Worldwide incidence of thyroid cancer has increased in recent decades.
ObjectiveTo provide evidence of the diagnostic and care efficiency of a monographic thyroid nodule clinic integrating clinical examination, ultrasound examination, and cytology with onsite evaluation.
Patients and methodsPatients attending the monographic thyroid nodule clinic from January 2004 to June 2010. Two periods may be distinguished based on availability of ultrasound equipment at the time of the visit: a first period (P1: 01/2004-09/2007) where no ultrasound equipment was available at the clinic and FNA by palpation was performed, and a second period (P2: 10/2007-06/2010) where this equipment was available and ultrasound-guided FNA was performed.
ResultsA total of 1036 patients [P1: 537 (52%), P2: 499 (48%)] were seen and enrolled.
Diagnostic efficiency (P1 vs P2): 143 vs 181 patients were seen annually, p<0.001; FNA number/nodule: 1.68 vs 1.17, p<0.001; percent FNAs with inadequate material: 26% vs 5.3%, p<0.001; mean (SD) nodule size: 23.6 (12.4) vs 21.7 (11.7)mm, p 0.040; proportion of nodules examined less than 10mm in size: 9.9% vs 13.7%, p 0.030.
Care efficiency: mean time (range) from the first visit to surgery indication: 332 (0–2177) vs 108 (0–596) days, p<0.001; proportion of patients referred for surgery due to suspect cytology/other reasons: 1.06 vs 2.21, p<0.001; and operated benign neoplasm/pathology: 0.47 vs 0.93, p=0.002.
ConclusionA monographic thyroid nodule clinic integrating clinical examination, ultrasound, and cytology evaluated onsite increases diagnostic and care efficiency in patients with thyroid nodules.
La incidencia de cáncer de tiroides ha aumentado en las últimas décadas en todo el mundo.
ObjetivoAportar evidencias sobre la eficiencia diagnóstica y asistencial si la atención al nódulo tiroideo se realiza en una consulta monográfica que integre exploración clínica, estudio ecográfico y citología con valoración in situ.
Pacientes y métodosPacientes que acudieron a la consulta monográfica de nódulo tiroideo entre enero 2004 y junio 2010. Basado en la disposición del ecógrafo en el momento de la visita 2 períodos son definidos: primer periodo (P1: 01/2004-09/2007) sin ecógrafo en la consulta, PAAF por palpación; y segundo periodo (P2: 10/2007-06/2010) con ecógrafo, PAAF eco-guiada.
ResultadosUn total de 1.036 pacientes [P1: 537 (52%), P2: 499 (48%)] fueron consultados e incluidos.
Eficiencia diagnóstica (P1 vs P2): número de pacientes visitados/año fue 143 vs 181, p<0,001; número de PAAF/nódulo: 1,68 vs 1,17, p<0,001; porcentaje de PAAF con material insuficiente: 26 vs 5,3%, p<0,001; tamaño medio (DE) del nódulo: 23,6 (12,4) vs 21,7 (11,7) mm, p 0,040; porcentaje de nódulos estudiados menores a 10mm: 9,9 vs 13,7%, p 0,030.
Eficiencia asistencial: tiempo medio (rango) entre primera visita e indicación de cirugía: 332 (0-2177) vs 108 (0-596) días, p<0,001; relación de pacientes derivados a cirugía por sospecha citológica/por otros motivos: 1,06 vs 2,21, p<0,001; y de neoplasia/patología benigna intervenida: 0,47 vs 0,93, p=0,002.
ConclusiónLa consulta monográfica del nódulo tiroideo, que integra exploración clínica, ecografía y citología con valoración in situ, aumenta la eficiencia diagnóstica y asistencial del nódulo tiroideo.
Thyroid nodule (TN) is a very common condition in clinical practice. Up to 4–7% of the population has a palpable nodule, and ultrasound examination reveals TNs in 50–70% of cases.1 What matters in clinical practice is to determine which patients are candidates for surgery for suspected tumor, so that patients with thyroid cancer, 5–10% of the total population with TNs, are not left untreated.1
The extension of supplementary tests has increased the number of early diagnoses because many patients have silent TNs. This is the main reason for the two–threefold worldwide increase in the incidence of thyroid cancer (TC) in the last decades.2,3 Early diagnosis of TC increases the chances of its being confined to the gland and, depending on size, being managed with surgery alone. Early diagnosis is also important for patients, who experience distress and fear that they may have cancer when they notice a nodule. By contrast, delayed diagnosis increases the chance of extrathyroid tumor extension and more aggressive and expensive surgery, as well as the need for the ablation of thyroid remnants with radioiodine. All of this has an impact on patient quality of life and costs.
The identification of patients with suspected TC requires careful evaluation of each nodule. This is achieved by combining information from the clinical history and physical examination with the information provided by ultrasound. Not all TNs require cytological study. Clinical and ultrasound findings determine the need to perform a cytological study on a sample taken by fine needle aspiration (FNA).4 There is general agreement that FNA may be performed by a radiologist, surgeon, cytologist, or endocrinologist, provided they are adequately trained, for which they should perform from 20 to 35 punctures every year.1 It is also widely agreed that the most effective and inexpensive way to perform FNA is under ultrasound control,5,6 but no studies analyzing on-site evaluation of the material in the final results are available. It is known that the experience of the ultrasonographer7 and the availability of a cytologist experienced in thyroid pathology8 have a positive impact on the diagnostic yield of thyroid nodule.
As regards healthcare staff, efficiency is associated with a higher motivation and creativity.9 The current scientific literature reports evidence of improved therapeutic efficiency when patients with TC are treated and followed up by a multidisciplinary team.10 As to the most effective way of organizing the care of TN, there are diverse opinions concerning the necessity of integrating the different diagnostic tools or promoting on-site evaluation of cytological material,11 but no studies assessing their potential impact on patients and costs are available
The hypothesis of our study was that a monographic TN unit where ultrasound examination is available which allows clinicians to perform all FNAs of TNs and on-site evaluation of cytological material improves both diagnostic efficiency and quality of care. Our aim was to provide evidence of diagnostic efficiency, as assessed by the annual number of patients seen, the number of FNAs performed, and the number of FNAs providing inadequate material for diagnosis, and also of the improvement of certain aspects of care quality, such as the time taken to make a diagnosis and perform treatment, decreases in negative events such as the need to repeat FNA due to inadequate material, or surgery referral criteria, and the type of procedure to be performed.12,13
Patients and methodsStudy designThis was a prospective, single center, cohort study of all patients attending the monographic TN unit for diagnosis from January 2004 to June 2010 inclusive. The study was conducted under conditions of standard clinical practice. The hospital General de Granollers, located in the Vallés Oriental area (Barcelona), covers a population of approximately 320,000 inhabitants. This study was conducted in accordance with the Declaration of Helsinki.
Study populationPatients of both sexes with TN attending for diagnosis and treatment and for whom clinical examination, ultrasound examination, and cytological study using FNA were available.
The following information was collected in real time in an electronic clinical history specifically designed for clinical management and prepared at the same endocrinology clinic14: date of visit, age, sex, reason for unit referral (problem incidentally detected at another examination/by the patient or at a medical visit), TSH, date of FNA, cytological result (Thy: inadequate material for diagnosis, Thy 2: benign, Thy 3: follicular lesion, Thy 4: suspected neoplasm, Thy 5: diagnosis of malignancy), nodule size measured by ultrasound (larger diameter in millimeters), date surgery was indicated, reason for referral for surgery (size, hyperthyroidism, cytological report of suspected malignancy), surgery (hemithyroidectomy, total thyroidectomy, total lymph node dissection), and pathology (hyperplasia, thyroiditis, adenoma, papillary, follicular or medullary thyroid cancer).
Monographic thyroid nodule unitFor more than 20 years, patients with TNs attending our hospital have been seen at the endocrinology department, and each case is discussed at an interdisciplinary committee.
In 2004, the endocrinology department implemented a monographic TN unit in collaboration with the pathology department. This unit was created to care for patients who needed a cytological study of TN, and patients in whom FNA was known to be required were referred to it. At the first visit, FNA was performed by palpation whenever possible, and the suitability of the cytological material was assessed onsite. If ultrasound examination was required, the patients were referred to the radiology department, where a member of the staff performed an ultrasound-guided FNA but the cytological material was not evaluated onsite.
The monographic TN unit was fitted with ultrasound equipment in October 2007. Since then, all patients have undergone clinical and ultrasonographic evaluation at the first visit and ultrasound-guided FNA followed by an assessment of the suitability of the cytological material is performed in all cases. This has made it possible for all the FNAs required to be performed at the unit.
Two periods were defined based on the availability of ultrasound equipment at the unit: the first period (P1, with no ultrasound equipment available) covered the period from January 2004 to September 2007 (45 months), and the second period (P2, with ultrasound equipment available) from October 2007 to June 2010 (33 months). In both periods, the monographic unit operated one morning per week (for 5h) in the outpatient clinics.
In both periods, clinical examination and FNAs (by palpation in P1 and all of them in P2) were performed by the same endocrinologist, and on-site assessment of the suitability of the cytological material was performed by the same experienced professional from the pathology department. When the monographic unit started to operate in 2004, both these professionals had a proven experience in the practice of FNA by palpation. Specific training was provided in ultrasound examination before this diagnostic procedure was implemented.
Ultrasound examinationEach nodule was examined to assess the following: size in the anteroposterior, transverse, and longitudinal axes; the presence of suspicious signs (microcalcifications, hypoechogenicity, ill-defined margins, or anteroposterior diameter longer than transverse diameter); and vascularization using power Doppler. During P1, ultrasound examination was performed using a Logiq 700 MR scanner (GE Medical Systems, Milwaukee, WI) with a 6–9MHz probe, while a Logiq book XP MR scanner (GE Medical Systems, Milwaukee, WI) with a 6–11MHz probe was used in P2. The largest diameter of the nodule under study was always collected from the examination. In P1, ultrasound examination was performed at the radiology department according to schedule. There was no radiologist exclusively assigned to perform such examinations. In P2, ultrasound examinations were always performed by the same examiner (IC) at the monographic unit.
FNA and cytological analysisAs many nodules as deemed appropriate by the examiner were subject to cytological study. If more than one nodule was found, only the nodule with the cytological result suggesting the greatest risk (with the highest score) was considered for statistical analysis. In patients with several nodules with the same cytological diagnosis, the biggest nodule was considered. In both P1 and P2, the criteria for selecting the nodule to be tested included a size greater than 10mm according to medical judgment or smaller nodules with a suspicious ultrasonographic sign or risk factor.
FNA was performed with a 25 or 23gauge needle, coupled to a 10mL single use syringe, without anesthesia. One or more punctures were performed depending on the characteristics of the nodule. FNAs by palpation in P1 and all FNAs in P2 were immediately repeated if the sample taken was not adequate for diagnosis. Fast staining of the sample (Diff-quick stain) was performed for on-site sample assessment. FNA samples taken in P1 at radiology were sent without any assessment being made of the cytological material. In both P1 and P2, samples were subsequently processed for staining with Giemsa and Papanicolaou in equal parts. From January 2004, the pathology department adopted the classification of the British Thyroid Association8 for reporting the cytological results.
The criteria for repeating the FNA were always the same: inadequate TN material, benign TN with greater than 20% growth in an axis at follow-up, or TN with indeterminate cytology not initially referred for surgery in the absence of suspicious clinical or ultrasound criteria.
Statistical analysisNo formal sample size estimation was made, and sample size was defined as the total number of patients attending the TN unit for diagnosis. A descriptive analysis was made of the baseline characteristics of the population enrolled into the study. Continuous variables are given as mean and standard deviation if they follow a normal distribution, or as median and range (minimum–maximum) if they do not follow a normal distribution. Qualitative variables are given as absolute frequency and percentage (n, %).
The difference between the two study periods for qualitative variables was assessed using a Chi-square test, and an ANOVA test was used when quantitative variables were analyzed with other qualitative variables. Ninety-five percent confidence intervals (95% CIs) were calculated, and a value of p≤0.05 was considered statistically significant.
Information was collected using database software (Microsoft Access for Windows XP, Redmont, CA), and statistical analysis was performed using SPSS version 17.1 statistical software.
ResultsPatient characteristicsFrom January 2004 to June 2010, a total of 1036 patients with TN were seen, 537 (52%) in P1 (143 patients/year) and 499 (48%) in P2 (181 patients/year). The number of annual patients attending for a first visit increased in P2, but the weekly time devoted to TN consultation did not increase.
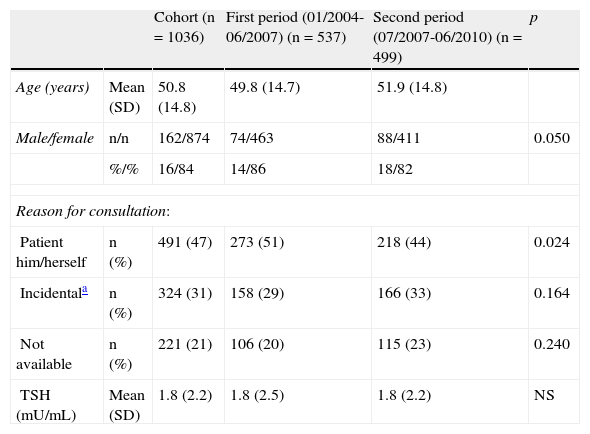
Table 1 shows the characteristics of the study population. As regards the reason for referral, a statistically significant decrease was seen in the ratio “nodule detected by the patient or physician/nodule incidentally detected at another examination” from 1.7 in P1 to 1.3 in P2 (p=0.024).
Baseline characteristics of the study population.
| Cohort (n=1036) | First period (01/2004-06/2007) (n=537) | Second period (07/2007-06/2010) (n=499) | p | ||
| Age (years) | Mean (SD) | 50.8 (14.8) | 49.8 (14.7) | 51.9 (14.8) | |
| Male/female | n/n | 162/874 | 74/463 | 88/411 | 0.050 |
| %/% | 16/84 | 14/86 | 18/82 | ||
| Reason for consultation: | |||||
| Patient him/herself | n (%) | 491 (47) | 273 (51) | 218 (44) | 0.024 |
| Incidentala | n (%) | 324 (31) | 158 (29) | 166 (33) | 0.164 |
| Not available | n (%) | 221 (21) | 106 (20) | 115 (23) | 0.240 |
| TSH (mU/mL) | Mean (SD) | 1.8 (2.2) | 1.8 (2.5) | 1.8 (2.2) | NS |
The result of a total number of 1036 TNs found in 1036 patients is reported. The number of FNAs performed on such nodules was 1485 (FNAs per nodule: 1.68 in P1 and 1.17 in P2; p<0.001). Specifically, two FNAs were performed on 263 nodules during the study period, and 93 nodules required a third FNA. The proportions of patients who underwent FNA on the day of the first visit were 51% (274/537) in P1 and 93% (464/499) in P2 (p=0.0001).
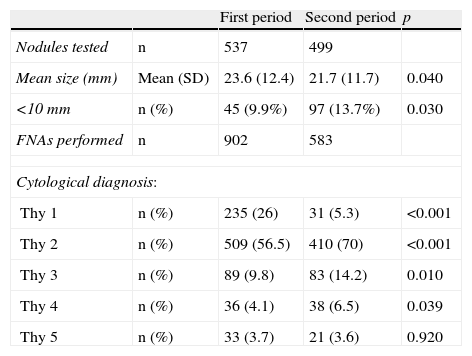
Table 2 gives information about the size and cytological diagnosis of the nodules. The marked decrease in the proportion of cytological results Thy (or inadequate material) in P2 should particularly be noted. On the other hand, nodule size was smaller in P2, and the proportion of nodules less than 10mm in size increased. Mean size (range) of papillary thyroid carcinoma also decreased from 21.7mm (9–55) in P1 to 20.0mm (5–39) in P2 (p=NS).
Size and cytological diagnosis of the tested nodules.
| First period | Second period | p | ||
| Nodules tested | n | 537 | 499 | |
| Mean size (mm) | Mean (SD) | 23.6 (12.4) | 21.7 (11.7) | 0.040 |
| <10mm | n (%) | 45 (9.9%) | 97 (13.7%) | 0.030 |
| FNAs performed | n | 902 | 583 | |
| Cytological diagnosis: | ||||
| Thy 1 | n (%) | 235 (26) | 31 (5.3) | <0.001 |
| Thy 2 | n (%) | 509 (56.5) | 410 (70) | <0.001 |
| Thy 3 | n (%) | 89 (9.8) | 83 (14.2) | 0.010 |
| Thy 4 | n (%) | 36 (4.1) | 38 (6.5) | 0.039 |
| Thy 5 | n (%) | 33 (3.7) | 21 (3.6) | 0.920 |
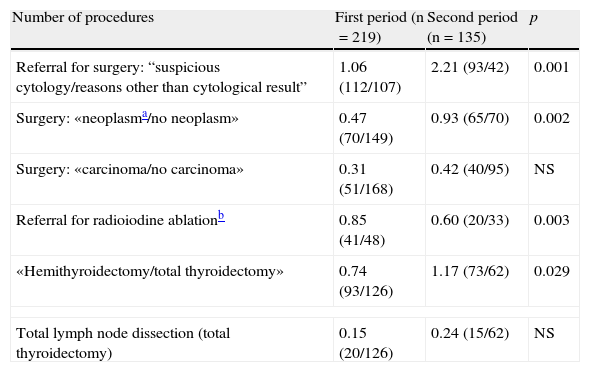
A total of 354 patients (34%) underwent surgery, 41% (219/537, 58 procedures/year) in P1 and 27% (135/499, 49 procedures/year) in P2 (p<0.001). Table 3 shows the results of the types of surgery undergone. The rise in hemithyroidectomies, neoplasm surgery and lymph node dissection, as well as the decrease in radioiodine ablation therapy in P2 should be noted.
Surgery referral criteria, ratio of oncological to non-oncological pathology, referral for radioiodine ablation, and type of procedure performed in the study periods.
| Number of procedures | First period (n=219) | Second period (n=135) | p |
| Referral for surgery: “suspicious cytology/reasons other than cytological result” | 1.06 (112/107) | 2.21 (93/42) | 0.001 |
| Surgery: «neoplasma/no neoplasm» | 0.47 (70/149) | 0.93 (65/70) | 0.002 |
| Surgery: «carcinoma/no carcinoma» | 0.31 (51/168) | 0.42 (40/95) | NS |
| Referral for radioiodine ablationb | 0.85 (41/48) | 0.60 (20/33) | 0.003 |
| «Hemithyroidectomy/total thyroidectomy» | 0.74 (93/126) | 1.17 (73/62) | 0.029 |
| Total lymph node dissection (total thyroidectomy) | 0.15 (20/126) | 0.24 (15/62) | NS |
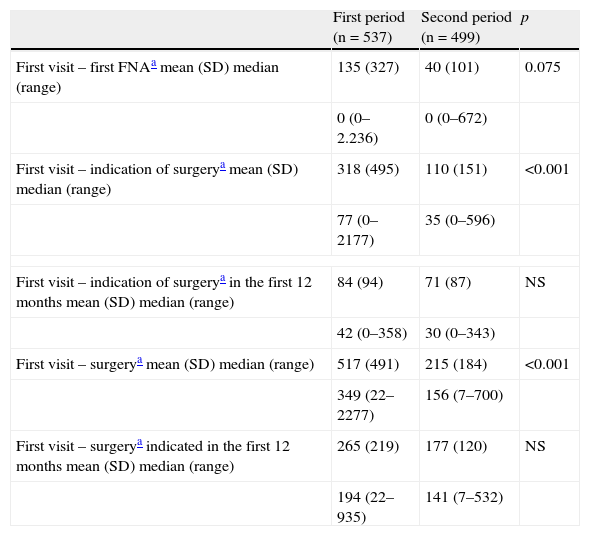
Table 4 shows the times elapsed from the first visit to the indication of surgery and the surgical procedure, showing a clear reduction in the time required to decide on the treatment approach and in the waiting time for surgery in P2, a trend that is maintained if analysis is limited to patients for whom surgery was indicated during the first year of follow-up at the unit.
Times elapsed before diagnosis and treatment.
| First period (n=537) | Second period (n=499) | p | |
| First visit – first FNAa mean (SD) median (range) | 135 (327) | 40 (101) | 0.075 |
| 0 (0–2.236) | 0 (0–672) | ||
| First visit – indication of surgerya mean (SD) median (range) | 318 (495) | 110 (151) | <0.001 |
| 77 (0–2177) | 35 (0–596) | ||
| First visit – indication of surgerya in the first 12 months mean (SD) median (range) | 84 (94) | 71 (87) | NS |
| 42 (0–358) | 30 (0–343) | ||
| First visit – surgerya mean (SD) median (range) | 517 (491) | 215 (184) | <0.001 |
| 349 (22–2277) | 156 (7–700) | ||
| First visit – surgerya indicated in the first 12 months mean (SD) median (range) | 265 (219) | 177 (120) | NS |
| 194 (22–935) | 141 (7–532) | ||
Current medicine needs to search for efficiency more than ever. The integration of clinical evaluation, ultrasound examination, and cytological assessment in one and the same clinic has resulted in a statistically significant reduction in the times taken to make a diagnosis and perform adequate treatment. Our results also show a reduction in the number of FNAs required to reach a diagnosis resulting from a decrease in the number of FNAs providing inadequate material.
Although the monographic TN unit started to operate in 2004, it had an antecedent at the general endocrinology clinic, where the endocrinologist and the cytologist had already started to work in concert. The only difference between the two periods compared was the availability of ultrasound at the time of the visit. A comparison of the results achieved in P2 with the type of care performed before 2004 (data not shown) revealed even greater differences, making the diagnostic and care efficiency achieved in this second period even more evident. These results suggest that when the professional in charge of the patient has the different diagnostic tests available, he/she tends not to delay the tests required, while a delay may occur when these are done at another department not directly responsible for the patient.
While the number of weekly hours available for TN care was the same in both periods, integration in the same care team of all supplemental examinations was shown to be more efficient, as it made it possible to provide care to a higher annual number of patients and to perform less FNAs. The performance of part of the FNAs in P1 by palpation may have been the reason for the higher proportion of inadequate samples, but a post hoc analysis showed that the higher number of FNAs yielding inadequate material in P1 was mainly due to the performance of FNA outside the monographic unit, i.e. without a dedicated examiner and with no on-site assessment of the material. Greater efficiency was also achieved by significantly decreasing both the number of days needed to take a therapeutic decision from the day of the first visit and the waiting time for surgery, which suggests an improved efficiency in the use of resources, since processes of a similar complexity were resolved in a shorter time.13
In patients with TC, the need for specialized care in the setting of an interdisciplinary committee has been recognized and proven.9 The results achieved show that patients were increasingly indicated for surgery on the basis of suspicious or indeterminate cytology, rather than on arbitrary criteria such as nodule size. As a result, an increase occurred in the ratio of patients who underwent surgery for neoplasm as compared to thyroid hyperplasia. This suggests that when clinicians master the different diagnostic tests, they are able to withhold the indication of surgery in patients with no suspected malignancy. In addition, not only were patients with a greater chance of neoplasm operated on, but the type of surgery selected in each case was much more individualized and based on the risk of carcinoma in each patient. The number of hemithyroidectomies (usually indicated for patients with indeterminate cytology and low suspicion of carcinoma) increased, as did the number of total lymph node dissections associated with total thyroidectomy. By contrast, the use of postoperative radioiodine ablation decreased. An explanation for these results may be both an earlier diagnosis of new cases and the trend of the scientific community in recent years to avoid the generalized use of total thyroidectomy and subsequent ablation of remnants with radioiodine, its indication being individually assessed.8,15 On the other hand, the decreased size of new cases of cancer during the second period suggests that changes in care have had an impact on the type of treatment proposed to our patients. However, the decrease in size may also be due to the increasing number of patients seen with small thyroid incidentalomas. As a result, and as has occurred all over the world, the greater incidence of TC less than 1cm in size may have influenced our results.2,3
We think that our results, like those from other recently reported series, confirm that the introduction of ultrasound examination in the hands of endocrinologists results in no impairment in patient care.7,16,17 The care structure discussed in this study is not, by definition, the only way to care for patients. At other hospitals, experience in each field comes from different departments which may achieve results similar or even better than the ones reported here from collaborative work, but a monographic unit is probably the most convenient for patients, who perceive that the physician who treats them is an expert who quickly resolves their case.
Mention should be made of some limitations of the study. It is well known that the experience of healthcare professionals influences the final outcome,7,8 and in our case, the experience accumulated by the professionals, who were highly motivated and convinced of the need to implement the monographic unit, may have led to our overestimating the results. However, this study provides evidence, uncommon in the literature, which shows that attention to the way in which care is organized for treating a highly prevalent health problem such as TN is an essential precondition for achieving optimum results, not only for patients, who gain time and have to wait less, but also for professionals, who increase both their experience and their commitment, and also for the healthcare system, which optimizes its resources. On the other hand, we know that reduction in the waiting time for surgery is a variable that may depend on many factors other than those assessed here. However, the operating room time reserved for thyroid surgery at our hospital was the same in both periods, and we therefore think that our faster indication of surgery has resulted in faster treatment. We also need to assess whether the less common indication of surgery in patients with hyperplastic disease does not represent underdiagnosis of some cases of occult cancer, or whether the smaller size of thyroid cancer at diagnosis or the decreased use of radioiodine ablation has an impact on the future prognosis of such patients.
In conclusion, the integration of the different diagnostic tools by the team caring for patients with TN makes it possible to increase the annual number of patients seen and to decrease the number of diagnostic tests needed. It also shortens the times to diagnosis and treatment. As a result, patients gain time, and our healthcare system optimizes surgical resources to the benefit of the patients most in need of them, those with thyroid cancer.
Conflicts of interestThe authors state that they have no conflicts of interest.
Authors thank Dr. Xavier Serres, Dr. Vicky Yetano, and Dr. Josep Maria Campos for their professional contributions over the years in the thyroid cancer committee of Hospital General de Granollers.
Please, cite this article as: Castells I, et al. Impacto asistencial tras la introducción de la ecografía tiroidea en una unidad monográfica de atención al nódulo tiroideo. Endocrinol Nutr. 2013;60:53–9.