We report the case of a 40-year-old with an unremarkable clinical history seen for asymptomatic primary hyperparathyroidism. Palpation of thyroid gland and neck lymph node chains revealed no pathological findings.
Laboratory test results included a serum calcium level of 11.8mg/dL (normal range [NR], 8.5–10.5mg/dL), intact parathormone (PTH) 169pg/mL (NR, 15–69pg/mL), and a urinary calcium level of 342mg/24h. Bone densitometry (DEXA) showed a T score of −2.1 in the lumbar spine and −0.5 in the femoral head.
A preoperative localization study showed images consistent with left inferior and right inferior parathyroid adenoma (sestaMIBI scintigraphy) and multinodular goiter with two hypoechogenic nodular lesions in the left thyroid lobe 5 and 7mm in size respectively, and a 4mm hypoechogenic nodular lesion in the right thyroid lobe of a benign appearance and two posterior 6mm hypoechogenic lesions suggesting a parathyroid nature (thyroid scan).
Surgical exploration of the four parathyroid glands was performed through a Kocher cervicotomy followed by subtotal thyroidectomy combined with resection of both left inferior and right inferior parathyroid adenomas, as well as a potential right superior adenoma. The pathological study confirmed the presence of parathyroid hyperplasia, colloid nodular goiter, and chronic lymphocytic thyroiditis. Calcium and PTH levels normalized after surgery.
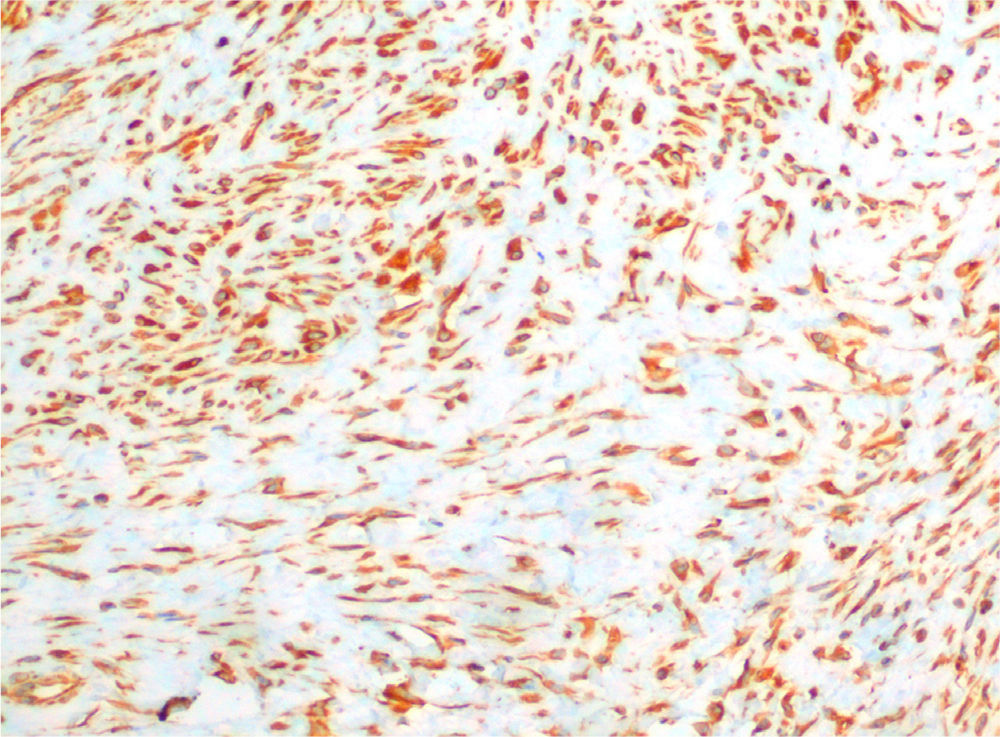
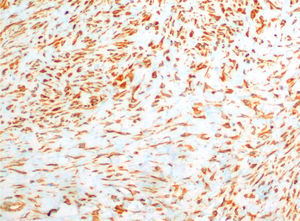
After surgery, the patient was seen for symptoms of dysphagia, and a neck ultrasound revealed a hypoechogenic nodular formation in the left thyroid lobe located in the posterior and caudal position, 14mm×11mm×14mm in cross-sectional, anteroposterior, and longitudinal diameter respectively, which could be interpreted as either thyroid or parathyroid tissue. Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) provided no adequate material for diagnosis. An additional EUS-FNA revealed striated muscle fibers, fibroblasts, and only a few follicular cells, and was again considered non-diagnostic. A third EUS-FNA was therefore scheduled, showing fusiform cells with wide cytoplasms on a proteinaceous striped background. Cytological diagnosis was musculoaponeurotic fibromatosis or nodular fasciits (NF). The imaging study was completed with a computed tomography (CT) scan of the neck and chest which showed an isodense 23mm×23mm×27mm tumor located between the distal insertion of the left hyoid muscles, with which it had no separation plane, and the anteroinferior margin of the lower thyroid lobe. The lesion showed well defined contours, with no calcium, fat, or significant enhancement with non-specific contrast. After consultation with the endocrine surgery department, resection by cervicotomy was decided upon and performed without complications. On gross examination, the surgical specimen was described as an irregular tissue fragment of elastic consistency with an approximate volume of 2mL. Microscopic examination found a mesenchymal lesion consisting of proliferated fibroblasts without cell atypia with a fusocellular arrangement on myxoid stroma and between muscle fascias, consistent with NF. Immunohistochemistry was positive for vimentin (Fig. 1).
Six months after surgery, neck ultrasound showed a 22mm×22mm recurrent lesion in the surgical bed which caused no compressive symptoms. Since size remained stable, conservative management and regular ultrasonographic monitoring was decided upon after three months of postoperative follow-up.
The description of NF in thyroid bed related to thyroid/parathyroid surgery is exceptional and has not been reported to date. NF, also called pseudosarcomatous fibromatosis and proliferative or pseudosarcomatous fasciits, is a benign tumor derived from fibrous tissue described by Konwaler et al. in 1955.1 It usually occurs as a single, round tumor located subcutaneously. It may, however, occur in dermis, deep fascia, and skeletal muscle, and even intravascularly, adjacent to the skull, intra-articularly, and around the serous surface of the small bowel, urinary bladder, and gallbladder.2,3 NF most commonly occurs in the upper limbs, specifically in the volar aspect of the forearm (46% of cases), followed by the trunk (20%), head and neck (18%), and lower limbs (15%).3,4 Patients aged 20–40years old are mainly affected, but cases occurring at extreme ages have also been reported.5
Its etiology is uncertain. Although a clear association with recent trauma is occasionally found, this is not true in most cases. Clonal chromosomal abnormalities recently documented in a small number of cases suggest that it may represent a myofibroblastic tumor.5 The finding of this at the site of a tick bite which contained ribonucleic acid specific to Borrelia afzelii suggests a potential infectious etiology.6,7 Based on the presence of estrogen receptors in tumor cells, it is suggested that pregnancy could induce proliferative changes in fibroblasts7 which represent a risk factor for the development of the condition.
Clinically, NF appears as a firm, rapidly growing, hard, circumscribed tumor, not encapsulated and usually painless. Size does not usually exceed 4cm in largest diameter at diagnosis. NF has no specific radiographic characteristics, appearing in CT as a hyperdense, homogeneous lesion, and in magnetic resonance imaging as a T2 hyperintense lesion.
FNA may be helpful as an initial approach to diagnosis. Because of the need to rule out a sarcomatous lesion, resection and histological examination are recommended.7,8 The most striking cytological features include the presence of fusiform cells with wide, clear cytoplasms, nuclear irregularities, inconspicuous nucleoli, and mitotic figures, immersed in a hematic, myxoid stroma, and cellular proteinaceous background. Some lymphocytes, polimorphonuclear cells, and macrophages also occur among fusiform cells forming S-shaped groups. Histological indicators characteristic of malignant tumors may sometimes be found, including cell atypia, high cellularity, and mitoses, an infiltrating growth pattern, and necrosis, which often lead to interpretation errors and allows for the including of NF in the group of pseudosarcomatous lesions.6–9 Immunohistochemistry is essential for differential diagnosis with these lesions and with malignant tumors such as fibrosarcoma, malignant fibrohistiocytoma, neurofibrosarcoma, and myxoid dermatofibroma protuberans.8,9 Thus, NF is negative for CD-34, which rules out a sarcomatous origin, and also for protein S-100, caldesmin, desmin, trypsin, factor viii, and HLA-DR, but positive for vimentin and smooth muscle actin.9
Treatment of choice is local surgical resection. Although NF is a benign condition, it has a 7% recurrence rate, and clinical and ultrasonographic follow-up is therefore required.10
Please cite this article as: Jiménez Varo I, Luján Rodríguez D, Romero Lluch AR, Guerrero Vázquez R, Martínez-Brocca MA. Fascitis nodular tras paratiroidectomía. Endocrinol Nutr. 2014;61:e13–e14.