Epidemiology of acromegaly in Spain does not differ from that reported in other published series. Prevalence rate is approximately 60 cases per million, peak incidence occurs in middle age, more women are affected (61%), and there is a substantial delay between occurrence of the first symptoms and diagnosis. Studies REA (Spanish Acromegaly Registry) and OASIS analyzed the epidemiology, clinical characteristics, and management of the disease in Spain. Surgery, performed in more than 80% of patients, has been (and continues to be) the main treatment for the past four decades. In the past decade, however, more patients have received somatostatin analogs (SSAs) as first-line treatment. Use of radiation therapy has significantly decreased in recent decades. Somatostatin analogs (SSAs) are the most commonly used drugs, administered to 85% of patients; however, only 12–15% continue on drug treatment alone. The surgical remission rate was 38.4% in the last decade, with a significant improvement over decades. Preoperative treatment with SSAs has no influence on surgical cure rates. Second-line therapies used after surgical failure in the past decade included SSAs in 49% of patients, repeat surgery in 27%, radiotherapy in 11%, pegvisomant in 15%, and dopamine agonists in 5%. Mean cost of acromegaly treatment was 9668€ (data estimated in 2009 and adjusted in 2010), of which 71% was due to the cost of SSAs. Patients treated with pegvisomant have a more aggressive form of the disease and higher comorbidity rates.
La epidemiología de la acromegalia en España no difiere de la de otras series publicadas. La prevalencia es de alrededor de 60 casos por millón, el máximo de diagnósticos ocurre en la edad media de la vida, hay predominio de mujeres (61%) y se objetiva un gran retraso entre la aparición de los primeros síntomas y el diagnóstico. Los estudios del registro español de acromegalia (REA) y OASIS han analizado la epidemiología, las características clínicas y el tratamiento de la acromegalia en España. El tratamiento principal ha sido y sigue siendo la cirugía (en más del 80% de los pacientes), aunque en la última década más pacientes han recibido terapia médica como primera línea de tratamiento. En las últimas décadas se ha observado una disminución significativa en las tasas de radioterapia. Los análogos de la somatostatina (SSA) son los fármacos más utilizados. Alrededor del 85% de los pacientes reciben terapia con SSA, aunque solo un 12–15% persisten con tratamiento médico como terapia exclusiva. La curación quirúrgica es pobre, alcanzando el 38,4% en la última década según el REA sin influencia del tratamiento con SSA previo. En la última década la segunda línea de tratamiento tras el fracaso quirúrgico fue los SSA en un 49%, la reintervención en un 27%, la radioterapia en un 11%, Pegvisomant en el 15% y agonistas dopaminérgicos en el 5%. El coste medio del tratamiento de la acromegalia es de 9668€ (datos estimados en 2009 y ajustados en 2010) y un 71% corresponde al coste de los SSA. Los pacientes que reciben Pegvisomant presentan una acromegalia más agresiva con mayor tasa de comorbilidades.
Acromegaly is a disease resulting from excess production of growth hormone (GH) by the pituitary gland, caused in the vast majority of cases by a GH-secreting adenoma and in a few cases by ectopic GHRH secretion. The following review is intended to summarize the most important epidemiological data about acromegaly in Spain as regards both its incidence and prevalence and its treatment and cure.
Epidemiology: incidence, prevalence, sex, and age at diagnosisThe first study on the prevalence of acromegaly in Spain was conducted in Biscay.1 Etxabe et al. recorded 72 patients with acromegaly diagnosed over 20 years in Biscay (from 1970 to 1989), an area with a population of 1,183,000 inhabitants at that time. The incidence was 3.1 cases per million inhabitants, per year, and an increase was seen over the years from 1 to 5.6 cases per million inhabitants, per year. The prevalence was 60 cases per million of the population. The condition predominated in females as compared to males (64% and 36% respectively), and age at diagnosis was 44.2±17 years. Two thirds of the patients were diagnosed between the fourth and sixth decades of life. An estimated time between symptoms and diagnosis ranging from 0.5 to 35 years was also found. Only 50% of patients reported symptoms for less than nine years.
Mestrón et al. reported data on a higher number of patients (n=1219) included in the Spanish acromegaly registry (Registro Español de Acromegalia, REA).2 The first objective of the REA was to collect epidemiological data about acromegaly in Spain. For this, researchers were asked to systematically record all cases diagnosed at their centers, although participation in the study was voluntary and case registration depended on the participating physicians. The REA was started in 1997, when a greater incidence of the disease was seen. Its incidence subsequently decreased. An incidence rate of 2.1 cases per million of the population, per year was estimated in 1997, with great differences between the autonomous communities. Some autonomous communities such as Asturias, Aragón, and La Rioja, with a population of 2.5 million, reported no cases. Excluding these regions, the prevalence of acromegaly was estimated at 36 cases per million inhabitants, ranging from 15.7 to 75.8 depending on the autonomous community. The REA also showed that acromegaly was more common in females (60.8%) as compared to males (39.2%). Mean age at diagnosis was 45 years (SD=14), and estimated mean time with symptoms before diagnosis was five years.
In the recent 2010 analysis of the REA, 61% of the 1658 patients were women.3 Mean age at diagnosis was 45.5 years (interquartile range, 35–55), and the estimated time with symptoms before diagnosis was 6±6 years. A predominance in women has been shown in all Spanish studies (Etxabe et al.,1 OASIS,4 and REA2,3), and also in most European registries, including the German (54% of women),5 French (55% of women)6 and Italian (59% of women) registries7; the Belgian registry is the only one to report similar proportions of men and women (51/49%).8 The mean age at diagnosis was similar in all of them.5–8
The prevalence reported by Etxabe et al. (60 cases per million population) was reliable for the specific geographical area of Biscay at the time of the study. The prevalence reported by Mestrón et al.1 (36 cases per million population) was probably an underestimation, not only due to undiagnosed cases, but also because not all the patients with acromegaly seen at the different hospitals were included. The prevalence of acromegaly in the different studies ranges from 36 to 151 cases per million.8–11 Cannavò et al. studied the prevalence of acromegaly in Messina (Sicily, Italy) and found a great difference between the different areas, classified on the basis of the environmental context and industrial density (from 26 to 210 cases per million).12 These authors hypothesized a potential environmental influence on the incidence of the disease. Schneider et al. used IGF-I levels to screen an unselected adult population attending several primary care centers (n=6773).11 The prevalence of acromegaly was 1034 cases per million of the population, much higher than the theoretical prevalence, which supports the concept that this is an underdiagnosed disease. Acromegaly is not only diagnosed late, but is overlooked in many cases. The predominance of the disease in females may be related to consultation for menstrual changes.
Treatment of acromegaly in SpainThe retrospective REA study,1,2 active for the past 14 years, allowed for the analysis of patients with acromegaly over four decades. The OASIS study,4 shorter and smaller, enrolled a cohort of 74 patients who were monitored for 28 months (recruited from 2005 to 2007) and mainly provided data about the clinical practice in patients treated in recent years.4
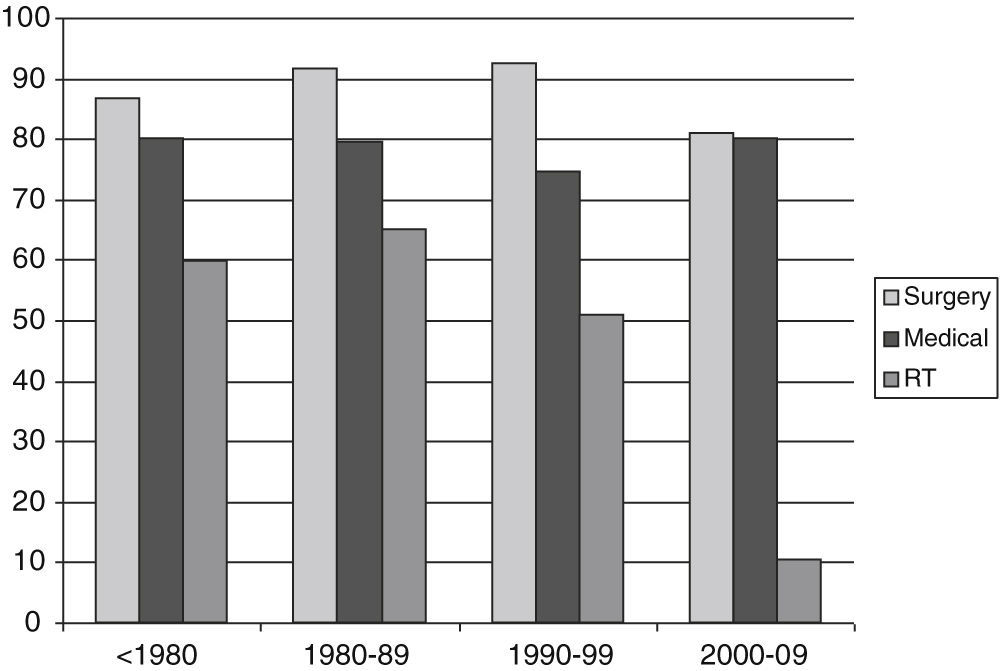
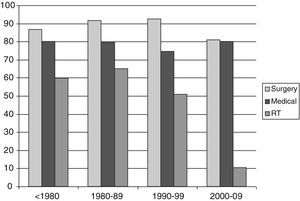
Analysis of the REA study enabled us to confirm that surgery has been and continues to be the main treatment for acromegaly. Eighty-four percent of patients underwent surgery, with sustained rates over the decades. Seventy-five percent of patients received medical treatment, which changed over time, with a decrease in the use of dopamine agonists and an increased used of somatostatin analogs (SSAs) over the decades.3 The REA study also reported decreased radiotherapy use over time. Overall, 36% of patients received radiotherapy: 62.8% of patients diagnosed before 1980, and 61.6%, 42.2%, and 11.9% of patients diagnosed in the subsequent three decades (p<0.001) (Fig. 1). The proportions of patients given medical treatment alone were 7.3%, 6%, 7.2%, and 15% respectively in the four decades analyzed.3
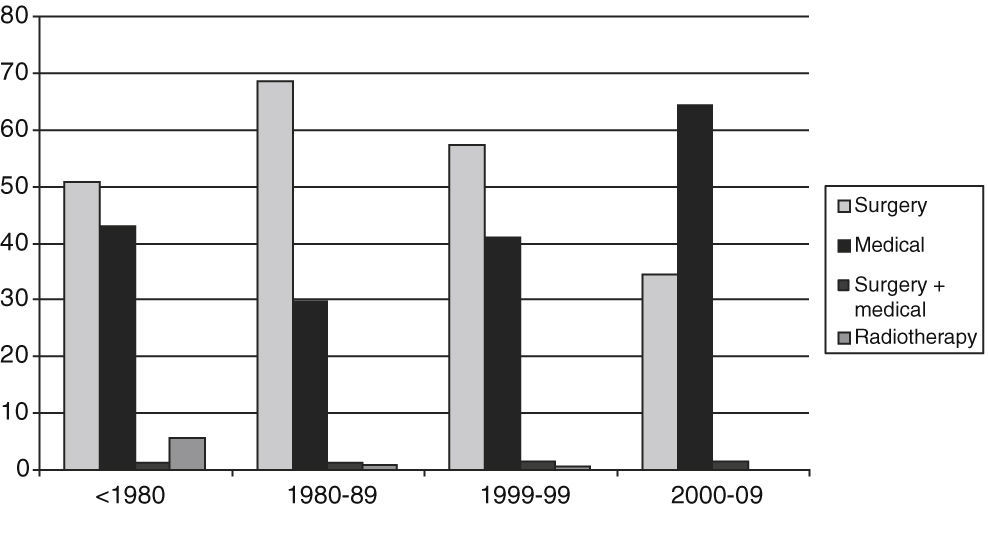
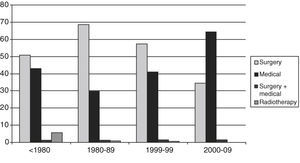
A significant change was also shown in the first treatment used to treat the disease; surgery was the first-line treatment until the most recent decade (2000–2009), when medical treatment was more commonly used first. Surgery was the first-line treatment in respectively 50%, 66.5%, 58.9%, and 38.5% of patients diagnosed over four decades, while medical treatment was first used in 42.4%, 31.3%, 39.2%, and 60.3% of cases, respectively.3 The positioning of medical treatment as the approach most commonly used in patients with acromegaly coincided with the availability of long-acting SSAs, available since 1997. First-line radiotherapy was only marginally used in patients diagnosed in the first decades (Fig. 2).
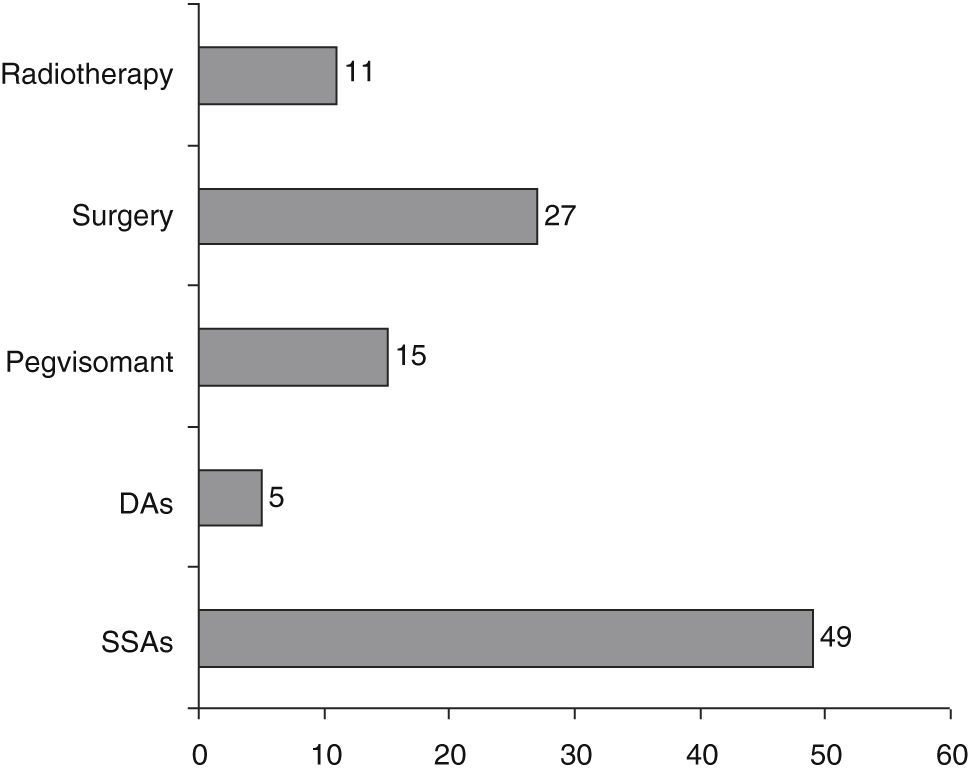
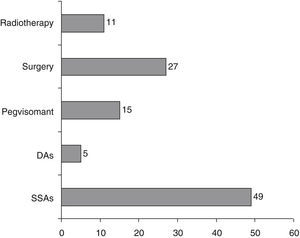
Results from the OASIS study4 agree with those from the REA study for patients diagnosed in the same decade. Overall, 76% of patients underwent surgery in the first six months from diagnosis. Of these, 36% had been pretreated with SSAs. Twenty-four percent received SSAs as first-line treatment (treatment with analogs for longer than six months), although 50% of them subsequently required surgery for poor control. Thus, 60% of patients received medical treatment with SSAs as initial therapy and only 12% of patients continued on primary medical treatment at the end of the 28 months of follow-up. The OASIS study clearly defined the second-line treatments after the failure of surgery: 49% of patients were treated with SSAs, 27% underwent repeat surgery, 11% received radiotherapy, and of the remaining patients, 15% were given pegvisomant and 5% dopamine agonists (Fig. 3).
Second-line treatments in the OASIS study after surgery (%). DAs: dopamine agonists; SSAs: somatostatin analogs. Data from Luque-Ramírez et al.4.
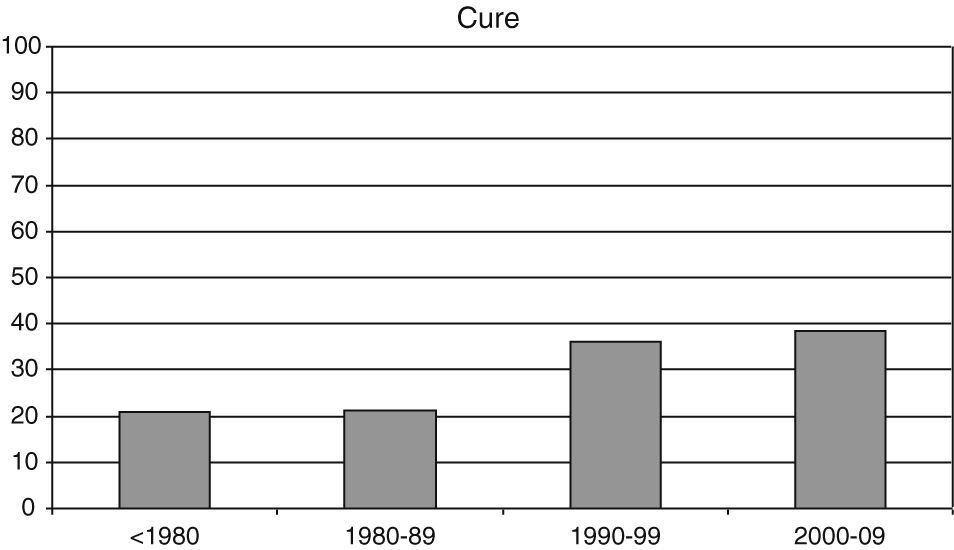
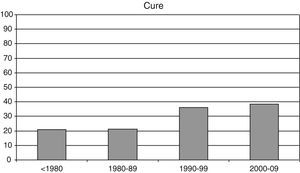
In the OASIS study, 27% of patients had postoperative cure criteria (GH less than 1 mcg/L after an oral glucose tolerance test), which were found in a significantly greater proportion of patients with microadenoma (71%) as compared to those with macroadenoma (15%). In the REA study, among the 698 patients evaluable in the last statistical analysis, the overall surgical cure rate, defined as normal IGF-I levels after surgery without the need for concomitant medical treatment, was 32%, with a significant increase over the decades: 20.8%, 21.1%, 36.1%, and 38.4% before 1980 and in the subsequent three decades, respectively (Fig. 4).
Pre-treatment with SSAs did not influence the cure rate in either study. The effect of pre-treatment with SSAs on cure is controversial, and randomized studies reporting benefits and no effects are both available.13–16
The surgical cure rate in the REA study was low, far below the cure rates reported by individual surgeons and hospitals specializing in this treatment.17–20 Only data from the Belgian registry more or less agree with those from the Spanish registry, with an overall surgical cure rate of 34%.8 A 67% cure rate was reported in the German registry using as criterion normal IGF-I levels.5 Individual surgical series reported cure rates ranging from 50% to 80%, with higher rates found in microadenoma as compared to macroadenoma.17–20 Some more recent endoscopic series reported cure rates of up to 100% in microadenoma.21,22 For individual surgeons, the endoscopic procedure allows for a better approach to tumors with lateral extension, common in acromegaly, but the superiority of one procedure over the other has not been shown.
In the REA study, the factors associated with the prognosis of surgical cure included adenoma size (macroadenoma or microadenoma) and male sex.3 In the reported series, the factors influencing surgical cure were surgical experience, basal GH, and adenoma extension, and male sex in some series.17–21
Patients treated with pegvisomantPegvisomant, a GH receptor antagonist, was used to treat 9.5% of patients in the REA study.3 The study of these patients when compared to all others showed that patients treated with pegvisomant in the REA study had more aggressive acromegaly, with higher GH levels at diagnosis, greater tumor size, and a higher proportion of associated comorbidities.23
Costs of treatment for acromegalyThe OASIS study assessed the financial impact of treatment of a representative cohort of standard management in Spain between 2005 and 2009.4,24 In the 74 patients included in the analysis, the following was considered: first-line surgery, those who received treatment before six months of recruitment and first-line medical treatment, and those who underwent no surgery before six months. Seventy-six percent of patients underwent surgery before six months of diagnosis, and 85% at some time during the study (in the 28 months of follow-up). The mean annual cost per patient was 9668€, ranging from 9223€ in the surgery subgroup to 11,054€ in the medical treatment subgroup. Seventy-one percent of costs were from SSAs. The cost per patient undergoing surgery alone was 2501€ per year, as compared to 9745€ per patient treated with SSA alone. The annual cost in patients receiving combined treatment ranged from 10,886 to 12,364€. Only 27% of patients were cured with surgery, and the vast majority of the patients therefore required combined treatment, involving high annual costs.
ConclusionsThe epidemiology of acromegaly in Spain does not differ from that reported in other published series. Its revalence is approximately 60 cases per million of the population, most diagnoses are made in middle age, and there is a long delay from the occurrence of the first symptoms to diagnosis. Surgery (performed in 80% of patients) is the main treatment for acromegaly, but a higher number of patients have received medical therapy as first-line treatment in the last decade. Radiotherapy rates have also decreased in recent decades. SSAs are the most widely used drugs. Approximately 85% of patients are given SSAs, although only 12–15% receive medical therapy as the sole treatment. Surgical cure rates are low, reaching 38.4% in the last decade according to the REA study. The mean cost of treatment for acromegaly is 9668€ (data estimated in 2009, adjusted in 2010), of which SSAs account for 71%. Patients who receive pegvisomant have more aggressive acromegaly with a higher comorbidity rate.
Conflicts of interestEpidemiological data on acromegaly in Spain mainly come from the REA and OASIS studies, conducted with support from Novartis Oncology.
These projects would not have been possible without the Neuroendocrinology group of SEEN and without the collaboration of participating researchers.
Please cite this article as: Sesmilo G. Epidemiología de la acromegalia en España. Endocrinol Nutr. 2013;60:470–474.