Therapeutic education (TE) has been gradually introduced progressively into diabetes mellitus care programs with the aim of providing patients and their families or caregivers with the necessary skills for the self-management of the disease. The Diabetes Attitudes, Wishes and Needs 2 (DAWN2) study helps to clarify what are the unmet needs with regards to self-management and the TE offer available to patients and their families. The objective of this paper is to analyze the results of the DAWN2 study regarding self-care habits and participation in TE activities in Spain.
MethodsThe DAWN2 is an observational, cross-national study. In this paper, an analysis was performed on the Spanish sample of diabetic patients (502) and family members (123).
ResultsPatients report taking their medications as recommended by their doctor an average of 6.4 days/week, and self-monitor their blood glucose an average of 3.4 days/week. The large majority (86%) of patients with diabetes mellitus type 1, 59% of patients with diabetes mellitus type 2, and 21% of family members state to have participated in education activities.
ConclusionsDiabetes educators should reinforce the messages about the benefits of self-care, particularly for patients who are in the early stages of the disease. Likewise, access for family members and people with diabetes mellitus type 2 to TE programs should be improved, and these programs for diabetic patients and their families should be included in the services portfolio of health centers.
La educación terapéutica (ET) se ha introducido progresivamente en los programas de atención a la diabetes mellitus para dotar a las personas con diabetes, sus familiares y cuidadores de los conocimientos necesarios para la autogestión de la enfermedad. El estudio Diabetes Attitudes, Wishes and Needs 2 (DAWN2) contribuye a clarificar cuáles son las necesidades no cubiertas en relación con la autogestión de la enfermedad y la ET a disposición de las personas con diabetes y sus familias. El objetivo de este trabajo es analizar los resultados del estudio DAWN2 relativos a hábitos de autocuidado y la asistencia a actividades de ET en España.
MétodosEl DAWN2 es un estudio internacional, observacional transversal. En este trabajo hemos tomado en consideración la muestra española de personas con diabetes (502) y familiares (123).
ResultadosLas personas con diabetes manifiestan tomar la medicación prescrita en la pauta recomendada por su médico 6,4 días de media a la semana y reconocen autocontrolar su nivel de glucosa una media de 3,4 días a la semana. El 86% de los pacientes con diabetes mellitus tipo 1 y el 59% de los pacientes con diabetes mellitus tipo 2 reconocen haber recibido algún tipo de actividad educativa, al igual que el 21% de los familiares.
ConclusionesLos educadores en diabetes deberían reforzar los mensajes acerca de los beneficios derivados del autocuidado, en especial para los pacientes que están en las etapas iníciales de la enfermedad. Asimismo, convendría mejorar el acceso de familiares y personas con diabetes mellitus tipo 2 a programas de ET y reflejar en la cartera de servicios de los centros sanitarios los programas de ET disponibles para las personas con diabetes y sus familiares.
Diabetes mellitus (DM) is a chronic, complex disease that requires active involvement by the people who suffer from it and their families and caregivers, who in each stage of the disease need to take therapeutic decisions to achieve adequate management of the condition. Therapeutic education (TE) has been progressively introduced into DM care programs in order to provide people with diabetes and their relatives or caregivers with the necessary knowledge, skills, and attitudes for the self-management of diabetes and prediabetes. This process incorporates the needs, values, and life experiences of people with diabetes or prediabetes and should be guided by evidence-based care. The objectives include:
- •
To support informed decision making.
- •
To promote adherence to treatment self-management.
- •
To promote problem resolution and active collaboration with health care professionals in order to improve clinical results, health status, and quality of life perception.1
The available evidence suggests that this type of educational intervention would improve patient quality of life,2–5 self-care control,5 and metabolic control.2,3,5,6 It has also been noted that TE may result in decreased care costs,7,8 and also in an increased use of prevention and primary care services.9
There is, therefore, a wide consensus on the importance of providing people with diabetes and their relatives with TE information, resources, and programs to promote the use by patients of a number of routine self-care measures intended to achieve better results in terms of both quality of life and health outcomes.10
Health care professionals in Spain usually support the integration of TE into the health care provided to these patients,11 and training in the self-control of diabetes is one of the main elements both in the diabetes strategy of the National Health System12 and in the diabetes programs of regional Health Departments.13–15
As regards evaluation, Health Departments have been measuring patient satisfaction with the TE received, and the Basque Health Service has also conducted a randomized clinical trial to assess the effectiveness of its education program in self-care “Active Patient” in terms of clinical results (metabolic control and cardiovascular risk) and quality of life.16,17 A randomized clinical trial recently conducted in Murcia also assessed the effectiveness of health education associated with physical exercise in patients with type 2 diabetes mellitus (T2DM) and reported positive, but not statistically significant, results in metabolic control, body mass index, blood pressure, and lipid profile, as well as increased dietary compliance, physical exercise, and self-moitoring.18
The international study Diabetes Attitudes, Wishes and Needs 2 (DAWN2), comprising approximately 16,000 adult patients from 17 different countries, has helped to clarify the unmet needs as regards disease self-management and TE availability to people with diabetes and their families.19 Among other aspects, the study describes the psychosocial and educational needs of people with diabetes and their families and, based on their opinions, areas for improvement in TE have been identified.
The purpose of this paper was to analyze the results of the Spanish sample of patients and relatives in the DAWN2 study in terms of their self-care habits and their participation in educational programs.
Subjects and methodsStudy design and participantsDAWN2 is an international, observational, cross-sectional study. A total of 8596 adults with diabetes, 2047 relatives, and 4785 health care professionals from 17 countries were enrolled into the study.19 A total of 909 people participated in Spain, consisting of 502 patients with diabetes, 123 relatives, and 284 health care professionals. Only the Spanish sample of people with diabetes and relatives is analyzed in this paper.
A mixed methodology was used to recruit patients, as some were invited to participate via electronic mail and some by telephone. The first group was recruited from online panels, while patients contacted by phone were identified from phone listings of people with diabetes. The patient sample included people over 18 years of age diagnosed with diabetes more than 12 months before, excluding patients with gestational diabetes.
Relatives were also recruited by phone or email, and the sample was selected from the references of patients and online panels. The sample of relatives consisted of adults (≥18 years) not diagnosed with diabetes living in the same home as an adult with diabetes and who were involved in his/her care.19 They all answered the questionnaire electronically.
QuestionnairesThe questionnaires used, specific to each of the groups participating in the study (patients and relatives), were prepared from a patient-centered care model by the Global DAWN2 Survey Working Group with the cooperation of experts and representatives of patients from all countries participating in the study. In addition to collecting sociodemographic and disease profile information, the questionnaires examined aspects related to disease self-management, health care quality, psychosocial aspects, quality of care, TE, family and social support, and areas for improvement in diabetes care. To ensure quality and understanding of the language used in the questionnaires, they were translated from English into Spanish and subsequently reviewed by Spanish experts in diabetes.19
Self-care of patients with diabetes was assessed using the questionnaire Summary of Diabetes Self-Care Activities Measure.20 This instrument measures patient perception in different aspects of the daily self-management of diabetes, including diet, physical exercise, glucose measurement, foot care, and treatment adherence.
Statistical analysesThis paper gives the results of the Spanish sample of the DAWN2 study as regards disease self-management and educational interventions. Mean and standard deviation have been used to provide the results of continuous variables and absolute and relative frequencies for categorical variables. Significance analyses were performed using a Chi-square test for categorical variables and a Mann–Whitney U test for continuous variables. A descriptive analysis of diabetes self-management and education based on these results was performed in the Spanish sample of patients and relatives.
The minimum sample size by country was 900 participants (500 patients, 120 relatives, and 280 health care professionals). In each participating country, a sample size of patients and health care professionals adequate to achieve an 80% statistical power to detect a clinically relevant effect was estimated; that is, a moderate size effect in quantitative variables (Cohen's d=0.5). The minimum sample size by country was 120 relatives to have an 80% power to detect in the categorical variables 10% differences in difference of proportions.19
Ethical issuesThe protocol of the international DAWN2 study was submitted to the New England Institutional Review Board in the USA, and was approved before study start. The New England Institutional Review Board reviewed and approved, in addition to the protocol, the informed consent form, questionnaires for patients, relatives, and health care professionals, and all written information to be provided to participants, as well as procedures for the recruitment of participants.
In Spain, the study was conducted in compliance with the guidelines for performing noninterventional studies, using as minimal standard requirements the principles established by the International Chamber of Commerce/European Society for Opinion and Marketing Research (ICC/ESOMAR 2007) and the Council of American Survey Research Organizations (CASRO 2011).
To ensure confidentiality of information, adequate encrypting measures were used for data management, and personal data which could have made possible the identification of participants were removed at all phases of the project. Informed consent was obtained from all participants by electronic means or by phone, depending on the procedure used to answer the questionnaire, and participation was voluntary.
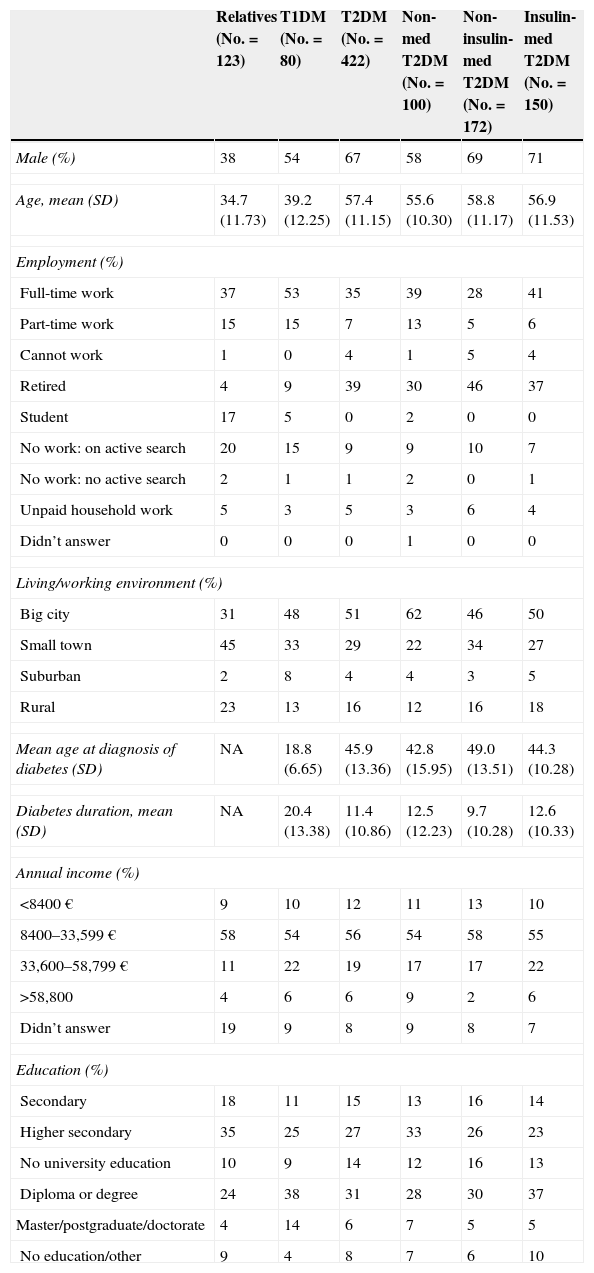
ResultsParticipantsIn Spain, a total of 502 patients with diabetes and 123 relatives participated in the DAWN2 study. Table 1 shows the sociodemographic and clinical characteristics of the Spanish sample of patients and relatives. Seventy percent of people with diabetes answered the questionnaire by electronic means, and the remainder by phone. All relatives answered the questionnaire by electronic means.
Characteristics of the sample of relatives and patients: DAWN2 Spain.
| Relatives (No.=123) | T1DM (No.=80) | T2DM (No.=422) | Non-med T2DM (No.=100) | Non-insulin-med T2DM (No.=172) | Insulin-med T2DM (No.=150) | |
|---|---|---|---|---|---|---|
| Male (%) | 38 | 54 | 67 | 58 | 69 | 71 |
| Age, mean (SD) | 34.7 (11.73) | 39.2 (12.25) | 57.4 (11.15) | 55.6 (10.30) | 58.8 (11.17) | 56.9 (11.53) |
| Employment (%) | ||||||
| Full-time work | 37 | 53 | 35 | 39 | 28 | 41 |
| Part-time work | 15 | 15 | 7 | 13 | 5 | 6 |
| Cannot work | 1 | 0 | 4 | 1 | 5 | 4 |
| Retired | 4 | 9 | 39 | 30 | 46 | 37 |
| Student | 17 | 5 | 0 | 2 | 0 | 0 |
| No work: on active search | 20 | 15 | 9 | 9 | 10 | 7 |
| No work: no active search | 2 | 1 | 1 | 2 | 0 | 1 |
| Unpaid household work | 5 | 3 | 5 | 3 | 6 | 4 |
| Didn’t answer | 0 | 0 | 0 | 1 | 0 | 0 |
| Living/working environment (%) | ||||||
| Big city | 31 | 48 | 51 | 62 | 46 | 50 |
| Small town | 45 | 33 | 29 | 22 | 34 | 27 |
| Suburban | 2 | 8 | 4 | 4 | 3 | 5 |
| Rural | 23 | 13 | 16 | 12 | 16 | 18 |
| Mean age at diagnosis of diabetes (SD) | NA | 18.8 (6.65) | 45.9 (13.36) | 42.8 (15.95) | 49.0 (13.51) | 44.3 (10.28) |
| Diabetes duration, mean (SD) | NA | 20.4 (13.38) | 11.4 (10.86) | 12.5 (12.23) | 9.7 (10.28) | 12.6 (10.33) |
| Annual income (%) | ||||||
| <8400€ | 9 | 10 | 12 | 11 | 13 | 10 |
| 8400–33,599€ | 58 | 54 | 56 | 54 | 58 | 55 |
| 33,600–58,799€ | 11 | 22 | 19 | 17 | 17 | 22 |
| >58,800 | 4 | 6 | 6 | 9 | 2 | 6 |
| Didn’t answer | 19 | 9 | 8 | 9 | 8 | 7 |
| Education (%) | ||||||
| Secondary | 18 | 11 | 15 | 13 | 16 | 14 |
| Higher secondary | 35 | 25 | 27 | 33 | 26 | 23 |
| No university education | 10 | 9 | 14 | 12 | 16 | 13 |
| Diploma or degree | 24 | 38 | 31 | 28 | 30 | 37 |
| Master/postgraduate/doctorate | 4 | 14 | 6 | 7 | 5 | 5 |
| No education/other | 9 | 4 | 8 | 7 | 6 | 10 |
SD: standard deviation; T1DM: patients with type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; Insulin-med T2DM: patients with type 2 diabetes treated with insulin; Non-insulin-med T2DM: patients with type 2 diabetes on antidiabetic treatment other than insulin; Non-med T2DM: patients with type 2 diabetes with no medication; NA: not applicable.
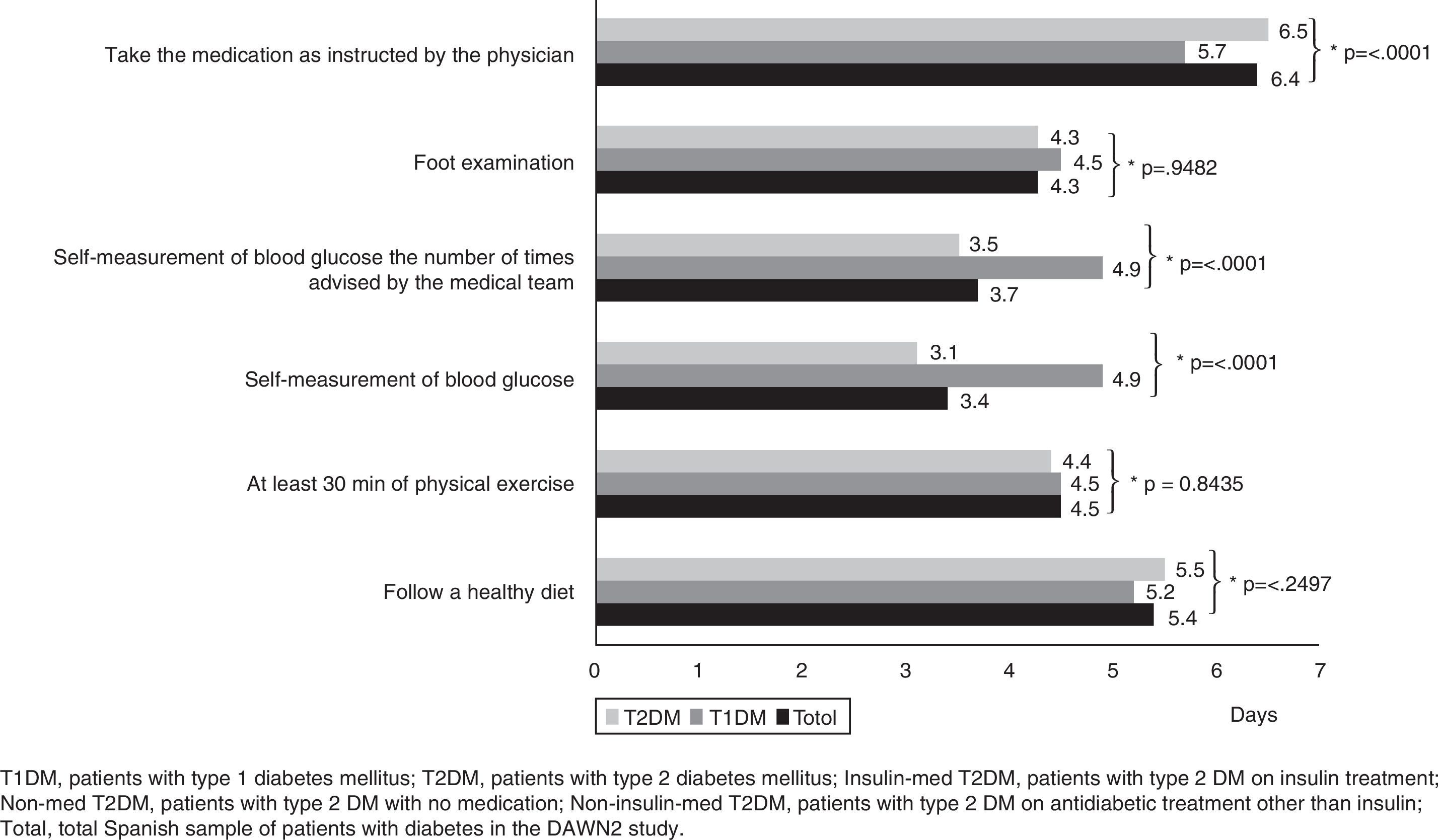
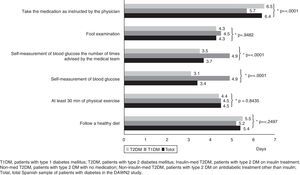
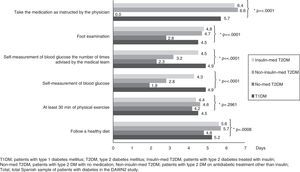
People with diabetes reported that they took the medication prescribed by their physicians in the recommended dosage 6.4 days per week on average. Patients with T2DM complied with drug treatment 6.5 days per week on average, while those with type 1 diabetes mellitus (T1DM) complied with treatment 5.7 days per week (p<0.0001; Fig. 1).
Overall, the sample of Spanish people with diabetes stated that they followed a balanced diet 5.4 days per week on average. As regards physical exercise, patients stated that they did at least 30min of physical exercise 4.5 days per week on average (Fig. 1).
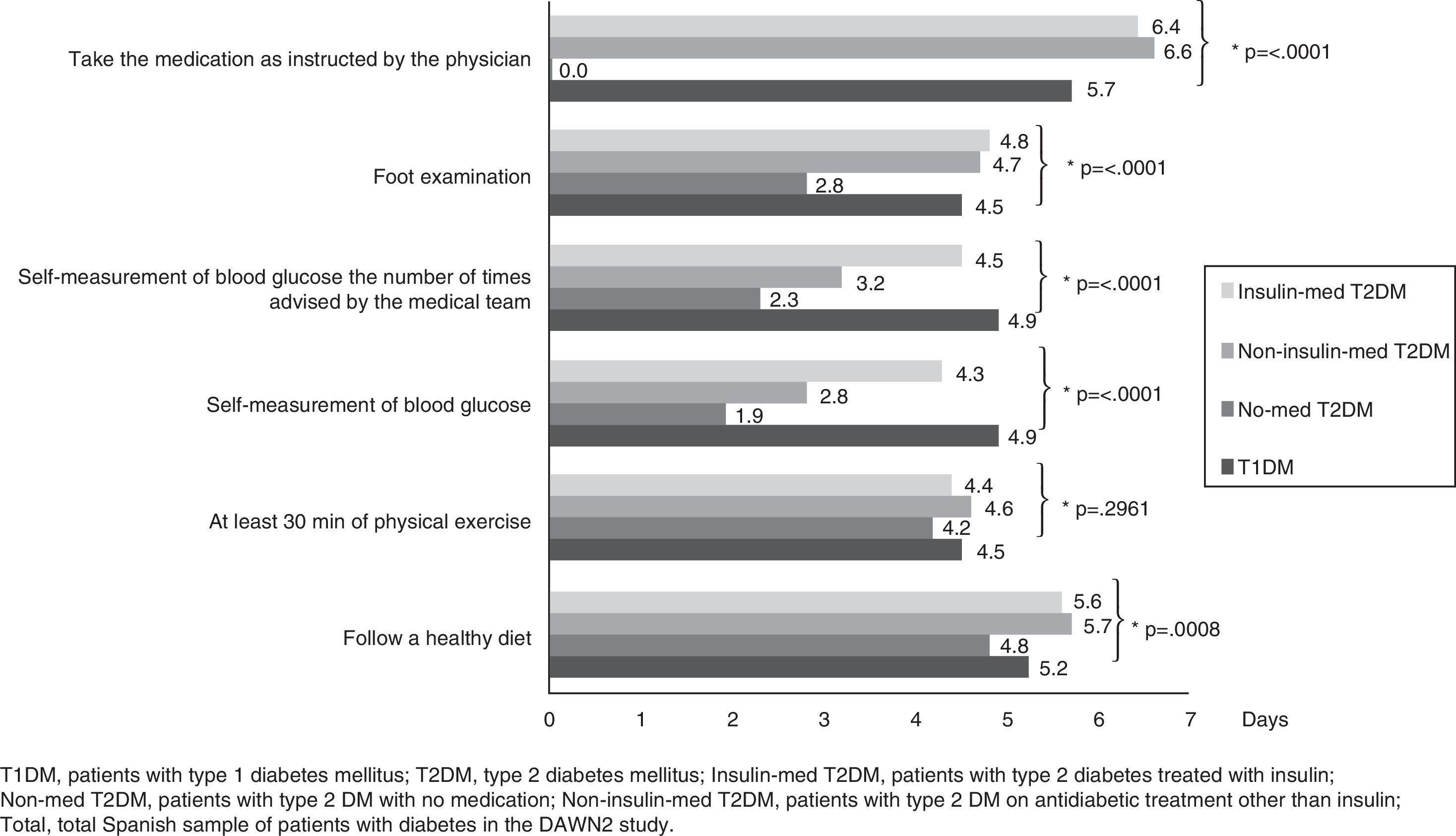
People with diabetes also reported self-monitoring of blood glucose levels 3.4 days per week on average. Patients with T1DM and T2DM treated with insulin self-monitored their glucose levels more days per week (T1DM: 4.9 days/week; T2DM: 4.3 days/week; Fig. 2), while patients with T2DM without drug treatment performed self-monitoring 1.9 days per week on average (Fig. 2).
Mean days per week in which participants performed self-care activities by type of diabetes and treatment. T1DM: patients with type 1 diabetes mellitus; Insulin-med T2DM: patients with type 2 diabetes treated with insulin; Non-insulin-med T2DM: patients with type 2 diabetes on antidiabetic treatment other than insulin; Non-med T2DM: patients with type 2 diabetes with no medication.
On the other hand, patients reported that they performed the number of self-monitoring tests recommended by their physicians 3.7 days per week on average (people with T1DM: 4.9 days/week; people with T2DM treated with insulin: 4.5 days/week; Fig. 2).
Patients diagnosed 6 or more years before reported glucose self-monitoring 3.8 days/week, while those diagnosed 5 or fewer years before performed glucose self-monitoring 2.5 days per week on average.
Finally, the overall sample of Spanish patients reported foot self-examination 4.3 days per week on average. People diagnosed with T2DM receiving no antidiabetic drug treatment reported foot self-examination 2.8 days per week on average (Fig. 2).
As regards support from other people, 69% of patients with diabetes stated that their medical team had represented a significant support for disease management over the previous year. Sixty-eight percent of patients with T2DM and 75% of those with T1DM reported that they had received support from their medical team (p=0.2307). On the other hand, significant support from the medical team was reported by virtually all patients in the subgroup aged <40 years (84%), and by somewhat lower proportions of patients in other age groups (40–59 years, 67%; >60 years, 68%; p=0.0693).
As regards the support received from other groups, only 13% of patients with diabetes stated that their colleagues, classmates, or people from their community had represented a significant support in the management of their disease over the previous year.
On the other hand, 66% stated that their families had given significant support in the management of their disease over the previous year. Approximately two thirds of patients with TD2M (65%) and 73% of those with TD1M recognized such support (p=0.2322). On the other hand, a little over one half (57%) of patients >60 years reported substantial support from their families, as compared to 76% of patients <40 years and 72% of those aged 40–59 years (p=0.0029).
Thirty-seven percent of relatives felt frustrated by not having the knowledge required to help their relative with diabetes to manage the disease; a little over one half (55%) were keen on becoming more involved in the diabetes care of their relative; and 59% desired to help him/her to better manage his/her emotions related to the disease.
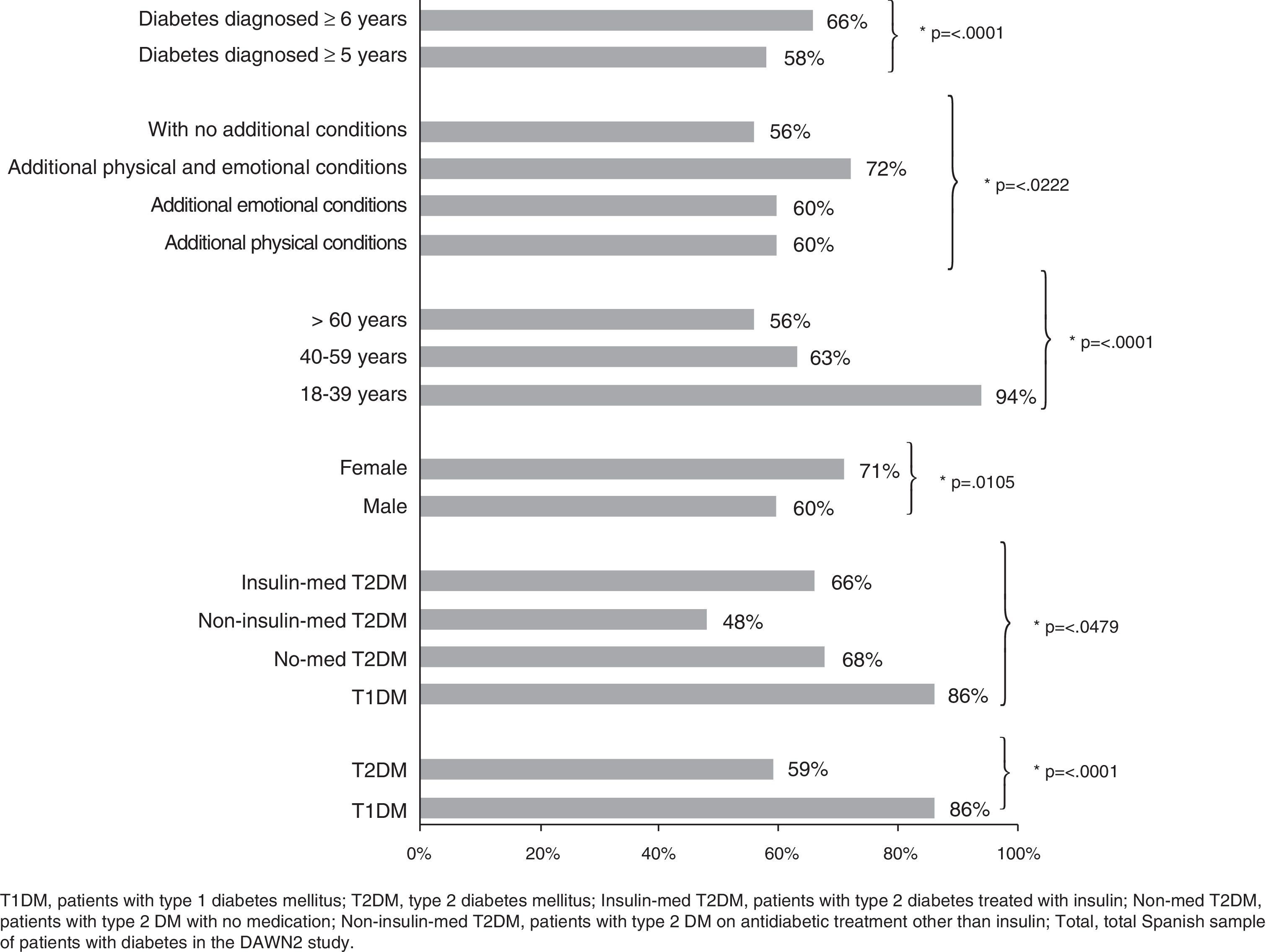
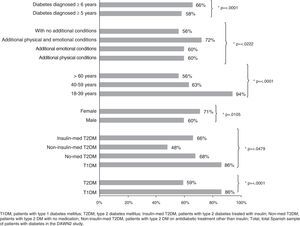
Educational interventionsSixty-four percent of patients with diabetes had participated in an educational program at one time or another, including, for example, training sessions on diabetes and its management through the Internet or in person, or programs intended to promote healthy lifestyles through diet or physical exercise. Virtually all patients with T1DM (86%) and 59% of those with T2DM stated that they had received some training (p<0.0001; Fig. 3). In addition, slightly fewer than half the patients with T2DM treated with oral antidiabetic drugs (48%) had participated in a diabetes education program (Fig. 3). Fig. 3 shows the different participation in these activities by patient subgroups according to type of diabetes, treatment, sex, age, time since diagnosis, and the presence or not of additional diseases.
Patients with diabetes who have participated in any education program by demographic and clinical characteristics (%). T1DM: patients with type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; Insulin-med T2DM: patients with type 2 diabetes treated with insulin; Non-insulin-med T2DM: patients with type 2 diabetes on antidiabetic treatment other than insulin; Non-med T2DM: patients with type 2 diabetes with no medication.
Finally, 21% of relatives reported participation in educational programs; of these, 85% considered that the training received had been beneficial.
DiscussionThe results of the DAWN2 study in Spain reveal that people with diabetes have a good record of adherence to the drug treatment prescribed by their physicians and that they usually follow a balanced diet. By contrast, they are less strict with themselves when it comes to following advice on self-care related to physical exercise, foot care, and glucose monitoring. These results are consistent with those of the overall sample of the DAWN2 study.21
The level of participation in diabetes educational programs can be regarded as acceptable; almost two thirds of Spanish participants reported their participation in some type of activity (Fig. 3). However, although percent participation was higher than the mean in the overall DAWN2 study (64% in the Spanish cohort vs 49% in the overall sample), the level of participation was below that reported in European countries such as Denmark, The Netherlands, and Germany, where approximately 70% of patients reported that they had participated in educational programs.21
Although widespread consensus exists regarding the need to include educational interventions for self-care in diabetes care programs, the results of this study suggest that access to TE programs should be improved, especially for patients with T2DM, who participate in such activities significantly less often than patients with T1DM (Fig. 3). Specifically, it would appear advisable to take action to encourage the greater participation of patients with T2DM, particularly non insulin-treated patients treated with oral antidiabetic drugs, since fewer than half of them had received TE.
It should be noted that patients with T2DM who were not receiving any antidiabetic drug treatment were those who less frequently included in their daily routine the various self-care activities, especially glucose self-monitoring and foot examination (Fig. 2). The reasons for this lower adherence are not known, but it seems logical to think that in the early stage of the disease patients do not perceive the immediate benefit of such self-care activities. In any case, further studies should be conducted to find out the reasons for this difference in behavior, and the contents of TE programs should be modified by having greater emphasis placed on motivating people recently diagnosed with the disease.
As regards the participation of relatives in educational programs, their attendance was very limited, despite the positive opinion of most of them regarding the activities they had attended. It should also be noted that more than one third of these relatives reported that they felt frustrated by not knowing how to provide support to his/her relative with diabetes, and that more than half of them said that they would be interested in playing a more active role in the care of the people with diabetes for whom they were responsible. It therefore appears that these relatives are both motivated and predisposed to help, and that their low participation could partly be due either to a lack of official encouragement or to their ignorance of the existence of educational programs for relatives.
There is also a significant margin for improvement in the role played by the community in supporting patients with diabetes, as shown by the low proportion of patients (13%) who stated that they felt supported by the members of their community. Aspects such as the promotion of physical exercise or a healthy diet should play a more prominent role in local policies, thus reinforcing the messages received by patients and relatives in educational programs. Any such community intervention would also have a favorable impact not only on diabetes management and prevention, but also on the prevention of other chronic diseases such as chronic respiratory diseases, cardiovascular diseases, or cancer, which share with diabetes the same risk factors: physical inactivity, unhealthy diet, smoking, and alcohol abuse.22
Analysis of the results of the DAWN2 study in Spain has contributed to identifying needs and areas for improvement in TE for self-care. Joint examination of self-care habits and the degree of participation in educational programs makes it easier for us to know the types of messages that should be reinforced and to know which patient subgroups most require encouragement to participate in educational programs. An additional strength of this study is that it gives us the viewpoint of relatives regarding their capacity to support patients in their self-care and expectations, so allowing for the easier adaptation of educational interventions to the needs of this group.
On the other hand, the study methods have some limitations which have been thoroughly discussed in other publications21 and should be taken into account when interpreting the study results. Specifically, because of the methodology used to recruit participants, it cannot be stated that the sample is representative of the Spanish population of patients with diabetes and their relatives. In addition, the recruitment process was closed once the established number of patients (502) and relatives (123) was reached in each country. Thus, not all eligible subjects were able to participate in the study. On the other hand, we do not know the characteristics of those subjects who refused to participate in the study and their reasons for such refusal. We also do not know whether or not, and if so to what extent, the means used for collecting the answers, mostly electronic, might have affected the content of the answers received.
In any case, this is a descriptive analysis that only allows for the generation of hypotheses for future analyses. Additional studies will be required to assess the effectiveness of diabetes education and self-care and their impact on the health status and quality of life of people with diabetes.
ConclusionsAll people with diabetes should acquire the knowledge, skills, and attitudes required to make self-care part of their daily routine. The results of the DAWN2 study in Spain show that people with diabetes followed the advice of their team of health care professionals on the use of the medication prescribed. However, they neglected other types of self-care, such as glucose self-monitoring or foot examination, especially in the early stages of the disease.
On the other hand, the participation of people with diabetes in educational programs was moderate, albeit with significant differences between patients depending on the type of diabetes. Thus, while only a little over half the patients with T2DM reported that they had received training, virtually all patients with T1DM had received training at some time.
The methodological limitations of the study prevent us from knowing whether the results may be extrapolated to the whole population of patients with diabetes and their relatives in Spain. In any case, the results obtained allow us to draw a number of conclusions regarding self-care, the provision of TE programs, and the support given to people with diabetes in the management of their disease.
In view of the results, diabetes educators should reinforce their messages on the benefits of self-care, especially for patients in the early stages of the disease. It would also be advisable to improve access to TE programs for patients with T2DM, particularly those on oral antidiabetic drugs who have not yet started insulin therapy.
The professional team is an essential support for people with diabetes in the management of their disease. However, the psychosocial and communication skills of professionals need to be reinforced to allow them to connect more effectively with those patients with more complex diabetes (children, the elderly, or people with several diseases or complications associated with diabetes). On the other hand, although patients with diabetes and their relatives bear the main burden of self-care, it would be a very positive measure for them if they were to find greater support in their communities in aspects such as the promotion of physical exercise or the development of healthy dietary habits.
Since care plans and control goals are jointly addressed with the patient and people around him/her, it is important that the relatives perceive that they have the knowledge needed to support the patient with diabetes. Despite the interest declared by relatives in supporting their loved ones, only a small number of them have actually participated in educational programs. However, those relatives who have done so have a positive opinion of them. In order to improve the current situation, measures should be taken to decrease this gap between the educational opportunities available and the apparent lack of demand for them by families.
Finally, we recommend that the TE programs intended for the different subgroups of patients with diabetes and their relatives or caregivers be included in the portfolio of services of primary and specialized care centers. Training in diabetes and TE of the members of the care team (physicians, nurses, podiatrists, etc.), especially nursing staff and dieticians, should also be taken into account, because these are the professionals most involved in the development of these educational programs in clinical practice.23–25
Conflicts of interestEdelmiro Menéndez Torre is a member of the Advisory Board of the DAWN2 study, but has received no fees from NN for this collaboration. In the past he has received fees for acting as a speaker from Novo Nordisk, Novartis, Eli Lilly, and Sanofi.
Margarida Jansà Morató and Mercedes Galindo Rubio are members of the expert panel of DAWN2 in Spain and have received fees from Novo Nordisk, S.A. for their participation in the coordination meetings of the panel. The authors have no additional conflicts of interest to declare.
The authors wish to thank Inés Hernando (Cociente S.L.) for her editorial support in the preparation of this manuscript, which was funded by Novo Nordisk S.A.
Sponsor: Novo Nordisk.
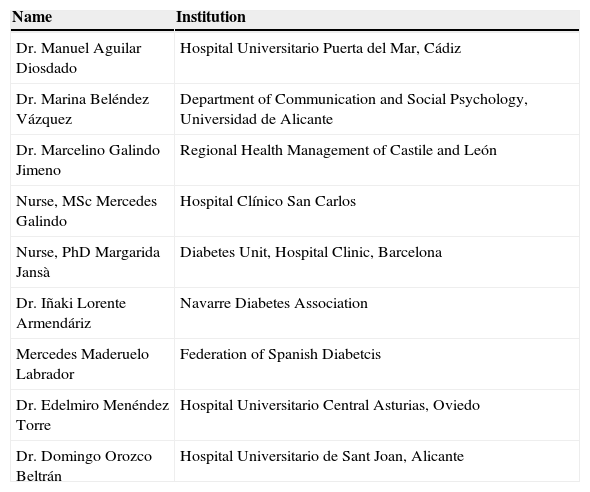
| Name | Institution |
|---|---|
| Dr. Manuel Aguilar Diosdado | Hospital Universitario Puerta del Mar, Cádiz |
| Dr. Marina Beléndez Vázquez | Department of Communication and Social Psychology, Universidad de Alicante |
| Dr. Marcelino Galindo Jimeno | Regional Health Management of Castile and León |
| Nurse, MSc Mercedes Galindo | Hospital Clínico San Carlos |
| Nurse, PhD Margarida Jansà | Diabetes Unit, Hospital Clinic, Barcelona |
| Dr. Iñaki Lorente Armendáriz | Navarre Diabetes Association |
| Mercedes Maderuelo Labrador | Federation of Spanish Diabetcis |
| Dr. Edelmiro Menéndez Torre | Hospital Universitario Central Asturias, Oviedo |
| Dr. Domingo Orozco Beltrán | Hospital Universitario de Sant Joan, Alicante |
Please cite this article as: Galindo Rubio M, Jansà Morató M, Menéndez Torre E, en nombre del Grupo DAWN2 España. Educación terapéutica y autocuidado: resultados del estudio observacional transversal Diabetes Attitudes, Wishes and Needs 2 (DAWN2) en España. Endocrinol Nutr. 2015;62:391–399.