No conclusive data exist on the value of a high resolution thyroid nodule clinic for management of nodular thyroid disease. The aim of this study was to evaluate the economic impact of and user satisfaction with a high resolution thyroid nodule clinic (HRTNC) in coordination with primary care.
Patients and methodA prospective, observational, descriptive study was conducted to analyze data from 3726 patients (mean age 61±12 years; 85% women) evaluated at an HRTNC during 2014 and 2015. Demographic data (sex and age), number of ultrasound examinations and fine needle aspiration cytologies (FNAC), referral center and consultation type were assessed.
ResultsIn 2014 and 2015, 3726 neck ultrasound examinations and 926 FNACs (3.8% rated as non-diagnostic) were performed. Among the 1227 patients evaluated for the first time, 21.5% did not require a second endocrine appointment, which resulted in mean estimated savings of 14,354.55 euros. Of all patients, 41.1% were referred from primary care, 33.4% from endocrinology, and 26.5% from other specialties. As compared to 2013, the number of thyroid ultrasound examinations requested decreased by 65.3% and 59.7% in 2014 and 2015 respectively, with mean estimated savings of 137,563.92 euros. Mean user satisfaction assessed was 4.0 points (95% confidence interval, 3.7–4.3) on a 5-point scale.
ConclusionsHRTNCs at endocrinology departments, coordinated with primary care, are a viable, cost-effective alternative with a positive user perception.
No existen datos concluyentes sobre la utilidad de las Unidades de alta resolución de tiroides en el manejo de la patología nodular tiroidea. El objetivo del presente estudio fue evaluar el impacto económico y la satisfacción del usuario tras la puesta en marcha de una consulta de alta resolución de nódulo tiroideo (CARNT) en coordinación con Atención Primaria.
Pacientes y métodoEstudio prospectivo, observacional y descriptivo en 3.726 pacientes (edad media: 61±12 años; 85% mujeres) evaluados en la CARNT durante los años 2014 y 2015. Se evaluaron datos demográficos (sexo y edad), centro y especialidad de derivación, número de ecografías y punciones aspiración aguja fina ecoguiada (PAAF) de tiroides y tipo de consulta.
ResultadosEn 2014 y 2015 se realizaron 3.726 ecografías cervicales y 926 PAAF con un 3,8% con resultado de muestra insuficiente. De las 1.227 primeras visitas, el 21,5% fueron altas directas sin revisión de resultados con un ahorro medio estimado de 14.354,55 euros. El 41,1% procedían de Atención Primaria, 33,4% de Endocrinología general y el 26,5% de otras especialidades. La reducción en 2014 y 2015 del número de ecografías solicitadas al Servicio de Radiodiagnóstico frente a 2013 fue de un 65,3 y un 59,7%, respectivamente, con un ahorro medio estimado de 137.563,92 euros.
La satisfacción media evaluada por el usuario fue de 4,0 puntos (intervalo de confianza 95%: 3,7-4,3) sobre 5 puntos.
ConclusionesLas CARNT en Endocrinología y en coordinación con Atención Primaria es una alternativa viable, coste-eficiente y con una percepción positiva por parte del usuario.
The prevalence of nodular thyroid disease is extremely important today because it affects up to 10% of the general population, a proportion which increases up to 20–70% if imaging studies are used for screening. However, despite the fact that it is the most common endocrine malignancy, only 5% of thyroid nodules are diagnosed as thyroid cancer.1
Neck ultrasound is the imaging test of choice for assessing nodular thyroid disease because of technical improvements and the high resolution of current equipment as well as its wide availability and safety.2 In fact, technical improvements in imaging equipment, specifically in high frequency ultrasonography, have been partly responsible for the increased diagnosis of nodular thyroid disease, which has even come to be regarded as a true epidemic.3
Because of the high prevalence of nodular disease, a global approach is required for this extremely common but rarely malignant condition in which endocrinologists play an essential role in diagnosis and treatment.4 As in other areas of medicine, the implementation of high resolution units may facilitate the diagnosis of the condition and allow for its early treatment and the reduction of associated costs, thus improving the quality perceived by users by decreasing the number of visits (for clinical and hormone assessment, ultrasound examination, and cytology) to a single medical visit.5
High resolution units are widely used in some areas of medicine and have been shown to increase the quality perceived by patients and to decrease financial costs (high resolution units for heart failure, arrhythmia, respiratory insufficiency, etc.).6,7 However, high resolution thyroid units have not been studied globally, are rarely part of a care plan coordinated with primary care,8 and have a variable distribution in Spain.9–11 In fact, they coexist with an organizational model where the patient is assessed by different specialists (endocrinologist, radiologist, pathologist), with a coordinated visit agenda in the best of cases.4,12 Carral et al. recently reported preliminary results showing the economic benefits in direct costs as compared to conventional clinics.13
The aim of this study was to improve understanding of the value, feasibility, economic impact, and user satisfaction associated with these units, based on the experience of a high-resolution thyroid nodule clinic (HRTNC) which is integrated in a comprehensive plan to coordinate care for thyroid disease with primary care, and has ISO-9001:2008 quality standard accreditation.
Patients and methodsThis was a prospective, observational, descriptive study undertaken to assess the feasibility and economic impact of, and satisfaction with, the implementation of an HRTNC at the Department of Endocrinology and Nutrition of Hospital Clínico Universitario de Valladolid and its catchment area (Valladolid East) from January 2014, when the unit started to operate, to December 2015.
All patients referred to the HRTNC for the evaluation of nodular thyroid disease, from primary care, endocrinology, or other hospital departments were assessed.
Before the single visit consultation was implemented, thyroid ultrasonography and ultrasound-guided (US) fine needle aspiration (FNA) had gradually been implemented at the conventional clinic by the three endocrinologists responsible for the HRTNC. Since 2012, virtually all samples for thyroid cytology have been taken at our hospital by the endocrinologist guided by ultrasonography, and less than 10% are considered inadequate for diagnosis. The HRTNC started to operate in January 2014 as part of a comprehensive care model for thyroid disease, coordinated with the primary care clinics in the Valladolid East area, and following the quality criteria for accreditation of the ISO-9001:2008 standard. Patients with thyroid nodular disease are directly referred to the HRTNC from primary or specialized care after the measurement of thyroid function. To ensure adequate compliance, all referrals are screened weekly by the physicians responsible for the HRTNC prior to patient selection for the unit. The criteria and indication for thyroid ultrasonography are assessed at the screening, as well as the priority to be given the appointment, based on the clinical information in the referral report.
At the HRTNC, the three endocrinologists take turns in running a special half-day clinic. The weekly schedule consists of 16 first visits lasting half an hour and 26 follow-up visits of 20min (10min longer than the usual duration of standard endocrinology visits at our hospital). Today, thyroid nodule follow-up in our reference area is performed in virtually all cases at the HRTNC, which has progressively assumed the monitoring tasks of the standard endocrinology clinic.
At the HRTNC, clinical and hormonal assessment, thyroid ultrasonography (General Electric S7 linear probe 9–14MHz, CT, USA), and FNA when required, based on the judgment of the endocrinologist in charge of the clinic according to the unit protocol, itself based on the current clinical guidelines, are performed during a single medical visit.1,14,15 A cytological examination is subsequently performed by the pathology department.
Patients with no clinically significant disease or criteria for performing US-guided FNA are discharged at the visit (high resolution clinic with no review of results), while those undergoing FNA are given an appointment for a review of the cytological results.
Those patients with thyroid nodular disease who are candidates for thyroidectomy are referred to surgery. Patients with no criteria for surgery having benign cytology and stable disease are discharged and referred to primary care with a report explicitly stating the need for repeat referral to the HRTNC between 2 and 5 years from the date of discharge (at the discretion of the endocrinologist in charge), according to the unit protocol based on the current follow-up criteria.1,16
Study variables, estimated direct cost savings, and perceived qualityDemographic data (sex and age), referring center and specialty, the number of ultrasonographies and US-guided FNAs performed at the unit, and the type of consultation (high resolution with no review of results or single visit with appointment for subsequent review) was analyzed. Information on the number of thyroid ultrasonographies requested by physicians of the unit in the 2013–2015 period was obtained from the radiodiagnosis unit.
To estimate the potential financial savings with the model of a single endocrinology visit, only the direct costs of health care not performed were taken into consideration. These included both the cost of a thyroid ultrasonography that would theoretically have been performed at the radiodiagnosis unit and the cost of control at endocrinology of patients attending a direct discharge visit with no subsequent review of results. Direct costs were calculated using a sensitivity analysis of costs to describe how changes in the established prices would have an impact on the economic results by means of a simple univariate analysis of minimum and maximum costs,17 using the updated reference prices of six Spanish regions following the model previously reported by Carral et al.13
The satisfaction of HRTNC users was assessed by anonymous surveys sent by post (with a prepaid envelope) to a representative sample of all the patients seen. Perceived satisfaction was assessed using self-completed surveys based on a 5-point Likert scale where 5 was the maximum value, based on the Outpatient Clinic User Satisfaction Questionnaire validated in Spanish (SUCE).18
Statistical analysisPatient data were entered into a database specifically prepared for that purpose. Continuous variables were displayed as mean±standard deviation, while qualitative variables were given as absolute and relative frequencies (percentages). The results of the sensitivity analysis for financial costs are given as a range of minimum and maximum costs, calculated because of the different reference prices of thyroid ultrasonography and control visits to endocrinologists established in the autonomous communities evaluated following the Carral et al. model.13,19
Perceived satisfaction was assessed using self-completed surveys based on a 5-point Likert scale sent anonymously to patient homes. To ensure representativeness, a systematic sampling with a random start was done from patients seen during the 2014–2015 period, 75% with a 10% error and a value of α=0.05, and a 40% replacement rate being considered an estimate of satisfaction.
Statistical data analysis was performed using Statistical Package for the Social Sciences (SPSS) software, version 17.0 for Windows.
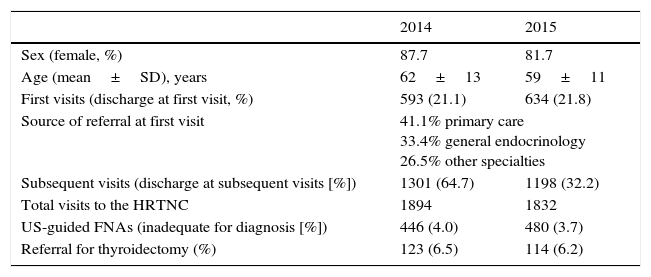
ResultsDuring 2014 and 2015, 1894 and 1832 neck ultrasonographies respectively were performed at the HRTNC, all of them in different patients. Females accounted for 87.7% and 81.7% of all patients seen and had a mean age of 62±13 and 59±11 years respectively. Requests for neck ultrasonography for any reason at the radiodiagnosis department decreased from 1413 in 2013, before the HRTNC was implemented, to 491 in 2014 and to 570 in 2015, i.e. by 65.3% and 59.7% respectively as compared to requests by endocrinologists in a standard clinic setting in 2013.
During 2014 and 2015 there were 593 and 634 first visits respectively. After the first visits, there were 21.5% direct discharges with no control visit (125 and 138 respectively). Of patients attending for a first visit, 41.1% came from primary care, 33.4% from general endocrinology clinics, and 26.5% from other specialties. The specialties with the highest referral rates were otolaryngology (47%), internal medicine (12.2%), and oncology (10.2%). First visits to the HRTNC represented 18.0% of all first visits to endocrinology during the period 2014–2015.
As regards control visits to the HRTNC (1301 and 1198 in 2014 and 2015 respectively), 842 patients (64.7%) were referred to primary care after the control visit in 2014, and 386 (32.2%) in 2015. Control visits performed at the HRTNC represented 11.0% of all controls performed at endocrinology during the period 2014–2015.
Among the 446 and 480 FNAs performed during 2014 and 2015, 4.0% and 3.7% respectively yielded inadequate samples for cytology.
Of the patients seen at the HRTNC in 2014 and 2015, 123 and 114 respectively were referred to the surgical department for possible thyroidectomy due to nodule size or malignant cytology (Table 1).
Activity of the high-resolution thyroid nodule clinic in 2014 and 2015.
| 2014 | 2015 | |
|---|---|---|
| Sex (female, %) | 87.7 | 81.7 |
| Age (mean±SD), years | 62±13 | 59±11 |
| First visits (discharge at first visit, %) | 593 (21.1) | 634 (21.8) |
| Source of referral at first visit | 41.1% primary care 33.4% general endocrinology 26.5% other specialties | |
| Subsequent visits (discharge at subsequent visits [%]) | 1301 (64.7) | 1198 (32.2) |
| Total visits to the HRTNC | 1894 | 1832 |
| US-guided FNAs (inadequate for diagnosis [%]) | 446 (4.0) | 480 (3.7) |
| Referral for thyroidectomy (%) | 123 (6.5) | 114 (6.2) |
HRTNC: high-resolution thyroid nodule clinic; SD: standard deviation; US-guided FNA: fine needle aspiration guided by ultrasonography.
The mean time from the request for an appointment to the actual HRTNC visit was 36.5±10.1 days during 2014–2015.
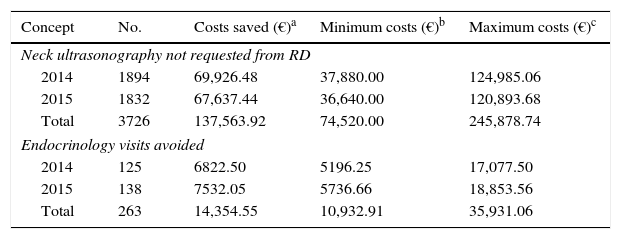
Table 2 shows the potential direct financial savings derived only from the non-performance of thyroid ultrasonography at the radiodiagnosis unit and the non-appointment for a subsequent visit to the endocrinology clinic for a review of the results. During 2014 and 2015, savings were estimated at €137,563.92 (the range of costs in the sensitivity analysis: €74,520.00–245,878.74) as the result of the non-performance of 3726 thyroid ultrasonographies at the radiodiagnosis unit, and €14,354.55 (the range of costs in the sensitivity analysis: €10,932.91–35,931.06) resulting from the 263 first visits followed by direct discharge with no subsequent control at endocrinology.
Estimation of potential direct cost savings in the model of ultrasonography at a single visit to the HRTNC.
| Concept | No. | Costs saved (€)a | Minimum costs (€)b | Maximum costs (€)c |
|---|---|---|---|---|
| Neck ultrasonography not requested from RD | ||||
| 2014 | 1894 | 69,926.48 | 37,880.00 | 124,985.06 |
| 2015 | 1832 | 67,637.44 | 36,640.00 | 120,893.68 |
| Total | 3726 | 137,563.92 | 74,520.00 | 245,878.74 |
| Endocrinology visits avoided | ||||
| 2014 | 125 | 6822.50 | 5196.25 | 17,077.50 |
| 2015 | 138 | 7532.05 | 5736.66 | 18,853.56 |
| Total | 263 | 14,354.55 | 10,932.91 | 35,931.06 |
HRTNC: high-resolution thyroid nodule clinic; RD: department of radiodiagnosis.
From Carral et al.13
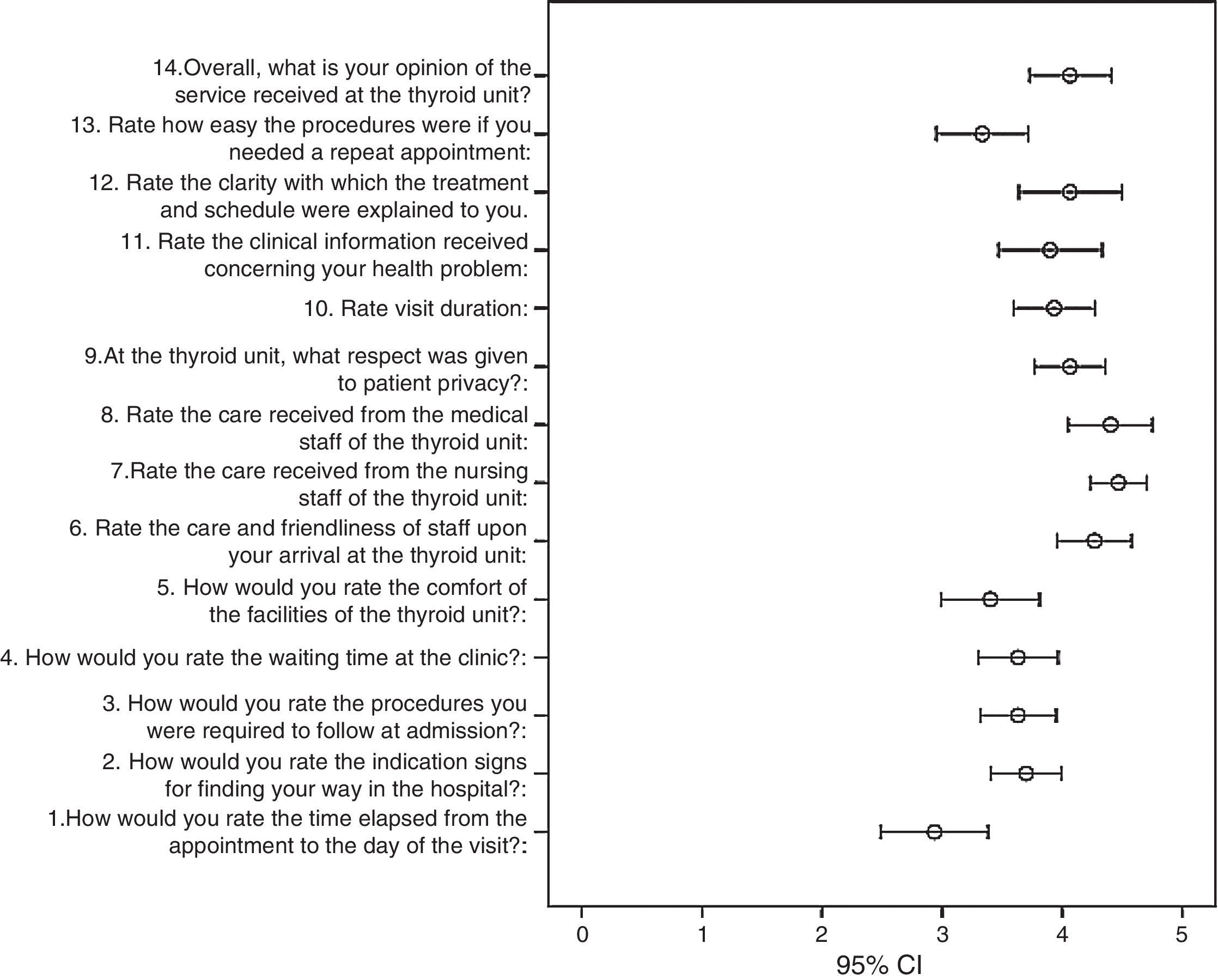
Fig. 1 shows the mean and 95% confidence interval (CI) for each of the 14 items assessed in the satisfaction survey. The mean satisfaction perceived by users was high, with a mean overall perception of 4.0 points (95% CI, 3.7–4.3) out of 5. Items related to waiting time were given the lowest scores.
DiscussionNodular thyroid disease is a condition whose prevalence goes beyond the channels of standard clinical care, as is shown by the fact that thyroid nodular disease is one of the most common reasons for referral to endocrinology departments.20 Its evaluation requires new approaches which should not only pursue the highest technical level, but also improve the efficiency of the system and increase perceived patient satisfaction.21,22
The results of this study support the hypothesis of the improved efficiency and user-perceived quality of high resolution thyroid nodule units (or single visit clinics) run by endocrinologists with the required technical capacity and knowledge, as compared to other models of single visit clinics.4
In this study, the HRTNC was related to a high degree of overall patient satisfaction. This improved satisfaction has been related to the reduction of waiting times and indirect costs, and in the anxiety resulting from the waiting times.13 Although time until the visit was the parameter given the worst score in our study (3.0±1.1 points), this score was higher as compared to that in other studies evaluating activity at outpatient clinics and may have partially contributed to the high degree of overall satisfaction.18
Savings in direct costs derived from the use of the HRTNC in this study are estimated at approximately €70,000 per year, with a range similar to that reported in recent publications.13 Such savings would appear to warrant, at least theoretically, the purchase of ultrasound equipment by endocrinology departments, since they could be repaid in the first year. However, such an approach would be rather simplistic, because the efficiency and savings derived from these clinics is directly related to the technical skills of the endocrinologists in charge of them. FNAs inadequate for diagnosis would obviously represent a significant loss of system efficiency, as a repeat visit and US-guided FNA would be required. This loss would be especially onerous if the rate of inadequate FNAs was to reach 10% or greater.23 In fact, at our center, with seven years of prior experience and only 4% of cytology samples inadequate for diagnosis, the cost derived from repeat FNAs is approximately €1200/year (minimum: €749, maximum: €2459). However, this cost, which can be regarded as given in any consideration of the total savings estimated, may increase exponentially during the learning curve of the ultrasound-guided puncture technique, significantly impairing system efficiency. Both the learning process and the technical training of endocrinologists are therefore indispensable.24
On the other hand, the referral system is an essential variable in any evaluation of the costs associated with the HRTNC. The implementation of the HRTNC at our hospital was part of a comprehensive plan for the coordinated care of thyroid disease with primary care, in the context of accreditation for the ISO-9001:2008 quality standard. All primary care and the specialized physicians working in the Valladolid East area could directly refer to the HRTNC any patient with suspected nodular disease after screening to decrease inadequate referrals (mainly for non-nodular functional thyroid disease). Despite this, 33.4% of first visits resulted from referrals from general endocrinology. That is, a significant number of patients had previously attended the department itself, resulting in impaired system efficiency by incurring a “successive visit” with a cost of approximately €11,188 €/year (minimum: €8522, maximum: €28,007). In our view, however, this is a problem inherent in the system itself, as endocrinologists are the main specialists aware of and qualified to assess thyroid nodular disease in the context of any other endocrine disease and, thus, one of the main actors.
One of the main criticisms of this system is the risk of high visit rates and referral for low complexity or even trivial disease.8,25 In this regard, it should be noted that the Carral et al. study reported 42.3% of direct discharges (with no need for FNA or a control visit), as compared to the 21.5% found in our study. In our view, this high proportion of visits with no need for subsequent control illustrates the risk of referral for low complexity disease which could have been addressed even in a conventional clinic. This suggests that the implementation of well structured protocols with control/screening systems, similar to those used at our center, is needed to minimize this percentage.
Finally, the role of HRTNCs should not be limited to an initial or cytological diagnosis. They should play a primary role in thyroid nodule monitoring and a comprehensive diagnostic process, thus ensuring efficiency. The preparation of protocols based on current criteria for the control of nodular thyroid disease, and based, in particular, on recently reported studies on the re-evaluation of thyroid nodules with prior benign cytology, is essential.1,4,16 In addition, this has allowed in our case for the certification of all the activities performed in this clinic with the ISO 9001:2008 standard. In this regard, the high proportion of patients referred to primary care with benign disease after the control visit (64.7% and 32.2% in 2014 and 2015 respectively) is intended to promote a greater involvement of primary care physicians in the follow-up of these patients with chronic conditions.
The main limitation of this study was that neither the indirect costs derived from savings resulting from decreased travel and working time lost, nor the shorter delay before testing, not to mention other possibilities, were estimated. However, it seems natural to expect that such costs could only have a positive effect on the final financial balance after the implementation of this type of clinic. In addition, satisfaction surveys conducted using self-completed questionnaires sent by post some days after the visit may have had limitations, resulting mainly from a recall bias. However, systematic and random sampling from all patients seen at the HRTNC warrants our acceptance of these results as being representative.
To sum up, the results of this study support the use of HRTNCs managed by endocrinologists in the framework of a comprehensive coordination plan with primary care as a cost-effective alternative which is both feasible in our public health system and viewed positively by users.
FundingThis study was supported by grant GRS 952/A/14 from the Regional Health Management of the Castile and León government.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Díaz-Soto G, Torres B, López Gómez JJ, Gómez Hoyos E, Villar A, Romero E, et al. Impacto económico y satisfacción de la implantación de una consulta de alta resolución de patología nodular tiroidea en Endocrinología. Endocrinol Nutr. 2016;63:414–420.