Introduction
The number of bariatric surgeries performed worldwide every year continues to grow because of the increased number of morbidly obese individuals that fail medical treatment and the increased awareness of the safety and success rate of bariatric surgery.1 However, as expected and as a result of the above mentioned the number of complications of bariatric surgery continues to grow as well.2,3 Stricture formation at the gastrojejunal anastomosis (GJA) is a relatively common complication after laparoscopic Rouxen-Y gastrojejunal bypass (LRYGB) that is reported in 3% to 27% of patients.2 The aim was to report the frequency in our institution of complications after bariatric surgery that needed endoscopic treatment.
Methods
A retrospective analysis of data obtained prospectively was made. Patients seen in our department that was undergone to bariatric surgery from May 2004 to May 2007 were included. All patients have a GJA by LRYGB. In every case, before the first procedure, complete blood count, INR, and prothrombin time were obtained for all patients to minimize the risk of bleeding. An experienced endoscopist in EGD performed the procedure in all cases. All procedures for an individual patient performed in the same endoscopy center by the same team. Written informed consent was obtained for each patient and the procedures were performed under deep sedation with midazolam, propofol and phentanyl by an anesthetist. A regular diagnostic endoscope was initially used GIF-100, GIF-130, GIF-140 or GIF-160 (Olympus, American Corp., Melville, NY, USA). Injection was made with epinephrine alone on a 1:10 000 dilutions. Supplemental oxygen was provided by means of nasal catheter. All patients were hospitalized after the procedure for at least 2 hours for surveillance of possible complications.
Statistical analyses: Descriptive statistics were used for demographic variables. Results are expressed as mean ± standard deviation or medians and ranges, according to distribution. Comparison of quantitative data was performed using the Student´s t-test. The differences between proportions of categorical data were obtained by the Fisher exact test when the number of expected subjects was less than five and by the Chi-square test otherwise. A p value < 0.05 was considered statistically significant. All statistical analyses were conducted using the statistics program SPSS/ PC version12.0 (Chicago, IL, USA)
Results
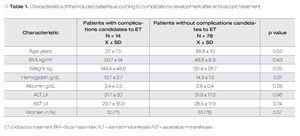
A total of 92 patients were included with a mean ± SD of 38.5 ± 9.6 years. Seventy-one (77.2%) were female. The body mass index (BMI) was 48.9 ± 9.3. The global complications were present in 22 (23.9%) patients with 22 cases, but only 14 (15.2%) patients needed of endoscopic treatment. In Table 1 are shown the characteristics of included patients according to presence of complications.
Of the total of post-surgical complications candidates for endoscopic treatment 12 (13%) cases were stenosis of gastrojejunal anastomosis and 2 (2.2%) cases with ulcers at the anastomotic site. The endoscopic treatment used was pneumatic dilation with balloon for strictures and injection of adrenaline at 1:10,000 dilution for ulcers. The median number of required endoscopic sessions was 4 (1-11). Only one patient required 11 endoscopic sessions, when we removed this data the median of endoscopic sessions were 2 (1-4). All patients were asymptomatic after the last endoscopic session. One patient had perforation as a complication of endoscopic treatment and one patient with bleeding of the anastomosis site that required treatment with injection of adrenaline. There was no mortality related to endoscopic treatment.
Discussion
In this study we found that the frequency of post-bariatric surgery complications requiring endoscopic treatment is high. Our data are consistent with data from previous studies.
In previous studies the most common complications are stenosis of the anastomosis and the presence of ulcers in this level. Our results are consistent with these statements. In relation to the frequency of development of stenosis, the data vary from 3% to 27% according to different studies.4-7 Our results are within the ranges reported. The treatment used in our patients (pneumatic dilation), is consistent with that used by other authors and has a proper success rate with low complications.2 Although in different studies have reported a high frequency of ulcers at the anastomosis in patients with stenosis of the same, in our series had no case in which there are two complications.5 Marginal ulcers occur at the gastrojejunal anastomosis, usually on the intestinal side, and are thought to arise from a number of factors, including local ischemia, staple-line disruption, effects of acid on exposed intestinal mucosa, and the presence of staples or suture material. Factors that increase the risk of marginal ulcers include smoking and nonsteroidal anti-inflammatory drug use, whereas proton pump inhibitor use appears to decrease the risk. The true incidence of a marginal ulcer after an RYGB is uncertain, with reports that range from 1% to 36%.2 In our series, the marginal ulcers was the second most common complication and all our patients were treated with only one endoscopic method without recurrence. Others complications after bariatric surgery as GERD, fistulas, cholecholithiasis, dumping syndrome, diarrhea, nutritional deficiencies, and chronic anemia have been reported but they did not presented in our series.
Some limitations of our study are: 1). although the patients were enrolled as a prospective cohort, the conclusions of this study are limited by the fact that they are based on retrospective analysis; and, 2). the medium sample size. It is important to mention that despite retrospective design and sample size, this is an important world-wide topic and information from other Latin American centers will be useful to improve quality attention in this kind of patients.
In conclusion post-GJA complications requiring endoscopic treatment are frequent. Endoscopic therapy is effective and safe in this group. There were no differences between patients assessed who developed complications and those who did not.
Correspondence: Dr. Félix Ignacio Téllez Ávila. Vasco de Quiroga N°15,
Sección XVI, Tlalpan, D. F. México.
Telephone: (525) 55487 0900 Ext 2150.
E-mail: felixtelleza@gmail.com