Most of the published studies on patients admitted with 2009 pandemic influenza are not population based. We have compiled the clinical information regarding all children admitted with 2009 pandemic influenza A (H1N1) infection during the season 2009-2010 in our defined population, in order to have an unbiased view of the most severe side of the clinical spectrum of the infection and to quantify its burden.
MethodsChildren <15 years-old admitted to any of 3 hospitals in South-East Spain with 2009 pandemic influenza A (H1N1) detected by means of reverse transcriptase polymerase chain reaction. High quality data were extracted from clinical records specially designed for the pandemic.
ResultsEighty two children fulfilled the inclusion criteria. The hospitalization rate was 68 per 100,000 children <15 years-old; in those <5 years-old the rate was of 131 and in <1 year-old, 234 per 100,000. An estimated 0.7% of the children who suffered from pandemic influenza were admitted (1.7% in <5 years-old). Intensive care was required for 5% of the hospitalized patients living in the study area. Mortality was roughly estimated about 1 per 100,000 children <15 years-old and was associated with the presence of very severe comorbidities or co-infections. Only 20% of the admitted children were ≥5 years-old and without risk factors. The disease followed a generally benign course despite the modest use of oseltamivir (49% of the patients).
ConclusionsClinical and epidemiological data are very similar to those observed in other places and in interpandemic seasons with a high influenza activity.
Pocos artículos sobre pacientes ingresados por la gripe pandémica de 2009 tienen una perspectiva poblacional. Hemos revisado la información clínica de todos los niños que han requerido hospitalización por gripe pandémica A (H1N1) 2009 durante la temporada 2009-2010 en nuestra población, para obtener una visión no sesgada de la faceta más grave de esta gripe y cuantificar su impacto.
MétodosSe incluyeron los niños menores de 15 años ingresados en 3 hospitales del sureste de España con infección por influenza A (H1N1) 2009 confirmada por reacción en cadena de la polimerasa. Los datos se obtuvieron de registros específicos diseñados durante la pandemia.
ResultadosOchenta y dos niños cumplieron los criterios de inclusión. La tasa de hospitalización fue de 68/100.000 niños <15 años; 131/100.000 en los menores de 5 años y 234/100.000 en menores de 1 año. Se estimó que el 0,7% de los niños que padecieron la gripe pandémica requirió ingreso (1,7% en menores de 5 años). El 5% de los niños hospitalizados precisaron cuidados intensivos. La mortalidad se calculó en torno al 1/100.000 menores de 15 años y se asoció con la presencia de otras enfermedades o infecciones graves. Solo 20% de los hospitalizados eran mayores de 5 años y sin factores de riesgo. La enfermedad siguió un curso generalmente benigno pese al uso modesto de oseltamivir (49% de los pacientes).
ConclusionesLos datos clínicos y epidemiológicos son muy similares a los observados durante la pandemia en otros lugares, así como en temporadas interpandémicas con alta actividad gripal.
Every year influenza causes high morbidity and mortality among the pediatric and general population. High risk groups for severe influenza include, young children, elderly people, and patients who suffer from chronic diseases.1 The declaration of the last pandemic by the WHO in June 2009 raised great social and health alarm, and triggered pre-established protocols with measures aimed at reducing the impact of this new but expected situation. Lastly, the clinical and epidemiological characteristics of the infection caused by 2009 pandemic influenza A (H1N1) have been shown to be very similar to those of seasonal influenza.2–5 As a result, many of those measures, and the WHO performance itself, are being subjected to scrutiny to determine their efficiency, the degree of adequacy and the involvement of the commercial interests in health decisions.6
Some series of pediatric patients admitted with 2009 pandemic influenza A (H1N1) infection have been published,7–16 but very few include the whole pandemic with a population perspective, and none in Spain. The alert caused by the declaration of the pandemic in our country provoked an extreme vigilance, stimulating the detection of the virus by means of high reliability techniques in many of the patients with symptoms compatible with influenza, so it is likely that the number of hospitalized patients who have been through an undetected infection caused by 2009 pandemic influenza A (H1N1) is minimal. This exceptional circumstance has led us to retrospectively compile the clinical information regarding pediatric patients admitted with confirmed 2009 pandemic influenza A (H1N1) infection, once the pandemic had ended, in order to determine the most severe side of the clinical spectrum of the infection, as well as quantify its burden in our population.
Patients and methodsThe study was conducted in three hospitals in the province of Alicante: Hospital General Universitario of Alicante (HA), Hospital General of Elda (HE) and Hospital Vega Baja of Orihuela (HO). These hospitals gave public health care to 42,797, 35,051 and 30,178 people <15 years of age in their respective health departments (108,026 in total, 7,269 <1 year of age), according to official data from the Population Information System of the Valencian Community in November 2009. The HA is the only one that has an intensive care unit (ICU) for children older than one month of age, being the reference pediatric ICU for the other two, and the rest of the hospitals of the province, where 298,335 children <15 years of age were registered. Pediatric hospitalization in private facilities is almost non-existent in the province of Alicante.
We went through all the records of children hospitalized from June 2009 to July 2010 and in whom the presence of 2009 pandemic influenza A (H1N1) was analyzed on respiratory tract secretions by means of reverse transcriptase polymerase chain reaction. Patients with a positive result were included in the present study. Data from the medical history of these patients, specially registered during the pandemic, were reviewed and extracted using a form designed to record the relevant information. This included demographic data, the presence of risk factors for severe influenza, the symptoms and signs at admission, the care and treatment needed during their hospitalization, the outcomes and the dates in which they occurred. Infections were considered nosocomial when symptoms started during hospitalization for another reason. Otherwise, they were considered infections acquired in the community. The study was approved by the Clinical Research Ethics Committee of the Hospital General Universitario of Alicante.
Data were entered, reviewed and analyzed using SPSS (v17.0, SPSS, Chicago, IL, USA). Descriptive statistics included frequency analysis for categorical variables and medians for continuous variables. We used two sample t tests or Mann-Whitney U test (depending on whether the criteria for normality were fulfilled or not) for continuous variables and χ2 test or Fisher exact test for categorical variables in bivariate analysis. Probabilities were two tailed and a P value of <.05 was considered significant.
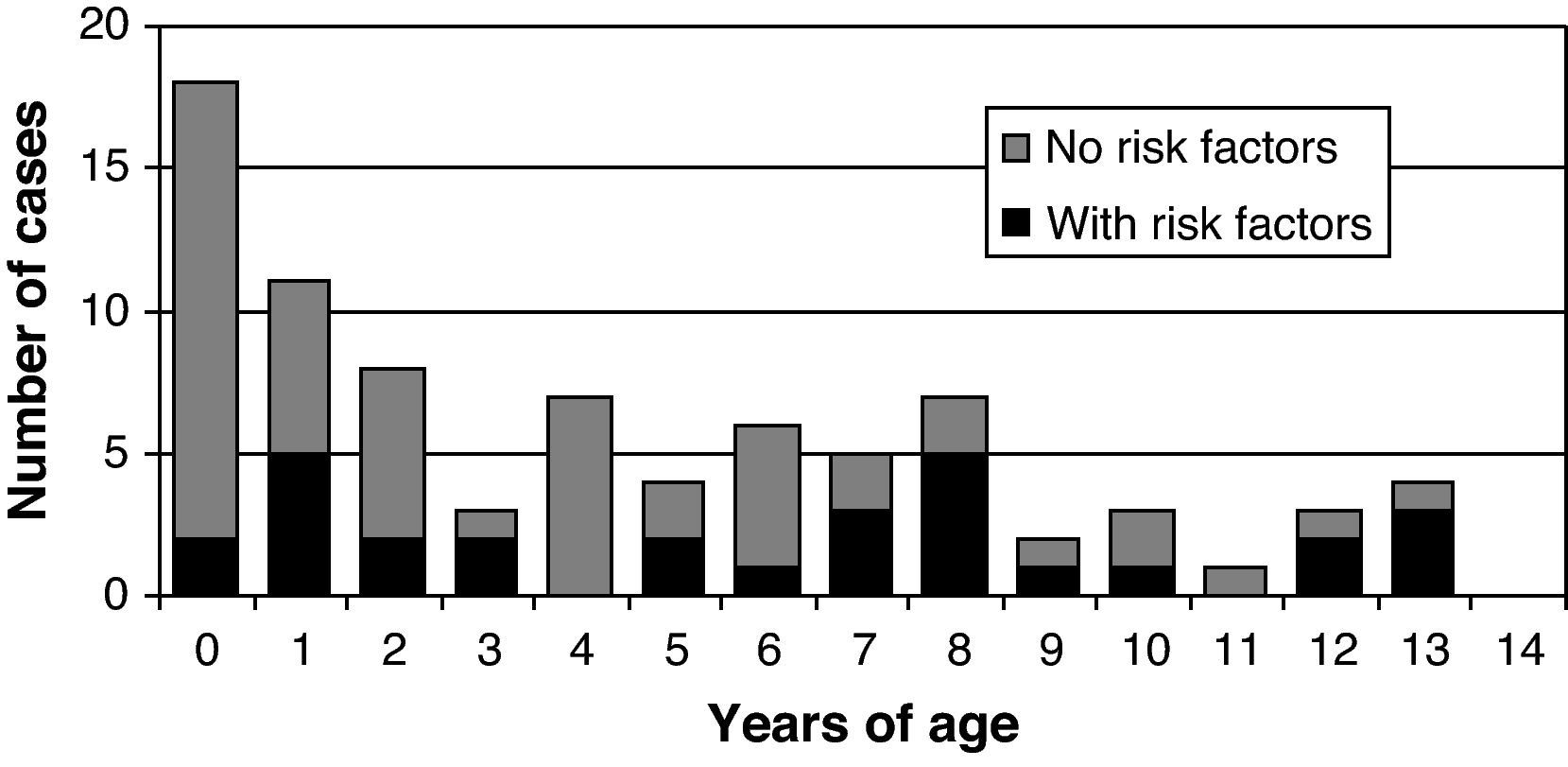
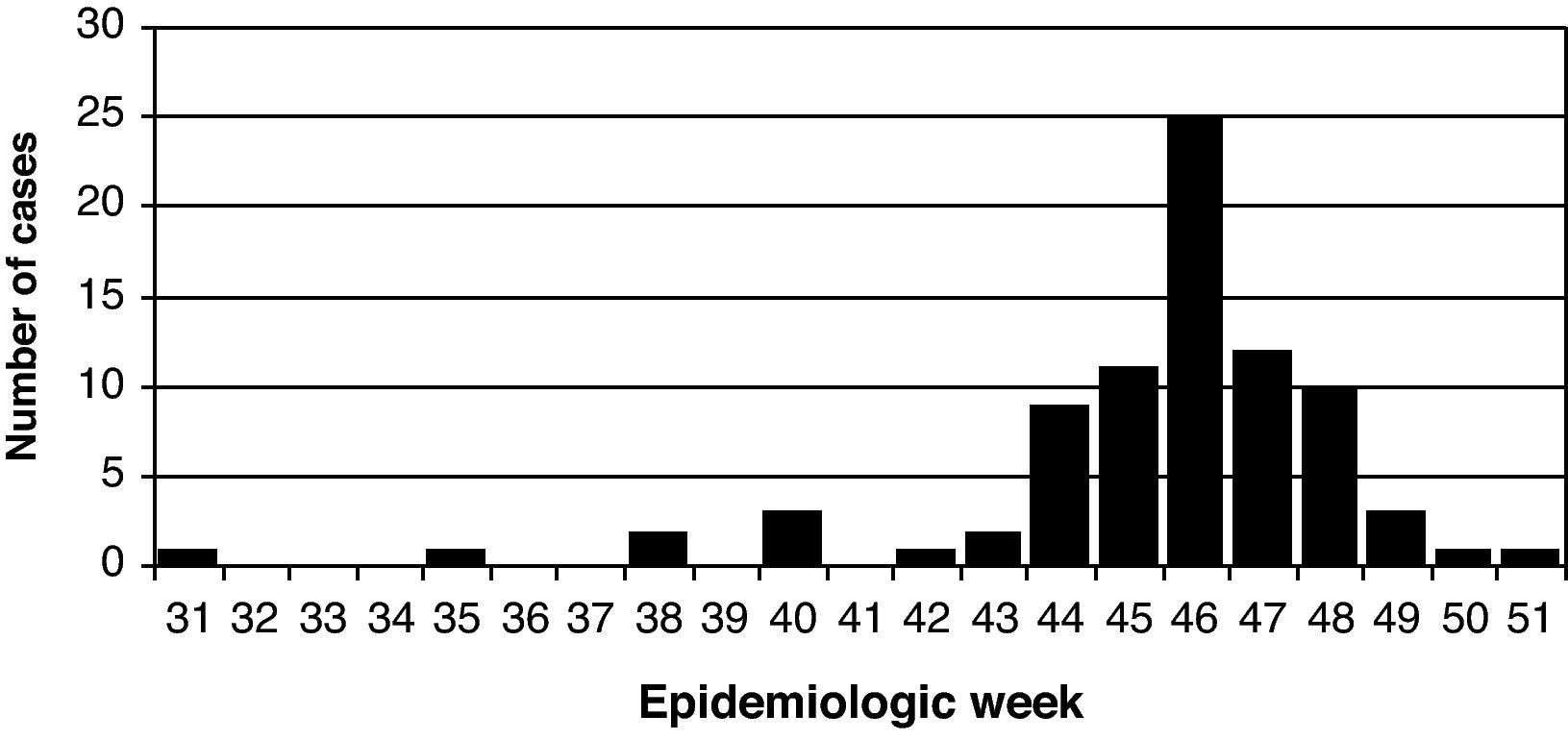
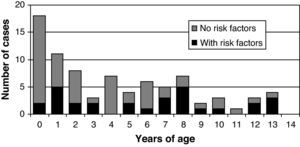
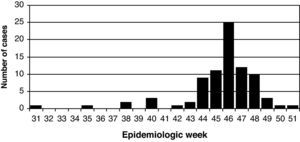
ResultsData from 82 children who fulfilled the inclusion criteria were collected. Fifty two patients (63%) were male, with a median of 4 years of age (Fig. 1). All the patients were hospitalized between August and December (Fig. 2). However, most of them were admitted in November: between the epidemiological weeks 44 and 48 (November 1 to December 5) when 68 cases were admitted (83% of the total). No differences were observed in the temporal distribution between the three centers. The infection was considered of nosocomial origin in 5 cases, all of them between weeks 45 and 48, with symptoms of infection appearing 4 to 35 days after admission. No new cases were detected in 2010.
Thirty nine patients were hospitalized in HA, 21 patients in HE and 22 in HO. Nine of the patients admitted to HA came from other areas not included in the study, 7 of them transferred from their hospitals because of the severity of the disease or for the risk of worsening. When excluding these 9 patients, the hospitalization rate was 70, 60 and 73 per 100,000 children <15 years of age for the HA, HE and HO areas, respectively, which were not significantly different. The rate was 68 per 100,000 for all three areas (95% confidence interval (CI), 52 to 83). The hospitalization rate in infants <1 year of age was 234 per 100,000 (95% CI, 123 to 345) and in children ≥1 year of age it was 56 per 100,000 (95% CI, 41 to 70); children <5 years of age were hospitalized at a rate of 114 per 100,000 (95% CI, 79 to 149) (83 per 100,000 between 1 and 4 years of age, both included; 95% CI, 50 to 117), and in those ≥5 years of age the rate was 44 per 100,000 (95% CI, 29 to 60).
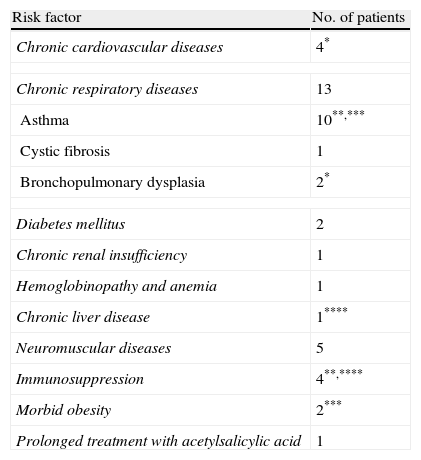
Thirty patients (37%) had a chronic disease considered of risk for severe influenza (Table 1). Four patients had 2 risk factors each. Risk factors were present in 23% of children <5 years-old and in 54% of those ≥5 years-old (P=.006) (Fig. 1). The median age for children with risk factors was 7 years, and for those without risk factors it was 2 years (P=.001). Only 16 children (20% of the total) were ≥5 years-old and did not have risk factors. Twelve children were vaccinated against seasonal influenza, 11 of them with risk factors, and only 2 children had also been vaccinated against 2009 pandemic influenza A (H1N1), which started in week 46, and represented 15% and 2% of all the patients, and 39% and 7% of the patients ≥6 months-old with risk factors.
Risk factors in 30 patients admitted with 2009 pandemic influenza A (H1N1) infection
| Risk factor | No. of patients |
| Chronic cardiovascular diseases | 4* |
| Chronic respiratory diseases | 13 |
| Asthma | 10**,*** |
| Cystic fibrosis | 1 |
| Bronchopulmonary dysplasia | 2* |
| Diabetes mellitus | 2 |
| Chronic renal insufficiency | 1 |
| Hemoglobinopathy and anemia | 1 |
| Chronic liver disease | 1**** |
| Neuromuscular diseases | 5 |
| Immunosuppression | 4**,**** |
| Morbid obesity | 2*** |
| Prolonged treatment with acetylsalicylic acid | 1 |
*, **, *** and **** correspond to the four patients who combined two different risk factors.
Excluding 5 patients with nosocomial infection and 2 whose dates were not registered, the admission occurred at a median time of 1 day after the onset of symptoms (range 0-9 days). There were no significant differences between patients with or without risk factors (P=.96), or in those <5 or ≥5 years-old (P=0.23), but differences were significant between those <1 and ≥ 1 year old (median time of 1 and 2 days respectively; P=.001). The median time of hospitalization (excluding 7 patients with nosocomial infection or deceased) was 3 days (range 0-12 days). Hospital stay was not significantly different as regards patient age, but it was close to reaching significance depending on the presence or absence of risk factors (median time of 4 and 3 days respectively; P=.055). The median duration of the disease (days prior to admission plus hospital stay) in the remaining 73 patients (excluding nosocomial infections, deceased and those who had no date of onset of symptoms) was 6 days (range 1-16 days), with no differences as regards ages or risk factors.
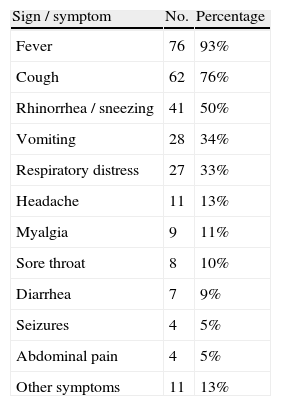
The most frequent signs and symptoms on admission were fever, cough, rhinitis, vomiting and respiratory distress (Table 2). Four patients had seizures but no other signs of encephalitis. The main diagnosis at discharge was influenza in thirty eight patients (46%). Other frequent diagnoses at discharge were pneumonia (14 patients, 17%), pneumonitis (10 patients, 12%) and bronchitis, bronchiolitis or asthma (11 patients, 13%).
Signs and symptoms observed at admission in 82 patients with 2009 pandemic influenza A (H1N1) infection
| Sign / symptom | No. | Percentage |
| Fever | 76 | 93% |
| Cough | 62 | 76% |
| Rhinorrhea / sneezing | 41 | 50% |
| Vomiting | 28 | 34% |
| Respiratory distress | 27 | 33% |
| Headache | 11 | 13% |
| Myalgia | 9 | 11% |
| Sore throat | 8 | 10% |
| Diarrhea | 7 | 9% |
| Seizures | 4 | 5% |
| Abdominal pain | 4 | 5% |
| Other symptoms | 11 | 13% |
Forty patients (49% of the total) were treated with oseltamivir, with no significant differences between the 3 hospitals. None of them had been treated before admission. In 24 of those 40 treated (60%) oseltamivir was given before having laboratory confirmation of the infection, and in 13 (33%) it was started within 48hours of the onset of symptoms. Only 2 patients had laboratory results and started the treatment in the first 48hours. Forty eight patients (59%) were given antibiotics. Of the 52 patients without risk, 16 (31%) were treated with oseltamivir and 27 (52%) with antibiotics. Of the 30 patients with risk factors, 24 (80%) were treated with oseltamivir and 21 (70%) with antibiotics. These differences were significant in the case of oseltamivir (P<.001), but not for antibiotics (P=.16).
Oxygen supplementation was provided to 22 patients (27%), of whom 17 were also given oseltamivir and antibiotics, but only 1 patient was given oxygen without either oseltamivir or antibiotics. The use of oxygen was significantly more frequent in patients with risk factors and increased significantly with age. Eight patients required intensive care (10% of the patients of the series and 5% of the patients from the areas of the hospitals of the study), 5 in pediatric ICU and 3 in newborn ICU, and were admitted between the weeks 44 and 48. Six patients needed respiratory support and 3 died (Table 3). All patients on intensive care received treatment with oseltamivir and broad-spectrum antibiotics. No significant relationship was observed between admission to the ICU and age, risk factors, previous vaccination, time from onset to admission, or the use of oseltamivir in the first 48hours of disease. Four ICU patients came from the HA area and 4 came from other areas not included in the study. The rate of admission to an ICU on the population covered by the 3 hospitals participating in this study was 3.7 per 100,000 <15-year-olds, the rate of respiratory support was 1.9 per 100,000 <15-year-olds, and the rate of invasive respiratory support and mortality was 0 per 100,000. The 3 deceased patients represented a mortality rate of 1.0 per 100,000 <15-year-olds, but it is not possible to rule out any other death in the province that had not been transferred to HA.
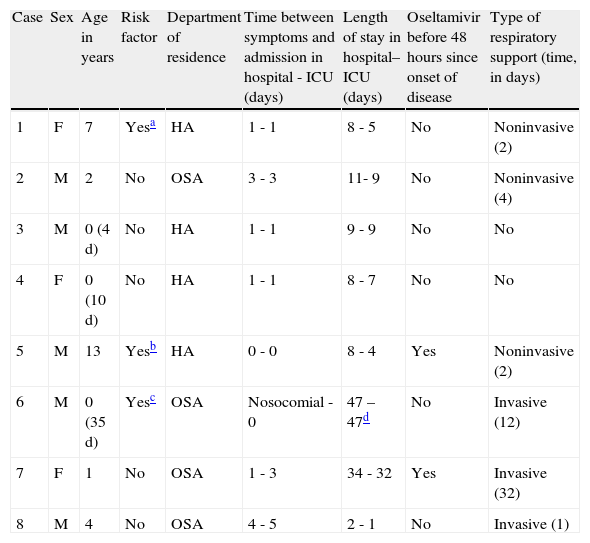
Children admitted to ICU (in chronological order): epidemiologic characteristics, time course, treatment received, final diagnosis and outcome
| Case | Sex | Age in years | Risk factor | Department of residence | Time between symptoms and admission in hospital - ICU (days) | Length of stay in hospital–ICU (days) | Oseltamivir before 48hours since onset of disease | Type of respiratory support (time, in days) |
| 1 | F | 7 | Yesa | HA | 1 - 1 | 8 - 5 | No | Noninvasive (2) |
| 2 | M | 2 | No | OSA | 3 - 3 | 11- 9 | No | Noninvasive (4) |
| 3 | M | 0 (4 d) | No | HA | 1 - 1 | 9 - 9 | No | No |
| 4 | F | 0 (10 d) | No | HA | 1 - 1 | 8 - 7 | No | No |
| 5 | M | 13 | Yesb | HA | 0 - 0 | 8 - 4 | Yes | Noninvasive (2) |
| 6 | M | 0 (35 d) | Yesc | OSA | Nosocomial - 0 | 47 – 47d | No | Invasive (12) |
| 7 | F | 1 | No | OSA | 1 - 3 | 34 - 32 | Yes | Invasive (32) |
| 8 | M | 4 | No | OSA | 4 - 5 | 2 - 1 | No | Invasive (1) |
| Case | Final diagnosis (in addition to 2009 pandemic influenza A (H1N1) infection) | Death |
| 1 | Pneumonitis | No |
| 2 | Middle lobe pneumonia | No |
| 3 | Neonatal seizures (with normal CSF, EEG and cranial MRI) | No |
| 4 | Late onset neonatal Klebsiella pneumoniae sepsis, neonatal seizures | No |
| 5 | Severe asthmatic exacerbation | No |
| 6 | Prematurity (28 weeks, 830 g), bronchopulmonary dysplasia, patent ductus arteriosus, bronchopneumonia | Yes |
| 7 | Bilateral necrotizing pneumonia, Streptococcus pneumoniae sepsis, pneumothorax, mechanical ventilation associated Pseudomonas pneumonia | Yes |
| 8 | Streptococcus pneumoniae septic shock, acute lymphoblastic leukemia onset | Yes |
d, days; HA, Hospital of Alicante; OSA, out of study area.
The extraordinary surveillance of 2009 pandemic influenza A (H1N1) allows us to be confident that the 82 patients included in our study are all those who had required hospitalization in our hospitals and were infected by 2009 pandemic influenza A (H1N1) throughout the pandemic season. This is the major strength of the study, as it gives us an unbiased population perspective of the burden and the clinical characteristics of the severe 2009 pandemic influenza A (H1N1) infection in our area. As in other locations in the northern hemisphere, pandemic activity peaked in autumn, where a massive contagion took place, most of the severe cases emerging at that time. Other epidemiological aspects were similar to those known for seasonal influenza in children in our contry.17
Slightly more than one third of the patients had any risk factor for influenza, mainly asthma and other chronic respiratory diseases, followed by neuromuscular and cardiovascular diseases and immunosuppression. Nevertheless, only 39% of them were vaccinated against seasonal flu. This figure is better than that usually observed in Spain in children of risk, which is normally below 20%,18 but it stresses the low perception that doctors and patients have about its benefit, even in spite of the social alarm generated by the pandemic.
Our patients were hospitalized in the first days of disease, and the hospital stay was short. The disease usually resolved within a week, and almost none lasted more than 2 weeks. Infants were hospitalized earlier, but the hospital stay was longer in those who had risk factors. Both the predominant symptoms and the main diagnoses at discharge showed a disease similar to seasonal influenza, with frequent involvement of the lower airway.
No patient had been given oseltamivir before admission, only half of them were given oseltamivir during the hospitalization, and only one third of these (17% of all the patients) started within 48hours of the disease onset. Oseltamivir was used more often in patients with risk factors, and in those treated with antibiotics. The limited use of oseltamivir did not affect the benign course of the disease in most of the patients. Antibiotics were used more frequently than oseltamivir and independently of the presence of risk factors.
Eight children required ICU. Two of them were newborns coming from their homes, they started oseltamivir late in the disease, did not require respiratory support and were discharged in less than 10 days. Three children required non-invasive mechanical ventilation for 2 to 4 days and recovered satisfactorily. The 3 deceased patients, including one patient early treated with oseltamivir, required invasive mechanical ventilation and their clinical course was complicated because of very severe concurrent diseases, including bacterial co-infections.
Data from the Influenza Surveillance Network of the Valencian Community indicated a cumulative rate of influenza in season 2009-2010 of 7,772 cases per 100,000 inhabitants <5 years of age and 9,983 cases per 100,000 inhabitants among children 5-14 years of age, much higher than in adults.19 These figures are 3 times higher than the average for the period 2002-2008 in Spain,20 though is difficult to know how much it was affected by the special surveillance of this latter season. Combining the cumulative rate of influenza in the Valencian Community with our hospitalization rate, resulted in 0.7% of the children with 2009 pandemic influenza A (H1N1) being admitted, 1.7% <5 years of age and 0.5% between 5 and 14 years of age.
Hospitalization rates in <5-year-olds in the Basque Country (Spain) during three influenza seasons (July 2001 - June 2004) were 120, 10 and 150 per 100,000 (an average of 90 per 100,000).21 The average ratio of admitted to children diagnosed with influenza in each season was 1.1%. The average hospital stay was 5 days (range 2-18), 3 patients required ICU (6.1%) and none died. Our results fit perfectly among those observed in interpandemic seasons in that study. In another study in <3-year-old children admitted with influenza in a Madrid hospital over an 8 year period, the rates of hospitalization ranged between 11 and 154 per 100,000, although they were possibly underestimated.22
The rate of hospitalization associated to 2009 pandemic influenza A (H1N1) in 6 public hospitals of the metropolitan area of Buenos Aires (during the one-wave pandemic of southern hemisphere) was lower than in our study, 21 per 100,000 <18-year-olds, not reaching 200 per 100,000 in <1-year-olds.7 Patients of that series were, younger than ours (75% <2-years-old), 17% were co-infected with respiratory syncytial virus, and were admitted later than ours (at an average of 4 days from disease onset). Oxygen was required for 82% of patients, intensive care for 19% of patients, and mechanical ventilation for 17%, figures greater than ours. Mortality was 7.6 per 100,000 in <1 year-olds and 1.1 per 100,000 in <18-year-olds. In other southern hemisphere locations, for example, Australia, the hospitalization rate in <5-year-olds was about 60 per 100,000, slightly higher than that observed in previous influenza seasons but lower than that observed in our study.23 The clinical profile was similar to that observed in our patients.8The cumulative hospitalization rate associated with 2009 pandemic influenza A (H1N1) registered by the Emerging Infections Program (EIP) in the United States was 83 per 100,000 <5 years of age and 34 per 100,000 children 5-17 years of age.24 In a population based study, the hospitalization rate for 2009 pandemic influenza A (H1N1) in <17-year-olds was 25 per 100,000, 1.5% of those infected, while in the two previous years it had been 15 and 50 per 100,000.4 These figures are high but not so different from those reported for seasonal influenza, although there were marked variations between seasons and locations, and possibly they underestimated the true data.25–28 Three series of pediatric patients hospitalized in the United States showed similar characteristics to ours, although in those reports more children with risk factors were admitted (67-81%), more frequently were obese, the majority were given antiviral drugs (64-99%), and required more interventions, including ICU in 19-30%.9–11
A population based, whole-pandemic study in Israel showed very similar results to ours, with a hospitalization rate of 72 per 100,000 <19-year-olds. They concluded that the severity and mortality of 2009 pandemic influenza A (H1N1) were similar to the figures reported in the literature on seasonal influenza.12 The number of estimated deaths associated to 2009 pandemic influenza A (H1N1) in England was 70 in <18-year-olds, which gave a mortality of 0.6 per 100,000, particulary high in <1-year-olds.29 Children hospitalized in Canada and the United Kingdom showed similar characteristics to those of our series and those of previous interpandemic influenza seasons.13–16,30,31
In conclusion, our review is comparable to, and reinforces, those studies showing that pediatric hospitalization related to 2009 pandemic influenza A (H1N1) infection has been high, although it does not appear to be very different from that seen in years with intense activity of seasonal influenza. The majority of our patients followed a satisfactory clinical course, in spite of the limited use of oseltamivir. The 3 deceased patients had very severe associated comorbidities and bacterial co-infections. Given the resemblance of the disease provoked by the 2009 pandemic influenza A (H1N1) with other seasonal influenza viruses, this study gives us an outlook of the burden of influenza on our pediatric population in a high activity year. This last influenza pandemic has increased some previous uncertainties on aspects related to the epidemiology and the measures for the control of the disease, as well as raising new concerns on the way experts and authorities must deal with these uncertainties in usual and exceptional influenza seasons.
Conflict of interestsThe authors declare that they have no conflicts of interest related to this study.