Thyroid abscess is rare in children but the presence of previous thyroid disease, and congenital remnants such as a pyriform sinus fistula, are predisposing factors. The classical presentation consists of fever, cervical pain and a painful mass. The diagnosis is confirmed through clinical findings, and by diagnostic imaging (ultrasound and computerized axial tomography). A barium swallow must be performed in order to detect a fistula and to consider surgical drain. We present the cases of thyroid abscess in five patients who were admitted in four medical centers (Fundación Cardioinfantil, Hospital Universitario San Ignacio, Clínica infantil de Colsubsidio and Hospital de la Misericordia) in Bogotá, Colombia between 2000 and 2010.
La formación de absceso tiroideo es una patología rara en niños; sin embargo, la enfermedad de tiroides previa, remanentes congénitos como fístula de seno piriforme son factores predisponentes. La presentación clásica consiste en fiebre, dolor cervical y sensación de masa dolorosa (frecuentemente izquierda) del lóbulo tiroideo. El diagnóstico se confirma por hallazgos clínicos, ecográficos, tomografía computarizada (TC). Se debe realizar un esofagograma para descartar la presencia de fístula y considerar el drenaje quirúrgico en los casos que lo ameriten. Se presentan los casos de absceso tiroideo en 5 pacientes que ingresaron en cuatro centros médicos (Fundación Cardioinfantil, al Hospital Universitario San Ignacio, a la Clínica infantil de Colsubsidio y al Hospital de la Misericordia) de Bogotá, Colombia, entre los años 2000 y 2010.
Acute suppurative thyroiditis is an uncommon condition in children. Progression to abscess formation is even rarer because the anatomical and physiological characteristics of the thyroid gland protect it against infection. Such characteristics include its fibrous capsule, high iodine levels, extensive vascularization, lymphatic drainage, and separation of the gland from other cervical structures by fascial planes in the neck.1 However, pre-existent thyroid disease, the persistence of a thyroglossal duct remnant, trauma, or a piriform fistula predispose immunocompetent patients to experience this disease. Although this is an uncommon emergency in the pediatric population, diagnosis is confused when it occurs, and it is initially managed as a deep cervical infection. The search for the cause and subsequent management are also fraught with problems.
Different literature reviews report in recurrent cases congenital defects such as persistent piriform sinus, remnants of the third and fourth branchial arches, and immune states that facilitate the progression of this rare inflammation. Diagnosis is based on clinical, laboratory, and imaging findings. The abscess typically occurs on the left side, and it is important to differentiate acute thyroiditis from the more common subacute thyroiditis. Five patients with this unusual condition are reported below, including their clinical and paraclinical (imaging and laboratory tests) characteristics and the treatment given.
Patients and methodsA report on cases seen in patients from four hospitals in Bogotá (Colombia) from January 2000 to April 2010.
Case 1A male patient aged 6 years and 2 months was admitted for pain starting 3 days before in the neck area and swelling mainly on the left side, with a temperature of 39°C, intermittent bitemporal headache, odynophagia, hyporexia, and left ear pain with no discharge. The patient had been seen for a similar episode 20 days previously.
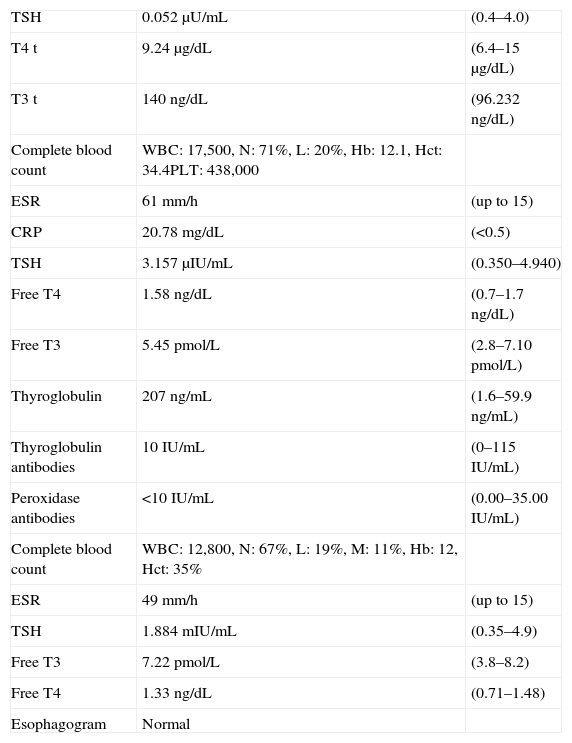
The results of initial serum laboratory tests are shown in Table 1. Thyroid ultrasound examination revealed a right thyroid lobe 28mm×14mm×11mm in size with a simple cyst, and a left thyroid lobe 28mm×13mm×12mm in size with a thyroid nodule. A thyroid scan was therefore performed with technetium 131 as a radiotracer, and was reported as showing poor visualization of the thyroid gland due to potential hypofunction versus subacute thyroiditis.
Baseline and follow-up laboratory data for case 1. Reference ranges are shown on the right side of the table.
| TSH | 0.052μU/mL | (0.4–4.0) |
| T4 t | 9.24μg/dL | (6.4–15μg/dL) |
| T3 t | 140ng/dL | (96.232ng/dL) |
| Complete blood count | WBC: 17,500, N: 71%, L: 20%, Hb: 12.1, Hct: 34.4PLT: 438,000 | |
| ESR | 61mm/h | (up to 15) |
| CRP | 20.78mg/dL | (<0.5) |
| TSH | 3.157μIU/mL | (0.350–4.940) |
| Free T4 | 1.58ng/dL | (0.7–1.7ng/dL) |
| Free T3 | 5.45pmol/L | (2.8–7.10pmol/L) |
| Thyroglobulin | 207ng/mL | (1.6–59.9ng/mL) |
| Thyroglobulin antibodies | 10IU/mL | (0–115IU/mL) |
| Peroxidase antibodies | <10IU/mL | (0.00–35.00IU/mL) |
| Complete blood count | WBC: 12,800, N: 67%, L: 19%, M: 11%, Hb: 12, Hct: 35% | |
| ESR | 49mm/h | (up to 15) |
| TSH | 1.884mIU/mL | (0.35–4.9) |
| Free T3 | 7.22pmol/L | (3.8–8.2) |
| Free T4 | 1.33ng/dL | (0.71–1.48) |
| Esophagogram | Normal |
Hb: hemoglobin; Hct: hematocrit; L: lymphocytes; N: neutrophils; M: monocytes.
Based on these findings, outpatient management with cefadroxil was decided upon. Five days later, the patient returned due to the persistence and exacerbation of the initial picture, occasional headache, and a sensation of tachycardia. Physical examination found a heart rate (HR) of 160bpm, respiratory frequency (RF) of 28/min, and blood pressure (BP) of 68mmHg, a weight of 18.2kg, a height of 111cm, mucocutaneous pallor, thyroid gland enlargement, tenderness, hyperdynamic and tachycardiac precordium, protomesosystolic murmur, normal abdomen, and good distal perfusion. Control laboratory data were obtained (see Table 2).
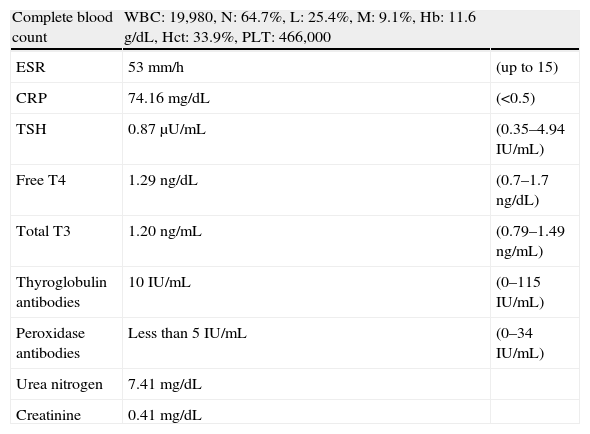
Laboratory data for case 2. Reference ranges are shown on the right side of the table.
| Complete blood count | WBC: 19,980, N: 64.7%, L: 25.4%, M: 9.1%, Hb: 11.6g/dL, Hct: 33.9%, PLT: 466,000 | |
| ESR | 53mm/h | (up to 15) |
| CRP | 74.16mg/dL | (<0.5) |
| TSH | 0.87μU/mL | (0.35–4.94IU/mL) |
| Free T4 | 1.29ng/dL | (0.7–1.7ng/dL) |
| Total T3 | 1.20ng/mL | (0.79–1.49ng/mL) |
| Thyroglobulin antibodies | 10IU/mL | (0–115IU/mL) |
| Peroxidase antibodies | Less than 5IU/mL | (0–34IU/mL) |
| Urea nitrogen | 7.41mg/dL | |
| Creatinine | 0.41mg/dL |
Hb: hemoglobin; Hct: hematocrit; L: lymphocytes; M: monocytes; N: neutrophils; CRP: C-reactive protein; T3: triiodothyronine; T4: thyroxine; TSH: thyroid-stimulating hormone; ESR: erythrocyte sedimentation rate.
An additional thyroid ultrasound showed a right thyroid lobe 26mm×10mm×7mm in size, with a volume of 1.5mL, with a simple cyst 6mm in diameter in the lower third ultrasonographically normal, and an enlarged left thyroid lobe 40mm×27mm×20mm in size in which a heterogeneous, ill-defined, echogenic, solid mass with increased color doppler flow, approximately 38mm×26mm×17mm in size, that displaced laterally to the carotid and jugular arteries was identified. The radiological report suggested thyroiditis of infectious and bacterial origin as the first possibility, but did not rule out a neoplasm. Enlarged nodes 8–12mm in size were also reported in cervical areas IIA, IIB, III, and IV. The patient was examined by pediatric surgery, which requested a CT scan of the neck to define the need for biopsy. A CT report described a heterogeneous mass related to the left thyroid lobe whose enhancement pattern suggested an abscess-like component and a probable inflammatory etiology. The mass measured 31mm×21mm in the axial plane and 38mm in the coronal plane. However, the involvement of the adjacent thyroid parenchyma suggested a less likely differential diagnosis of primary neoplastic involvement. Adenomegalies were also seen in areas IIA-B, III, and IV with a mass effect on the airway, with mild deviation to the right and lateral displacement of the carotid space.
The patient continued to experience febrile peaks and inflammatory signs at the anterior cervical level. Based on clinical and laboratory findings and on the clinical course, a thyroid abscess was diagnosed, and treatment was started with propranolol 10mg every 12h and antibiotic coverage with ampicillin/sulbactam at a dose of 200mg/kg. This treatment achieved a clinical improvement, pain relief, and an improvement in the cervical range of motion. Thyroid palpation found decreased edema, although the left lobe continued to be enlarged, but not tender. After seven days of antibiotic treatment, the patient was discharged and propranolol was discontinued.
The patient returned to the outpatient clinic 15 days after discharge and was found to be symptom-free. At the physical examination, the thyroid gland continued to be enlarged at the expense of the left lobe, with persistent homogeneous consistency and nonpalpable nodes. The right thyroid lobe was not palpated. Control laboratory test results were available (see Table 1). A control CT scan of the neck showed a small anterior mass in the left anterolateral soft tissues, in addition to multiple nodes at suprahyoid and infrahyoid internal jugular levels II and III.
Case 2A female patient aged 3 years and 5 months was referred by pediatric endocrinology for suspected thyroiditis. For the previous month, she had experienced upper respiratory symptoms caused by odynophagia, right ear pain, dysphagia, rhinorrhea, and fever up to 38°C. The patient had been treated outside the hospital for viral rhinopharyngitis with no improvement. She was seen again due to symptom persistence and high temperature, and a single dose of intramuscular benzathine penicillin, acetaminophen, and loratadine were prescribed. Subsequently, the patient experienced increased dysphagia, odynophagia, a loss of 5kg of weight in one month, and the occurrence of a mass in the neck, for which she was seen again days later at another center where a thyroid ultrasound examination revealed a generalized enlargement of the left thyroid lobe and isthmus, heterogeneous echogenicity with hypoechoic areas mainly in the central area, a diameter of 40mm×20mm×23mm, an isthmus of 12.5mm, and a normal right lobe 30mm×10mm×5mm in size, as well as adenomegalies. A complete blood count was also performed, and acute phase reactants were measured (see Table 3), and the patient was referred to our hospital to be assessed by the pediatric endocrinology department. Upon admission, the patient had tachycardia (HR, 124bpm) and a thyroid mass 3cm×4cm in size was found which was tender, soft in consistency, ill-defined, warm, and adherent to deep planes. Grade IV tonsillar hypertrophy and strong halitosis were also found. A CT scan of the neck with contrast showed an inflammatory process affecting the left thyroid lobe with cystic areas inside, suggesting an abscess, and extending behind the larynx to the prevertebral thyroid space. The left thyroid lobe measured 31mm×24mm×22mm. The thyroid profile and antithyroid antibodies were normal (see Table 2). Oxacillin 100mg/kg/day and amikacin 15mg/kg/day were started. The patient did not respond to antibiotic therapy, showing persistent febrile peaks. At the otolaryngology department, a hard mass with well defined margins and slightly tender, 7cm×bcm in size in the left neck region was found. The mass remained fixed during swallowing, with no tongue protrusion, and a thyroglossal cyst was therefore ruled out. Scintigraphy with technetium 131 showed findings consistent with an acute inflammatory process diffusely compromising the thyroid gland, of which only the right upper pole was defined. The patient continued to have febrile peaks with no decrease in mass size. Based on the suspicion of a thyroid abscess, broader antibiotic coverage for anaerobes was prescribed, amikacin was discontinued and replaced by clindamycin at a dose of 30mg/kg/day. Supplemental tests to rule out the presence of malformations (persistent piriform sinus) were requested.
A slow clinical improvement occurred, with mass size decreasing to 4cm×3cm. A subsequent naso/sinuscopy showed a nasopharynx with a normal appearance, an edema, and interarytenoid erythema, and a discharge of a purulent secretion from the left piriform sinus. The condition was considered to be consistent with the sinus of the third branchial cleft versus an abnormality of the third branchial arch which warranted surgical exploration with laryngeal microendoscopy, rigid bronchoscopy, and piriform sinus exploration plus fistulography with contrast medium. At surgery, performed by the otolaryngology department, an edema was found at the level of the left piriform sinus, with no secretion or masses and without extrinsic compression.
The clinical course was adequate, with a decrease in cervical mass size. A control ultrasound showed a resolving thyroid abscess and normal esophagogram. Pediatric surgery therefore decided to complete medical management and not perform puncture or biopsy. After 19 days on amoxacillin and 11 days on clindamycin, the patient was discharged on amoxacillin-clavulanate for 5 days and follow-up by the outpatient clinic with thyroid profile and control ultrasound examinations.
Diagnosis at discharge: a resolving left thyroid abscess, a fistula in the left piriform sinus, and suspected persistence of the third or fourth left branchial arch.
Case 3A 9-month-old male patient was seen for daily fever up to 39°C associated with emesis and diarrheal stools for the previous 3 days. A physical examination revealed grade I dehydration, HR of 184bpm, RF of 60/min, 39°C of temperature (T), and a weight of 8.2kg. The patient was thought to be suffering from gastroenteritis, with signs of dehydration and a toxic appearance, and was therefore admitted to hospital. On the second day, bilateral painful cervical swelling limiting lateral movements of the neck was noted. The results of the tests performed (complete blood count, electrolytes, partial urine analysis, and coproscopy) were normal. Antibiotic therapy consisting of oxacillin 100mg/kg/day and gentamicin 7.5mg/kg/day was started, and blood cultures were requested. Ultrasound examination of the neck showed cervical adenitis with multiple adenomegalies in the right cervical chains with no abscess and normal thyroid lobes. After 72h of antibiotic therapy, the patient still had febrile peaks, a toxic appearance, generalized mucocutaneous pallor, restricted neck motion, and an enlargement of the nodes in the bilateral cervical chains with no signs of fistula or abscess formation. Blood cultures for common pathogens, acid-fast bacilli (AFB), and slow growers were negative. A repeat ultrasound examination showed adenomegalies of 8 and 14mm in the internal lateral chains on both sides and a right thyroid lobe with ill-defined contours and a 13-mm echoic fluid collection. Acute thyroiditis was diagnosed versus a fluid collection in the right thyroid lobe, and a thyroid profile was therefore requested (see Table 3).
A CT scan of the neck with contrast revealed a fluid collection extending from the nasopharynx to the cervical area. The pediatric surgery department performed direct endoscopy which showed findings consistent with erythema in the posterior wall with no abscess, no elastic area, or foreign body, with an easy passage of the endoscope into the esophagus and no pharyngeal bulging. Based on the findings and clinical course of the patient, a thyroid abscess was diagnosed and coverage was started for anaerobes and staphylococci. Antibiotic therapy was switched to clindamycin 30mg/kg/day and metronidazole 30mg/kg/day.
Antibiotic therapy was administered for 10 days with a satisfactory clinical response. A control CT scan showed resolution of the collection in the retropharyngeal space with no image suggesting a congenital lesion. Thyroid hormone levels had normalized.
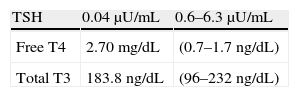
Case 4A female patient aged 13 years and 3 months was seen for pain on the anterior side of the neck over the previous 2 days and fever for the previous 24h. Her prior history was unremarkable. Vital signs in the initial physical examination included BP of 110/60, HR of 92bpm, and a temperature of 38.2°C. Her pharynx and tonsils were highly congestive, and a timpanoscopy was normal. Neck palpation was difficult due to pain and stiffness. Local warmth was found, and there were no changes in skin appearance or regional adenopathies. Table 4 shows the results of baseline laboratory tests. Blood cultures were taken for common pathogens, acid-fast bacilli, and slow growers. Thyroid ultrasound examination could not be performed due to neck sensitivity. A thyroid abscess was suspected, and treatment was started with oral dicloxacillin, 1g every 6h, and acetaminophen. The patient showed clinical improvement from the fourth day of treatment, and the 10-day cycle of antibiotic therapy was completed. Blood culture results were negative, and a biopsy was not considered necessary.
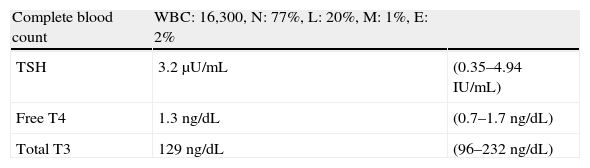
Laboratory data for case 4. Reference ranges are shown on the right side of the table.
| Complete blood count | WBC: 16,300, N: 77%, L: 20%, M: 1%, E: 2% | |
| TSH | 3.2μU/mL | (0.35–4.94IU/mL) |
| Free T4 | 1.3ng/dL | (0.7–1.7ng/dL) |
| Total T3 | 129ng/dL | (96–232ng/dL) |
E: eosinophils; L: lymphocytes; M: monocytes; N: neutrophils; T3: triiodothyronine; T4: thyroxine; TSH: thyroid-stimulating hormone.
A female patient aged 14 years and 8 months was seen for neck pain, hyporexia, nausea, a mass in the anterior neck region and a temperature of 39.5°C over the previous 2 days. She had experienced a similar episode, which resolved with medical treatment, 8 months before. A physical examination revealed normal weight and height for age, a toxic appearance with BP of 90/55, HR of 100bpm, T of 39.1°C, and dry oral mucosa. A hard mass, probably dependent on the thyroid and tender was noted in the anterior side of the neck. No skin changes were seen. The patient also had neck stiffness and regional adenopathies. The pharynx and tonsils were congested, but there was no exudate. Tooth decay was seen in two molar teeth. The patient was admitted to hospital and administered intravenous fluids, cefalotin 1g every 4h, and antipyretics. Laboratory tests showed 14,500 WBCs at the expense of neutrophils (81%). Two blood cultures were taken with negative results. Magnetic resonance imaging with and without contrast showed no fistula, and revealed a 4cm×5cm abscess encapsulated in the right thyroid lobe.
On the third day of her hospital stay, flushing, warmth, and smooth skin appeared in the right anterolateral region of the neck. The lesion was punctured, yielding a small amount of purulent material. Culture of this material was negative for common pathogens, acid-fast bacilli, and slow growers. The patient experienced an improvement from the fifth day of her hospital stay with the prescribed treatment.
DiscussionSuppurative thyroiditis is uncommon in children, and thyroid abscess is even rarer. Until 1997, only 60 cases had been reported in pediatric patients, 18 of which had recurred.2 Two additional cases had been reported by 2001, and cases have occasionally been reported in newborns. Our understanding and experience of the course and management of this condition is therefore poor. In addition, no data are available about the prevalence of this condition in our region. This article reports 5 cases seen from January 2000 to April 2010 at 4 hospitals in the city of Bogotá (Colombia, South America).
Incidence is difficult to assess because of the rarity of the disease. Hazard et al. reported that the condition was more common among women aged 20–40 years,1 while reviews by Yu et al. and Berger et al. found similar rates in both sexes.1 As regards age ranges, cases are usually reported from 16 months to 77 years of age. The condition is more common in immunocompromised patients, patients receiving chemotherapy or steroids, or after transplantation.1 Our reported cases occurred in previously healthy subjects with an initial viral infection and ages ranging from 9 months to 14 years and 4 months.
In children, a thyroid abscess occurs in most cases as a complication of a hypopharyngeal fistula.1 However, other causes of suppuration should be suspected, including direct trauma, a foreign body, hematogenous dissemination, or tuberculosis,3 the latter being more frequent in adults. An impaired immune function may play a significant role.4 However, the immune status of these patients was not analyzed because they were previously healthy children with no history of recurrent infection or with any previous data leading it to be suspected. Literature reviews suggest the possibility that the immune system is negatively influenced by infections such as mononucleosis some months before the abscess occurs.4
As stated above, acute suppurative thyroiditis with abscess formation is uncommon, particularly in pediatric patients. However, pre-existent thyroid disease, the persistence of a thyroglossal duct remnant, trauma, or a piriform sinus fistula predispose patients to thyroid infection.5
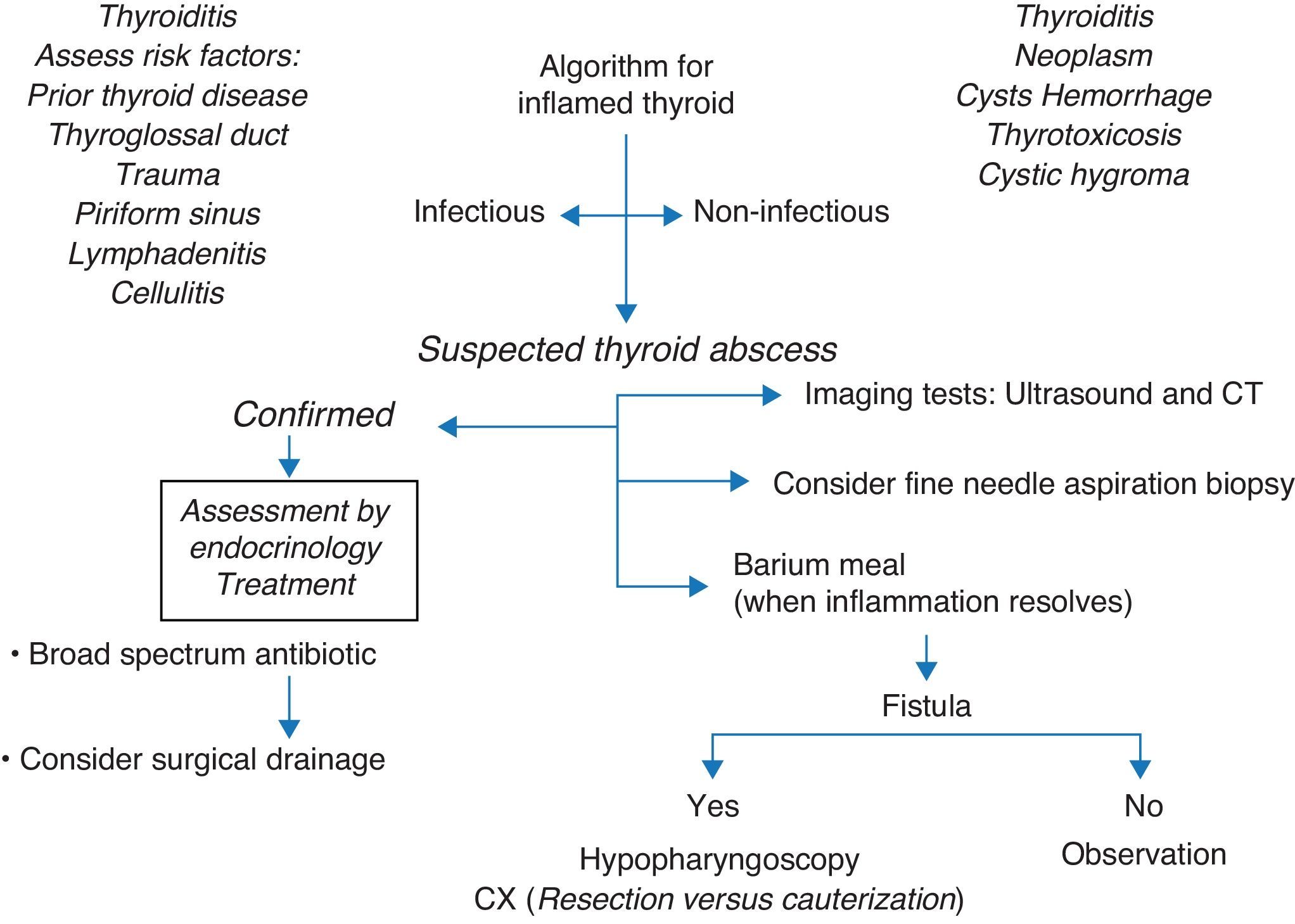
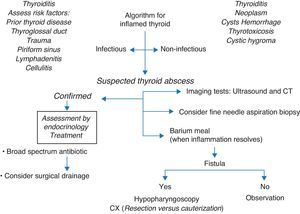
When this diagnosis is suspected, different imaging tests may be performed for definitive diagnosis. Ultrasound examination differentiates between solid and cystic masses and may detect the inflammation of gas around the thyroid gland. A CT scan may allow for the identification of inflammatory changes and abscess formation, and also of a fistula (a tract with air).6–8 Although an esophagogram makes it possible for the presence of a fistula to be demonstrated, this should only be performed after the infection has resolved.6,9,10 Otherwise, a false normal result may be obtained. This would explain the absence of changes in the esophagogram from our patient reported as case 2. Hypopharyngoscopy is an ideal procedure for diagnostic accuracy; Houghton et al. recommend ultrasound-guided fine needle aspiration, particularly if the collection is localized.11 There are times when this cannot be performed before antibiotic therapy is started, as occurred in the cases reported here. In our patients undergoing an esophagogram, this was normal. However, the infection was not fully controlled in all of them, as stated above. The persistence of piriform sinus, diagnosed by hypopharyngoscopy, could be shown in the second case. This fistula acts as a duct to disseminate microorganisms from the pharynx to the perithyroid space and thyroid gland.12 Its usual presentation signs include suppuration and/or cervical abscesses or left suppurative thyroiditis. However, patients may be symptom-free for long time periods. Literature reviews suggest that it corresponds to remnants of the third and fourth branchial arches. The fistula of the fourth branchial is caused by the persistence of the pharyngobranchial duct and communicates the pharynx to the upper thyroid pole.
Differentiation of abnormalities of the third or fourth branchial arches is difficult, and may only be performed during surgery.13 The tract has mucosa, which may be inflamed. If not closed, recurrent infections may occur. In patients with left thyroid abscess, the presence of piriform sinus tract should always be ruled out.
Similarly to what occurred in our patients, the clinical characteristics reported in the literature usually appear after an upper respiratory or pharyngeal event or middle ear infection and include fever, odynophagia, anterior neck swelling, erythema, dysphagia, hoarseness, and restricted head motion.1 The condition may also be suspected when a foreign body is found.14 Increased local sensitivity suggests an inflammatory or hemorrhagic process inside the gland. Tachycardia and leukocytosis are common findings. A diagnosis of thyroid abscess was not made initially in any of the cases reported here because of its low frequency in children, despite the presence of many of these characteristics.
As regards thyroid function, Kawanaka et al. in 1994,15 Meier and Nagle in 1996,16 and other authors reported thyroid hormone levels that may mimic hyperthyroid states, with increases in both free and total T4 and TSH suppression.4 This was shown in cases 1 and 3, where high total T4 levels were found. In case 3, thyroid function improved with the resolution of the infection.
Differential diagnosis of thyroid inflammation includes thyroiditis (acute, subacute, or chronic), carcinoma, branchial cleft cyst, thymus cyst, cellulitis, hemorrhagic thyroid cyst, thyroid abscess, thyrotoxicosis, cystic hygroma, inflamed thyroglossal duct, or cervical lymphadenitis,11,14,17 as well as Pneumocystis carinii infection and/or infarction of a thyroid lobe.1
In cases where microbiological studies were performed, no germs were isolated. However, literature reviews report common oropharyngeal flora from the upper respiratory tract that enters the perithyroid spaces and thyroid gland through congenital remnants and/or fistulas. Other commonly involved germs include hemolytic streptococci, Staphylococcus aureus, and pneumococci, as well as anaerobic and Gram-negative bacteria.18Acinetobacter, Mycobacterium, Coccidioides, Pseudomonas, Salmonella, Eikenella, Clostridium, Nocardia, Pneumocystis carinii, Haemophilus, and Candida isolates have been reported in immunocompromised patients.2,19–21
The literature discusses the management, including parenteral broad spectrum antibiotics and surgical drainage, of those patients who do not adequately respond to extended spectrum antibiotic therapy22 in order to ensure antibiotic coverage for typical microorganisms such as staphylococci, pneumococci, streptococci, and anaerobes.2,19–21 Surgery is delayed until the infection is resolved. Surgical excision of cysts, tracts and/or fistulas is the standard treatment described in the literature.21 Thyroid lobectomy with isthmus resection should preserve the recurrent laryngeal nerve and may decrease the risk of recurrence. Endoscopic cauterization with silver nitrate has been shown to be a safe, effective procedure for the treatment of cleft sinuses.6,23,24 None of our reported cases required surgery.
Complications of these infections include abscess rupture, sepsis, extension to the pharynx, neck, or mediastinum, or airway involvement.6,19 No complication occurred in any or our cases. Minhas et al. reported patients with left vocal cord palsy who required tracheostomy due to airway compromise.6,7
ConclusionsThyroid abscess is a rare condition in children, and its low prevalence delays diagnosis. In all the cases reported here, the abscess was preceded by infectious conditions, the first episode being suppurative thyroiditis. No changes were seen in the esophagogram in any case, and a piriform sinus fistula was shown by hypopharyngoscopy in a single patient. The assessment of anatomical abnormalities and the monitoring of images once the inflammatory process has been resolved is required, especially if it is recurrent or appears in very young patients. If the condition is suspected, ultrasound-guided fine needle aspiration biopsy allows for early differential diagnosis, as does surgical drainage, if needed. In addition, the adequate use of antibiotics ensures a better prognosis.
When a tender mass in the neck is seen associated with febrile peaks, it is mandatory to suspect thyroid abscess as a differential diagnosis in order that adequate work-up and antibiotic management can be performed. For this reason, we have considered it important to disseminate these cases to the pediatric community (Fig. 1).
Conflicts of interestThe authors state that they have no conflicts of interest.
Please, cite this article as: Céspedes C, et al. Absceso tiroideo. Serie de casos y revisión de la literatura. Endocrinol Nutr. 2013;60:190–6.