The thyroid gland descends through the foramen cecum leaving an epithelialized tract called the thyroglossal duct, which disappears between the fifth and tenth weeks or pregnancy. The lack of involution of any part of the thyroglossal duct leads to the formation of thyroglossal cysts (TGCs).1 Most TGCs occur at or just below hyoid bone level. Approximately half the cases occur before 20 years of age.1 Evaluation is done using neck ultrasound, while computed tomography (CT) and magnetic resonance imaging are rarely required.2–5 Approximately 1% of TGCs contain malignant elements, and the most commonly reported primary tumor is papillary carcinoma, which emphasizes the need for resection.2–7 Fine needle aspiration (FNA) is the most precise method for preoperative diagnosis.3,4,7 The treatment recommended for these carcinomas is controversial, and the procedures used have ranged from a Sistrunk operation followed by thyroid hormone replacement therapy to total thyroidectomy with cervical dissection and iodine ablation therapy.2–7 Management should be individualized based on histological type, tumor invasiveness, and lymph node involvement. The prognosis of carcinoma derived from thyroglossal duct cysts is good, with a 10-year overall survival of 95%.2–7
The purpose of this letter is to report the case of a woman with metastatic papillary carcinoma derived from a thyroglossal cyst, an uncommon clinical condition.
A previously healthy 28-year-old female patient with no prior exposure to radiation and no family history of thyroid cancer consulted for a non-tender, mobile mass in the neck midline starting approximately 1.5 years before and steadily growing, particularly over the previous six months. A physical examination revealed a mass approximately 2.5cm in diameter of hard consistency, not adhering to deep planes, and mobile in the midline tract on tongue protrusion. The thyroid gland was of normal size and consistency, and no cervical adenopathies were palpated. The results of thyroid function tests and all other preoperative studies were normal. Ultrasound examination (US) and CT of the neck were consistent with thyroglossal cyst. FNA of the lesion, which is not routinely requested at our hospital, was not performed because of the presumed benign nature of the condition.
An elective Sistrunk procedure was performed to resect the whole thyroglossal duct cyst (approximately 3cm in diameter and soft) and the entire duct up to the base of the midportion of the hyoid bone. Based on the findings of preoperative studies, no exploration was made of the thyroid gland and lymph node chains, and no complications were reported.
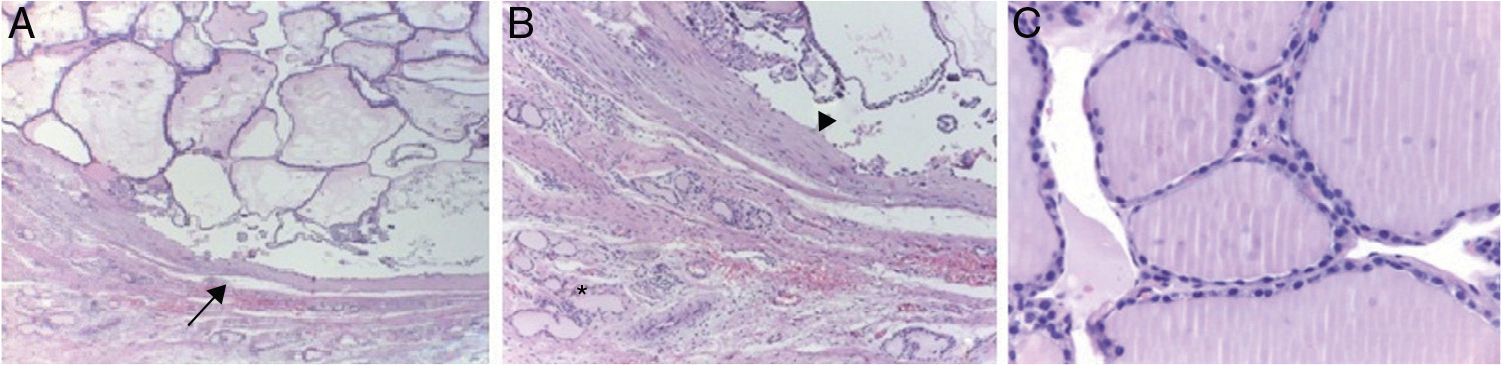
The final histopathological study revealed a surgical specimen 2.8cm in diameter containing papillary thyroid carcinoma, a wall free of neoplastic cells, and normal residual thyroid follicles at the periphery. A repeat neck US with an adenopathy scan showed an intact thyroid gland and bilateral lymph nodes in both jugular chains, with a mean diameter of 1cm, which were subject to US-guided FNA that led to a cytological result of papillary carcinoma metastases.
Repeat surgery, consisting of total thyroidectomy and modified, bilateral radical neck dissection, was decided upon, based on the foregoing. Postoperative recovery was successful, and hormone replacement with levothyroxine 100mcg daily (1.3mcg/kg/day) was subsequently started.
Histopathological examination of the surgical specimen revealed a microscopically normal thyroid gland and lymph nodes with metastases from moderately differentiated papillary carcinoma. The final diagnosis was primary papillary carcinoma derived from TGC (CaTGC) classified as T2 N1b M1, corresponding to stage II (Fig. 1). A whole body scan with 131I was negative, and the patient underwent ablation radiotherapy at doses of 100mCi approximately 10 weeks after final surgery.
Papillary carcinoma deriving from a thyroglossal duct cyst is very rare, and only approximately 260 cases have been reported in the literature since it was first described by Brentano in 1922.8 Diagnosis is difficult and usually incidental, because the clinical characteristics and preoperative imaging findings are not specific, and there is usually no elevation in the biochemical markers. This may have a direct impact on the planning of surgery. A preoperative diagnosis may be achieved through US-guided FNA in all adult patients with TGCs. A careful histological review of both the surgical specimen and associated adenopathies and the thyroid gland is mandatory, because nodal involvement has been reported in 40.5–75% of patients (with greater involvement of laterocervical compartments, approximately 60%),9,10 and concomitant papillary thyroid carcinoma in up to 61.5% of cases.9,10 However, only a few cases have been reported of primary CaTGC with cervical lymph node metastases leaving the thyroid gland free of disease. Despite multiple reviews of case series, it has not yet been possible to establish standard recommendations regarding the type of surgery and postoperative monitoring. Reports of new cases detailing the findings, treatment, and follow-up used should contribute substantially to unifying criteria in order to provide in a single intervention effective and minimally invasive treatments having a positive impact on the quality of life of affected patients.
Please cite this article as: Palomino Martínez BD, Beristain Hernández JL, Piscil Salazar MA, Villalpando Mendoza CJ, Velázquez García JA. Quiste tirogloso como foco primario de carcinoma papilar de tiroides metastásico a cadena ganglionar yugular. Endocrinol Nutr. 2014;61:e11–e12.