Thyroid hemiagenesis is a highly uncommon congenital abnormality, as attested by the fact that only approximately 300 cases had been reported up to 2010.1 Thyroid hemiagenesis is defined as the lack of development of one thyroid lobe or one thyroid lobe and thyroid isthmus, and was first reported by Handsfield-Jones in 1866. Its prevalence in the general population, estimated from screening ultrasound studies in different countries, is approximately 0.06% (ranging from 0.05% to 0.2%), with left thyroid lobe agenesis being more common.2–4
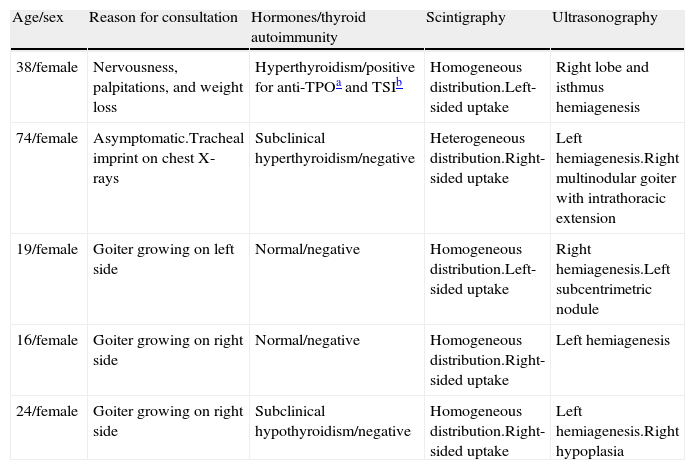
The clinical and imaging characteristics of five patients with thyroid agenesis attending our clinic from 1997 to 2006 due to the occurrence of documented or radiographically suspected goiter (4/5) or clinical signs of hyperthyroidism (1/5) are summarized below in Table 1. Diagnosis was therefore incidentally made in all cases in the setting of studies prompted by another thyroid condition because hemiagenesis itself did not induce any symptoms.
Clinical characteristics and results of imaging tests in five patients with thyroid hemiagenesis.
| Age/sex | Reason for consultation | Hormones/thyroid autoimmunity | Scintigraphy | Ultrasonography |
| 38/female | Nervousness, palpitations, and weight loss | Hyperthyroidism/positive for anti-TPOa and TSIb | Homogeneous distribution.Left-sided uptake | Right lobe and isthmus hemiagenesis |
| 74/female | Asymptomatic.Tracheal imprint on chest X-rays | Subclinical hyperthyroidism/negative | Heterogeneous distribution.Right-sided uptake | Left hemiagenesis.Right multinodular goiter with intrathoracic extension |
| 19/female | Goiter growing on left side | Normal/negative | Homogeneous distribution.Left-sided uptake | Right hemiagenesis.Left subcentrimetric nodule |
| 16/female | Goiter growing on right side | Normal/negative | Homogeneous distribution.Right-sided uptake | Left hemiagenesis |
| 24/female | Goiter growing on right side | Subclinical hypothyroidism/negative | Homogeneous distribution.Right-sided uptake | Left hemiagenesis.Right hypoplasia |
This abnormality has traditionally been considered to be more prevalent in women, with a 3:1 female to male ratio.2 The accuracy of this statement however is debatable because thyroid gland disease is overall more prevalent in females as compared to males, and the assumed higher frequency of cases detected in female patients could be a selection bias. This potential bias is also supported by systematic ultrasound studies conducted on non-selected populations providing different results, including even higher prevalence rates of hemiagenesis in males as compared to females.3 The higher frequency of hemiagenesis of the left lobe, absent in 80% of the reported cases and associated with isthmus agenesis in 50% of these patients, should particularly be noted.2–4
As previously mentioned, thyroid hemiagenesis does not cause any symptoms and is an incidental finding in the setting of another thyroid disease: there are reports in the literature of cases of hemiagenesis in congenital hypothyroidism, hyperthyroidism due to Graves-Basedow disease, hypothyroidism due to autoimmune thyroid disease, simple or nodular goiter, adenoma, and thyroid carcinomas.5,6 Our patients reflect this wide spectrum of presentations, so that we report a new case of Graves-Basedow disease, a case each of pretoxic and euthyroid nodular goiter, a case associated with simple euthyroid goiter and, finally, a case with subclinical hypothyroidism and negative thyroid autoimmunity.
As regards laboratory tests, thyroid stimulating hormone (TSH) levels, although within normal limits, are significantly higher in subjects with thyroid hemiagenesis as compared to healthy controls. These findings, probably related to the need for a greater stimulus by TSH on the thyroid remnant in order to ensure optimal hormone production, result in a compensatory hypertrophy which, when sustained over time in predisposed subjects, appears to be responsible for the greater prevalence of autoimmune thyroid disease and nodular goiter in patients with thyroid hemiagenesis as compared to subjects with complete gland development.7 Long-term monitoring of these patients is therefore advisable.
Little is known about the pathophysiological mechanisms responsible. Thus, it is not known whether the underlying event is an impaired descent of the gland along the thyroglossal tract or an absence of lobulation once the gland has reached its final position. There is however evidence suggesting a possible genetic basis, as cases of clear familial clustering have been reported.7
Thyroid development and gland migration from the pharyngeal floor depend on the interrelationship of different transcription factors including TTF-1, FOXE-1 (TTF-2), and PAX-8. Castanet et al. studied 22 patients with thyroid hemiagenesis finding no PAX-8 mutations, and as regards the FOXE-1 gene, the polymorphic variants with a higher number of alanine repeats could be associated with familial but not sporadic forms of hemiagenesis. On the other hand, TTF-2 mutations, while associated with syndromic congenital hypothyroidism, do not appear to be involved in thyroid hemiagenesis.7,8
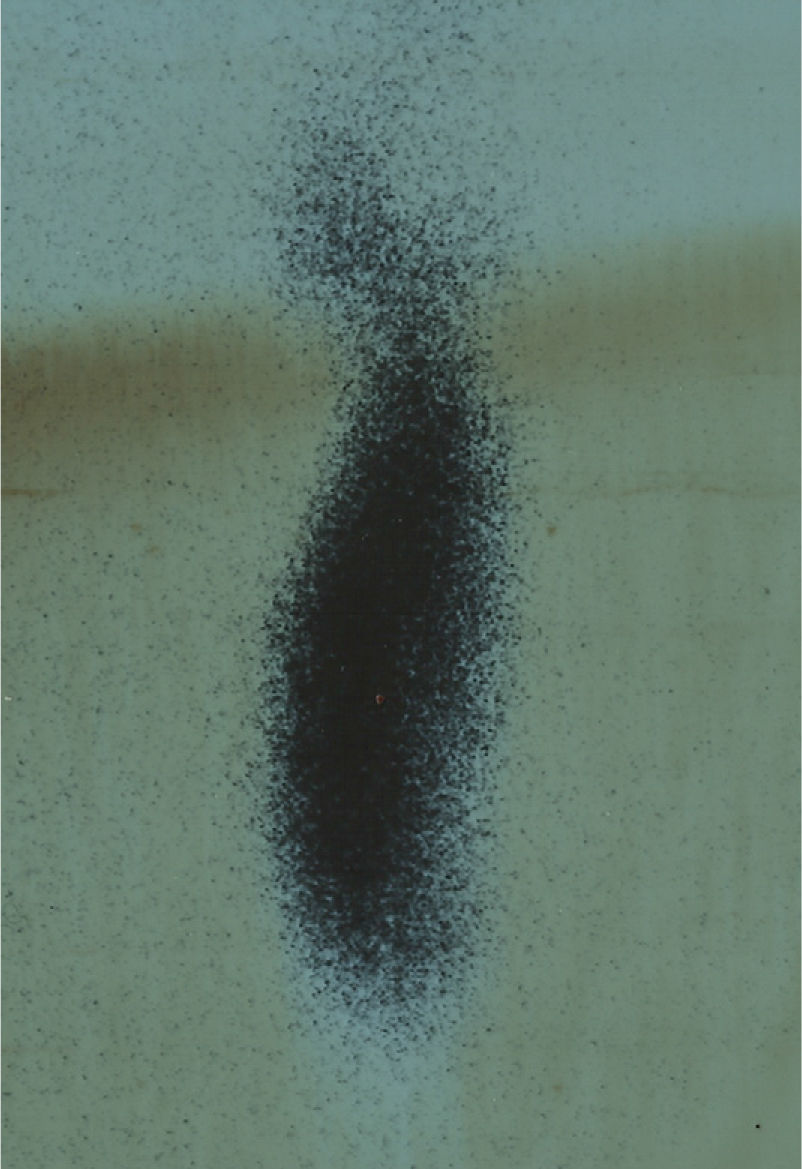
A presumed diagnosis may be made based on a thyroid scintigraphy showing the accumulation of the radiotracer in a single thyroid lobe, causing the so-called hockey stick sign when the thyroid isthmus is present.9Fig. 1 shows a scintigraphic image from one of our patients with a homogeneous deposit of radiotracer in the left thyroid lobe and a total absence of uptake by the right half of the gland. However, this image should be interpreted with caution because it does not occur in hemiagenesis only. For instance, a toxic adenoma that by feedback overrides uptake by the opposite lobe may lead to a similar scintigraphic image. Cases of primary and metastatic thyroid carcinoma and even infiltrative diseases (amyloidosis) with scintigraphic signs superimposable on those of “functional hemiagenesis” but not corresponding to a true anatomical hemiagenesis have also been reported. Neck ultrasound examination is the test of choice to confirm the presence of true anatomical hemiagenesis because it does not yield false images of functional hemiagenesis, is a cost-effective procedure, and does not expose patients to radiation.10
In conclusion, thyroid hemiagenesis is an uncommon congenital abnormality which is probably more prevalent in women and more commonly affects the left thyroid lobe. A certain genetic component appears to be involved in its etiology, and it is more frequently diagnosed in the setting of another thyroid disease. In cases where a presumptive diagnosis is made based on thyroid scintigraphy, work-up should be completed with thyroid ultrasound in order to achieve an adequate diagnosis which excludes potential functional hemiagenesis.
Please cite this article as: Peteiro-Gonzalez D, Cabezas-Agricola JM, Casanueva FF. Hemiagenesia tiroidea: registro de 5 casos y revisión de la literatura. Endocrinol Nutr. 2013;60:e15–e17.