To assess the incidence and perinatal complications of macrosomic infants born to diabetic and non-diabetic mothers.
Patients and methodsA six-year retrospective study of newborns at our hospital. A total of 996 macrosomic newborns were found. Maternal characteristics, mode of delivery, and perinatal outcomes were studied.
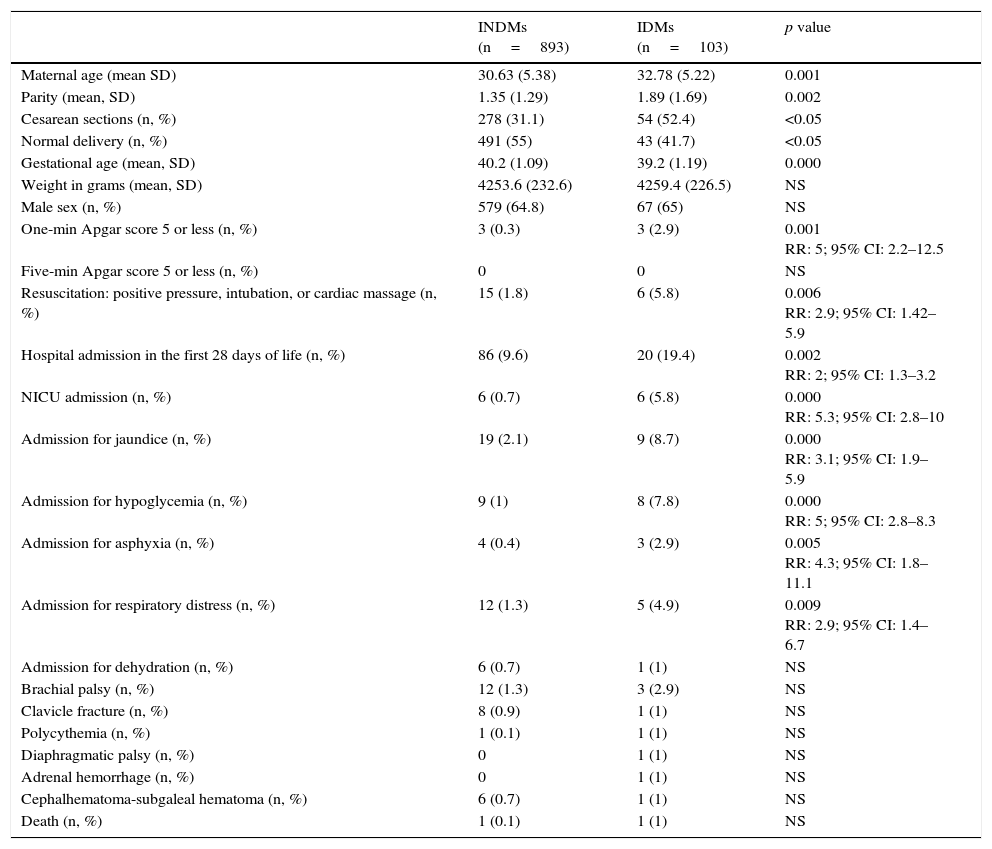
ResultsOf 18,005 newborns, 996 were macrosomic infants (5.53%). Of these, 103 (10.3%) were born to diabetic mothers. Diabetic mothers had higher parity (1.89 vs. 1.35; p<0.000), cesarean section rate (52.4 vs. 31.1%; p<0.05), and resuscitation rate (5.8 vs. 1.8%; p<0.006; RR: 2.9; 95% CI: 1.42–5.9), and greater need for hospitalization (19.4 vs. 9.6%; p<0.002; RR: 2; 95% CI: 1.3–3.2) and intensive care (5.8 vs. 0.7%; p<0.000; RR: 5.3; 95% CI: 2.8–10) mostly for hypoglycemia (7.8 vs. 1%; p<0.000; RR: 5; 95% CI: 2.8–8.3), jaundice (8.7 vs. 2.1%; p<0.000; RR: 3.1; 95% CI: 1.9–5.9), respiratory distress (4.9 vs. 1.3%; p<0.009; RR: 2.9; 95% CI: 1.4–6.7), and asphyxia (2.9 vs. 0.4%; p<0.005; RR: 4.3; 95% CI: 1.8–11.1). No differences were found in birth trauma.
ConclusionsMacrosomic infants born to diabetic mothers have an increased risk of hospital admission in the neonatal period for hypoglycemia, jaundice, respiratory distress, and asphyxia, and a greater need of intensive care. Obstetric trauma rates were similar in both groups.
Determinar la incidencia y las complicaciones perinatales de los recién nacidos macrosomas hijos de madre diabética y macrosomas hijos de madre no diabética.
Pacientes y métodoEstudio retrospectivo de 6 años de los macrosomas nacidos en nuestro hospital. Se encontraron 996 macrosomas. Se estudiaron características maternas, tipo de parto y resultados perinatales.
ResultadosDe 18.005 neonatos, 996 fueron macrosomas (5,53%), siendo 103 hijos de madre diabética (10,3%). La madres diabéticas tenían mayor paridad (1,89 vs. 1,35; p<0,000), porcentaje de cesáreas (52,4 vs. 31,1%; p<0,05), porcentaje de reanimación (5,8 vs. 1,8%; p<0,006; RR: 2,9; IC 95%: 1,42-5,9), mayor necesidad de ingreso hospitalario (19,4 vs. 9,6%; p<0,002; RR: 2; IC 95%: 1,3-3,2) y en cuidados intensivos (5,8 vs. 0,7%; p<0,000; RR: 5,3; IC 95%: 2,8-10); mayor cantidad de ingresos por hipoglucemia (7,8 vs. 1%; p<0,000; RR: 5; IC 95%: 2,8-8,3), ictericia (8,7 vs. 2,1%; p<0,000; RR: 3,1; IC 95%: 1,9-5,9), distrés respiratorio (4,9 vs. 1,3%; p<0,009; RR: 2,9; IC 95%: 1,4-6,7) y asfixia (2,9 vs. 0,4%; p<0,005; RR: 4,3; IC 95%: 1,8-11,1). No existieron diferencias en cuanto a traumatismos obstétricos.
ConclusionesLos recién nacidos macrosomas hijos de madre diabética tienen mayor riesgo de ingreso en el periodo neonatal, incluidos los ingresos por hipoglucemia, ictericia, asfixia, distrés respiratorio y mayor necesidad de cuidados intensivos. Los traumatismos obstétricos son similares.
Macrosomic newborns are arbitrarily defined by some authors as those with weights of 4000, 4100 or even 4500g or greater,1 irrespective of gestational age.
Fetal macrosomia is usually associated with greater perinatal complications. The incidence of macrosomia varies in different regions, ranging from 1–20%.2 Some of the associated causes include sex, parity, the mother's age, weight, maternal height, physical activity, smoking, pregestational and gestational diabetes, and genetic causes. Fetal macrosomia is associated with increased risks for the fetus, especially of obstetric trauma, perinatal asphyxia, death, metabolic changes such as hypoglycemia, or hematological changes such as polycythemia and jaundice.3,4 Few studies have been conducted to assess differences in perinatal outcome between macrosomic infants of diabetic mothers (IDMs) and those of non-diabetic mothers (INDMs).
The purpose of our study was to ascertain the incidence and neonatal complications of IDMs (pregestational or gestational) with weights of 4000g or greater as compared to macrosomic INDMs.
Patients and methodsA retrospective analysis was conducted of all deliveries occurring from January 1, 2010 to December 31, 2015 at Hospital Universitario Santa Lucía in Cartagena, Murcia (Spain). For data collection, delivery and stillbirth forms from the obstetrics department and maternity, as well as admission forms to neonatology and neonatal intensive care units (NICU) during that period and for up to 28 days of life were reviewed.
Histories of newborns, including admissions, supplemental tests, referrals, etc., were reviewed to detect conditions not requiring admission, such as brachial palsy. A differential review was conducted of all newborns also requiring admission.
Measurements and definitionsThe weight of newborns is routinely measured at the maternity ward in the first hour of life using an electronic scale (Seca® 354, Germany). “Macrosomic newborns” are defined as those weighing 4000g or more. In the study, “hypoglycemia” is defined as an episode requiring hospital admission. Blood glucose controls are routinely performed in all macrosomic newborns, IDMs, and those in other risk groups, using capillary blood glucose devices, every hour in the first 4h and every 2–3h thereafter, up to 24h of life. If an infant is asymptomatic and has levels less than 25mg/dL, he/she is fed an artificial formula, and if the blood glucose level is not increased after 1h, he/she is admitted for an intravenous infusion. If values range from 25–40mg/dL, the artificial formula is repeated, and if the level is not greater than 40mg/dL, the infant is admitted. After the first 4h, levels less than 35mg/dL in the first 24h are not accepted, and infants are given the artificial formula or breast milk, repeated 1h later. Infants with values not exceeding 35mg/dL are admitted, and those with levels ranging from 35–45mg/dL are fed again, with a subsequent verification of levels greater than 45mg/dL. All newborns with clinical signs consistent with hypoglycemia and levels less than 40mg/dL are admitted for the parenteral administration of glucose. Similarly, newborns are identified as admitted for “jaundice”, “polycythemia”, “respiratory distress”, “dehydration”, or “cephalhematoma-subgaleal hematoma” when those were the reasons recorded for hospital admission. Our unit follows the criteria of the American Academy of Pediatrics for the treatment of jaundice,5 and dehydration is defined as the clinical signs associated with jaundice together with the loss of more than 10% of birth weight. “Polycythemia” is defined as any venous hematocrit greater than 65%. “Perinatal asphyxia” is defined as encephalopathy associated with an umbilical cord pH less than 7 and a base excess greater than −16. Obstetric trauma includes fractures, brachial and diaphragmatic palsy, and cephalhematoma-subgaleal hematoma. Fractures are diagnosed by X-rays. The brachial palsies studied are those requiring follow-up by rehabilitation and/or pediatric neurology, excluding transient palsy at discharge. “Resuscitation” is defined as the need for intermittent or more advanced positive pressure in the delivery room. At our hospital, cesarean section is indicated for fetal macrosomia when two different observers estimate a fetal weight greater than 4500g irrespective of the diabetes status of the mother. Approval was obtained from the ethics committee of our hospital for our study.
Statistical analysisData were analyzed using SPSS software®, version 22. Descriptive statistics included the mean, standard deviation, and median for continuous data, and percentages for qualitative data; quantitative data were tested using a Kolmogorov–Smirnov test, and were compared between the groups using a Mann–Whitney U test, while quantitative data were compared using a Fisher's exact test. A value of p<0.05 was considered statistically significant.
ResultsA total of 18,005 deliveries occurred during the study, of which 996 were of macrosomic infants (5.53%). Birth weight was 4500g or greater in 0.87% of newborns (n=157) and 5000g or greater in 0.06% (n=11). Of these 996 newborns, 103 were IDMs (10.3% of macrosomic infants: 79 gestational diabetes, 7.9%; 24 pregestational diabetes, 2.4%). There were 68 stillbirths in this six-year period, none of which was a macrosomic fetus. The main results are shown in Table 1.
Characteristics of macrosomic infants born to non-diabetic and to diabetic mothers.
| INDMs (n=893) | IDMs (n=103) | p value | |
|---|---|---|---|
| Maternal age (mean SD) | 30.63 (5.38) | 32.78 (5.22) | 0.001 |
| Parity (mean, SD) | 1.35 (1.29) | 1.89 (1.69) | 0.002 |
| Cesarean sections (n, %) | 278 (31.1) | 54 (52.4) | <0.05 |
| Normal delivery (n, %) | 491 (55) | 43 (41.7) | <0.05 |
| Gestational age (mean, SD) | 40.2 (1.09) | 39.2 (1.19) | 0.000 |
| Weight in grams (mean, SD) | 4253.6 (232.6) | 4259.4 (226.5) | NS |
| Male sex (n, %) | 579 (64.8) | 67 (65) | NS |
| One-min Apgar score 5 or less (n, %) | 3 (0.3) | 3 (2.9) | 0.001 RR: 5; 95% CI: 2.2–12.5 |
| Five-min Apgar score 5 or less (n, %) | 0 | 0 | NS |
| Resuscitation: positive pressure, intubation, or cardiac massage (n, %) | 15 (1.8) | 6 (5.8) | 0.006 RR: 2.9; 95% CI: 1.42–5.9 |
| Hospital admission in the first 28 days of life (n, %) | 86 (9.6) | 20 (19.4) | 0.002 RR: 2; 95% CI: 1.3–3.2 |
| NICU admission (n, %) | 6 (0.7) | 6 (5.8) | 0.000 RR: 5.3; 95% CI: 2.8–10 |
| Admission for jaundice (n, %) | 19 (2.1) | 9 (8.7) | 0.000 RR: 3.1; 95% CI: 1.9–5.9 |
| Admission for hypoglycemia (n, %) | 9 (1) | 8 (7.8) | 0.000 RR: 5; 95% CI: 2.8–8.3 |
| Admission for asphyxia (n, %) | 4 (0.4) | 3 (2.9) | 0.005 RR: 4.3; 95% CI: 1.8–11.1 |
| Admission for respiratory distress (n, %) | 12 (1.3) | 5 (4.9) | 0.009 RR: 2.9; 95% CI: 1.4–6.7 |
| Admission for dehydration (n, %) | 6 (0.7) | 1 (1) | NS |
| Brachial palsy (n, %) | 12 (1.3) | 3 (2.9) | NS |
| Clavicle fracture (n, %) | 8 (0.9) | 1 (1) | NS |
| Polycythemia (n, %) | 1 (0.1) | 1 (1) | NS |
| Diaphragmatic palsy (n, %) | 0 | 1 (1) | NS |
| Adrenal hemorrhage (n, %) | 0 | 1 (1) | NS |
| Cephalhematoma-subgaleal hematoma (n, %) | 6 (0.7) | 1 (1) | NS |
| Death (n, %) | 1 (0.1) | 1 (1) | NS |
SD: standard deviation; IDMs: infants of diabetic mothers; INDMs: infants of non-diabetic mothers; 95% CI: 95% confidence interval; NS: not significant; RR: relative risk; NICU: neonatal intensive care unit.
The mean weight was 4253.6g (SD: 232.6) in the INDM group and 4259.4g (SD: 226.5) in the IDM group, a non-significant difference. Male sex predominated in both groups. Gestational age was significantly longer in INDMs (p 0.000), while maternal age was higher in IBDMs (p 0.000). Diabetic mothers had more deliveries (1.89 vs. 1.35; p<0.002).
As regards the type of delivery, IDMs had a greater proportion of cesarean sections (52.4% vs. 31.1%; p<0.05) and a lower proportion of normal vaginal deliveries (41.7% vs. 55%) (p<0.05). IDMs had a one-min Apgar test score less than 5 more frequently than INDMs (p<0.001; RR 5: 95% CI: 2.2–12.5) and required resuscitation at the delivery room more frequently (p<0.006; RR: 2.9; 95% CI: 1.42–5.9).
IDMs had a higher hospital admission rate in the neonatal period (19.4%) as compared to INDMs (9.6%) (p<0.002; RR: 2.9; 95% CI: 1.3–3.2). The NICU admission rate was also significantly higher in IDMs with macrosomia (5.8% vs. 0.7%; p<0.000; RR: 5.26; 95% CI: 2.86–10). There were also greater admission rates for hypoglycemia (7.8% vs. 1%; p<0.000; RR: 5; 95% CI: 2.8–8.3), jaundice (8.7% vs. 2.1%; p<0.000; RR: 3.1; 95% CI: 1.9–5.9), perinatal asphyxia (2.9% vs. 0.4%; p<0.005; RR: 4.34; 95% CI: 1.8–11.1), and respiratory distress (4.9% vs. 1.3%; p<0.009; RR: 2.9; 95% CI: 1.4– 6.7).
There were no differences in the rates of brachial palsy, diaphragmatic palsy, clavicle fractures, polycythemia, and admissions for dehydration.
DiscussionFetal macrosomia has significant implications at delivery, and is associated with neonatal complications. A higher number of macrosomic versus non-macrosomic stillbirths have been reported. In our study period, no stillbirth meeting this criterion was found. In our study, macrosomic IDMs had more admissions during the neonatal period both in the neonatology department and the NICU, including more admissions for hypoglycemia, jaundice, respiratory distress, and asphyxia, while their risk of obstetric trauma was similar to that of macrosomic INDMs.
In some studies of the symmetry or otherwise of macrosomic IDMs, it was concluded that the risk of hypoglycemia, if macrosomia is symmetrical, is similar to that of children with normal weight.6,7
In some studies, obstetric trauma was more common in macrosomic INDMs8 and in those delivered by the vaginal route, with more admissions to the NICU and lower breast-feeding rates9 in IDMs. By contrast, our study found no differences in obstetric trauma rates, but found an increased need for NICU admission in IDMs, probably related to different criteria for performing a cesarean section. According to another study, IDMs have higher rates of respiratory distress, jaundice, and hypoglycemia, and longer hospital stays.10 Although routine blood glucose controls are performed in all macrosomic newborns, we found a greater need for hospital admission in macrosomic IDMs as compared to INDMs.
Our study has the limitations inherent in retrospective studies, to which we should add the arbitrary definition of macrosomia, our not taking gestational age into consideration, and underestimating the problems which occur in newborns weighing less than 4000g.
ConclusionsMacrosomic IDMs have a greater risk of admission in the neonatal period, both at neonatology and the NICU, including admissions for hypoglycemia, jaundice, asphyxia, and respiratory distress, as compared to macrosomic INDMs. They also have a similar rate of obstetric traumas.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Lloreda-García JM, Sevilla-Denia S, Rodríguez-Sánchez A, Muñoz-Martínez P, Díaz-Ruiz M. Resultados perinatales entre macrosomas hijos de madre diabética y macrosomas hijos de madre no diabética. Endocrinol Nutr. 2016;63:409–413.