Actinomyces spp. are Gram-positive bacilli belonging to the Actinomycetales order which are part of the normal microbiota of the oropharynx and both the urogenital and gastrointestinal tracts.1 Although A. israelii is the most prevalent species isolated in human infections,1,2 there are new species which have been associated with particular clinical syndromes.2,3A. turicensis has been implicated with a range of infections such as urogenital and a variety of skin-related infections.2,3
Only three cases of breast abscess due to A. turicensis have been documented in the medical literature,4–6 but only one of them was isolated in pure culture.6 We report a new case of breast abscess caused by this microorganism in a non-puerperal women found as isolated pathogen.
A 44-year-old women refers six days history of pain, fever and a fluctuating abscess in the right breast. Her clinical history was unremarkable except for several episodes of mastitis. The patient was in treatment with levofloxacin (500mg/12h) and analgesics for 5 days. The fluid was drained and sent to the microbiology laboratory for culture. After centrifugation, the sample was inoculated in blood agar (either aerobic or anaerobic) (BD Columbia Agar 5% Sheepblood®, Becton Dickinson), chocolate agar (BD Choco Agar, Becton Dickinson) and thioglycolate broth (BD™ Fluid Thioglycollate Medium, Becton Dickinson), all incubated at 37°C.
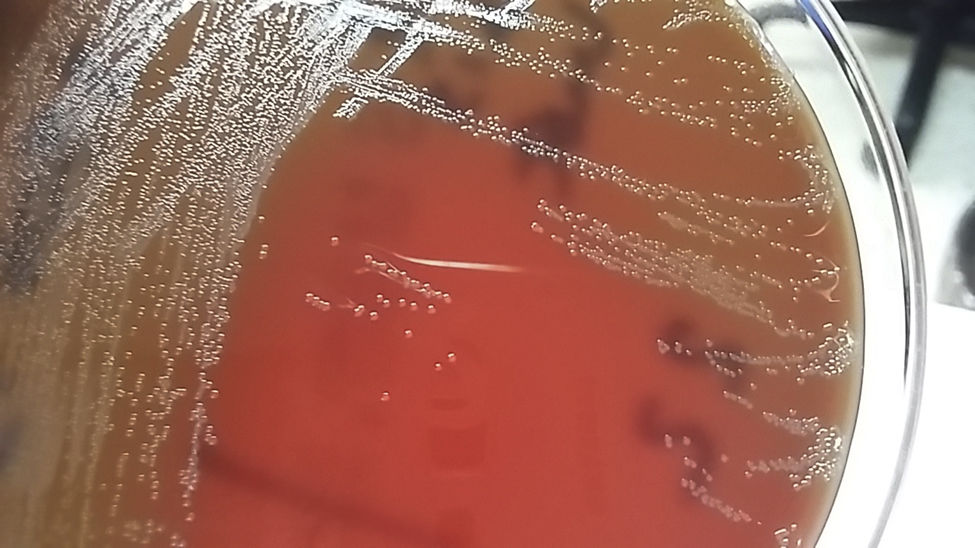
Gram staining of the fluid no exhibited microorganisms, but on the second day of incubation the growth of round and flat colonies was reported specially in the anaerobic blood agar. Greyish and glistening colonies were observed in pure culture (Fig. 1) and a mass spectrometry method (Bruker Biotyper, Billerica, MA, USA) was employed to identify the strain as A. turicensis (score 2.5). The MIC of the bacteria to different antibiotics was carried out by the E-test method in Brucella agar supplemented with hemin, vitamin K1 and laked sheep blood incubated at 37°C, anaerobically. According the CLSI 2016 criteria,7 the strain was susceptible to penicillin (0.19μg/mL), amoxicillin–clavulanate (0.25μg/mL), piperacillin–tazobactam (1.5μg/mL), clindamycin (0.032μg/mL), meropenem (0.38μg/mL), imipenem (0.064μg/mL), and moxifloxacin (1μg/mL), and resistant to metronidazole (>256μg/mL). Antimicrobial treatment was changed to amoxicillin (500mg/8h) for 10 days and at 3 month of follow-up the patient remained well.
A. turicensis produces a wide variety of infections such as genital, urinary, skin-related infections and bacteremias,3 although isolation in breast samples is uncommon. Previously, three reports have shown A. turicensis in breast infections,4,5 and only one in pure culture.6
The diagnosis of A. turicensis is mainly based on culture of an adequate sample obtained from the site of infection. Identification using conventional laboratory methods such as biochemical profiles of strains might be difficult, although A. turicensis is considered aero-tolerant and may clearly be discriminated with the API Coryne (Biomérieux).3 The recent introduction of mass spectrometry for routine analysis in the clinical laboratories may strongly help in the final identification due to it accuracy, as in our case.
Overall, drug resistance in Actinomyces spp. may be initially not considered a problem. They are usually susceptible to β-lactams, especially to penicillin G or amoxicillin, which are considered the drugs of choice for the treatment.8 As alternatives, macrolides and clindamycin have been used successfully. On the other hand, metronidazole and aminoglycosides have not activity against Actinomyces spp.8
Regarding A. turicensis, there are some reports on antibiotic susceptibility against this bacillus.9,10 In these studies, all isolates were susceptible to penicillin and amoxicillin, and a high number of isolates were resistant to fluoroquinolones.9,10 A study demonstrated a number of isolates of A. turicensis resistant to erythromycin,9 and in the other almost uniformly resistance to metronidazole was found.10 Thus, monitoring through susceptibility testing is always advisable.
In summary, the clinical implications of A. turicensis have been clearly established since many infections caused by this pathogen are monomicrobial and have been isolated from various clinical samples. In our case, the isolation of this pathogen also suggest that it is clinically relevant since it was found in pure culture. Physicians and microbiologists should be aware of these new strains of Actinomyces especially if the new diagnostic technologies are applied.
Conflict of interestThe author declare no conflict of interest.