalcemia and a low calcium/phosphorus ratio.9
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Moreno Ó, García PT, Sánchez D, Sancho T, Lecumberri B. Hipocalcemia severa y deterioro cognitivo en paciente con hipoparatiroidismo y esclerosis sistémica. A propósito de un caso. Endocrinol Nutr. 2015;62:356–358.