The adequate management of diabetic foot, both uncomplicated or at risk because of complications such as ulcer, infection, or gangrene,1 is a professional challenge inherited from the past century which continues to be a pending subject.2,3 Relatively frequently, infections concomitant with diabetic foot lesions may lead to lower limb amputation. Necrotizing infections are among the most serious of such infections. Soft tissue necrotizing infection or necrotizing fasciitis is an infection involving any soft tissue layers associated with necrotizing changes and causing significant tissue destruction.4 When infection involves the lower limbs of diabetic patients, it is sometimes called wet gangrene; the term ‘necrotizing infection’ is however more adequate. The frequency of necrotizing infection in the diabetic population is not well known. Surgical series have recently reported that up to 30% of infections associated with diabetic foot are necrotizing infections,5,6 but their frequency is much lower (7%) according to other reports.7 These differences may possibly be due to differences in the type of series analyzed, with infection being more common, and thus more serious, in surgical series, and less common when all infected diabetic foot ulcers or lesions are analyzed. We report below the case of a diabetic patient with necrotizing infection which demonstrates the difficulties involved in the diagnostic and therapeutic approach to these patients.
Our patient was a 48-year-old male with type 2 diabetes mellitus (T2DM) diagnosed three years before. The patient did not regularly return for clinical monitoring and was being treated with glimepiride 2mg/day. Prior disease control was not known. He smoked 30cigarettes/day and drank 120g of alcohol daily. His known complications included moderate diabetic retinopathy.
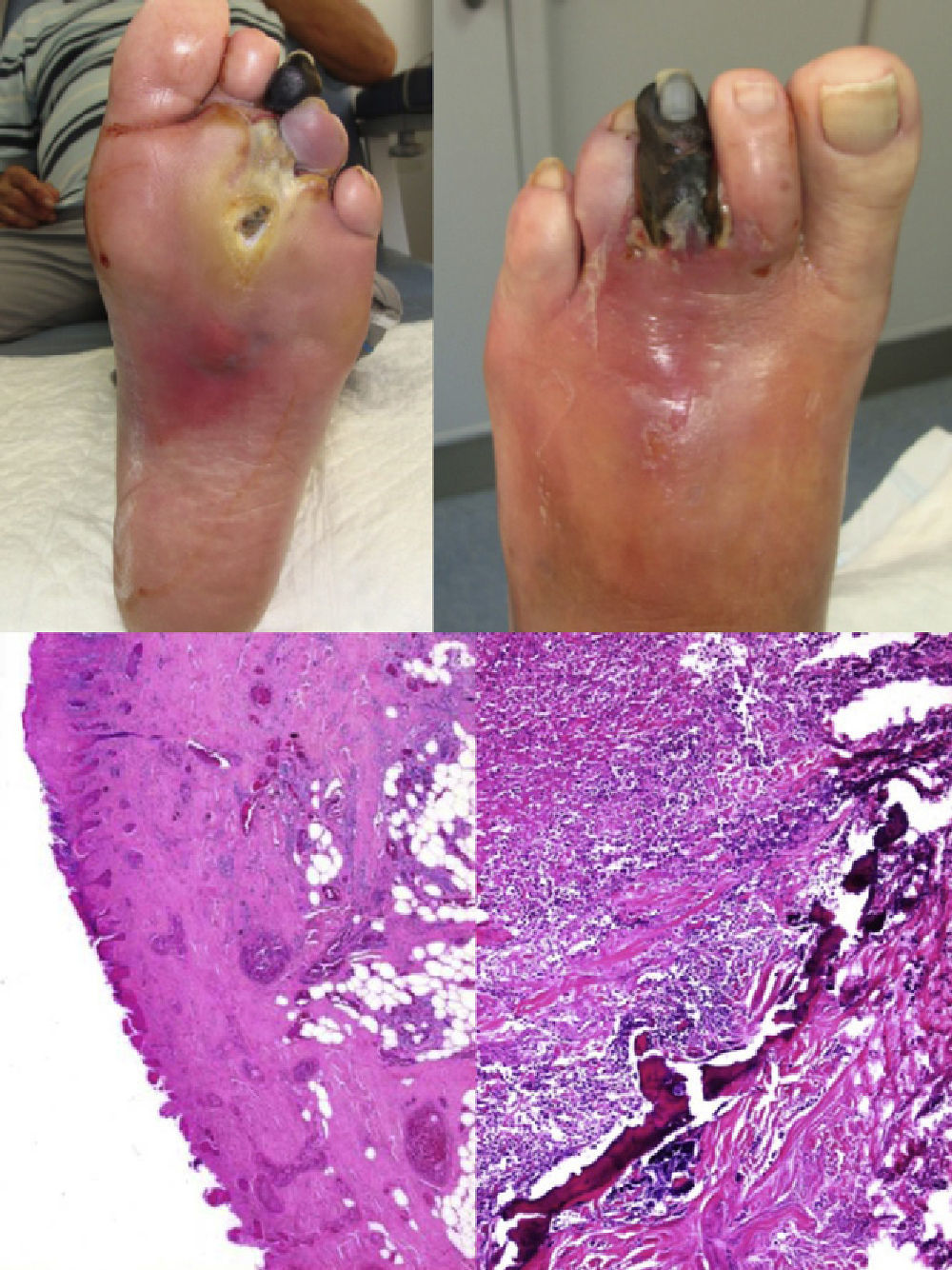
The patient attended the clinic reporting a plantar ulcer on the head of the 3rd metatarsal of his left foot from an unknown date, which had started to be associated with pain in the whole foot and necrosis of the 3rd toe approximately two weeks before. Treatment with amoxicillin/clavulanic acid was started at primary care. No discharge from the lesion was found at this visit. Lower limb examination showed preserved distal pulses, no sensitivity as assessed using the 10g Semmes-Weinstein monofilament, and decreased vibratory sensitivity using the Rydel-Seiffer graduated tuning fork. The left foot showed necrosis in the third toe, cyanosis in the fourth toe, and plantar ulcer with significant exudate, edema, erythema, and increased perilesional temperature (Fig. 1, upper images). Ulcer examination showed positive probing to the bone.
Upper images: top left, plantar view of foot showing an ulcer on the head of the 3rd metatarsal, with marked perilesional reddening and a necrotic 3rd toe. Ulcer was exposed after delamination of the surrounding hyperkeratosis, which is typical in neuropathic lesions. Top right, dorsal view of foot showing reddening of midfoot and 3rd toe necrosis. Lower images: bottom left, blood vessel congestion and dilation, as well as granulation tissue. Ulceration and a necrotic appearance of epidermis and dermis are also seen. Bottom right, intensive, predominantly eosinophilic inflammatory infiltrate with eosinophils involving bone tissue.
After initial evaluation, hospital admission for definitive treatment was decided upon, based on suspicion of necrotizing infection. Baseline laboratory test results included a WBC count of 11,000 with a left shift, blood glucose of 199mg/dL, a sodium level of 124mmol/L, and glycosylated hemoglobin of 8.4% (normal range, 4.2–6). All other results were unremarkable. The patient underwent transmetatarsal amputation of the 3rd and 4th rays, with good postoperative outcome. A microbiological study showed the presence of methicillin-resistant Staphylococcus aureus (MRSA). Antibiotic therapy was therefore switched to sulphametoxazole-trimethoprim. A histological study showed necrosis in the epidermis and dermis, predominantly neutrophilic severe inflammatory infiltrate with eosinophils affecting the area from the epidermis up to the vicinity of bone tissue (Fig. 1, lower images).
As is shown by this case, necrotizing infections require a rapid diagnostic approach and urgent medical and surgical treatment.5 The patient probably had the disease for a longer time than since diagnosis, as he had moderate diabetic retinopathy and a loss of sensitivity from advanced sensory neuropathy, resulting from poor prior glucose control. His history of alcohol consumption probably contributed to the occurrence of neuropathy, as it is usually found in daily practice. The initial infection occurred in the plantar neuropathic ulcer, which is usually indolent until it commonly becomes complicated with infection. In these patients, a lack of education about lesion prevention in an insensitive foot (which is therefore at risk), combined with an absence of pain, usually prevent patients from seeking the help of a healthcare professional until more advanced stages. If we add to this the occasional lack of adequate expertise of some of the professionals in charge of these patients, the result may be a more severe and infected lesion. The presence of pulses ruled out ischemia as the cause of the lesion, and concomitant necrosis suggested a serious infection, even in the absence of signs of systemic impact such as fever, hyperglycemia, leukocytosis and/or an increased erythrocyte sedimentation rate, which is typically found in diabetic patients when infection exists, but may sometimes be absent when a foot is affected.8 In an infected ulcer, a positive probe-to-bone test normally leads us to suspect bone involvement,9 as it was confirmed in this case by the histological study. The isolation of MRSA is relatively common in these infections and may partly account for lesion severity and aggressiveness and for the lack of an initial response to empirical antibiotic therapy. S. aureus is the germ detected in approximately 50% of these infections, and MRSA strains are found in almost half of them.5 Toe necrosis results from arteriolar septic necrosis, caused in turn by neutrophilic vasculitis due to infection itself, and is therefore not caused by ischemia. Revascularization is thus not indicated in cases like this, but should be replaced by extensive surgical debridement and antibiotic coverage, either broad spectrum or specifically directed against the responsible pathogen.10 The patient underwent minor amputation. It should be noted, however, that amputation is required in more than 75% of cases because of the severity of these infections. Several surgical procedures and a major amputation, with the resultant high morbidity, are not uncommonly required to save a limb or prevent the risk of death.5,6 Other crucial issues in the management of these patients include glycemic and co-morbidity control.
To sum up, the presence of necrosis in the foot of a diabetic patient without ischemic involvement should lead to suspicion of necrotizing infection. An aggressive approach including systemic, broad spectrum antibiotic therapy, and urgent surgical treatment consisting of extensive debridement and/or adequate amputation may save the limb and/or life of the patient. Prior identification of a foot at risk, such as an insensitive foot, should prompt preventive measures aimed at avoiding ulcers, which are the harbingers of future amputation.
Please cite this article as: Rubio JA, et al. Infección necrotizante en el pie diabético: una urgencia que amenaza la pérdida de la extremidad. Endocrinol Nutr. 2012;59(7):466–468.