Patients with locally advanced breast cancer receiving preoperative chemoradiation have a 45% surgical complication rate including surgical site infection, dehiscence and flap necrosis.1 Secondary chest wall osteomyelitis (CWO) is an infrequent, poorly described event, usually a complication of cardiothoracic surgery. After breast surgery, it has been described anecdotally.
The aim of this study was to describe a follow-up case series of patients who presented with CWO after mastectomy. Between January 2005 and August 2010, eleven patients developed CWO. Ten had tumors >5cm, 4 (36.3%) were ulcerated at diagnosis; 10 had locally advanced breast cancer, and 1 metastatic disease. Bone scans (99mTc-MDP) prior to treatment were negative for bone metastasis in all cases. Patients received anthracycline based neoadjuvant chemotherapy; none had an adequate clinical response. Nine were treated with concomitant chemoradiation and 2 received preoperative radiation; ten (91%) developed radioepithelitis. All, except one underwent modified radical mastectomy.
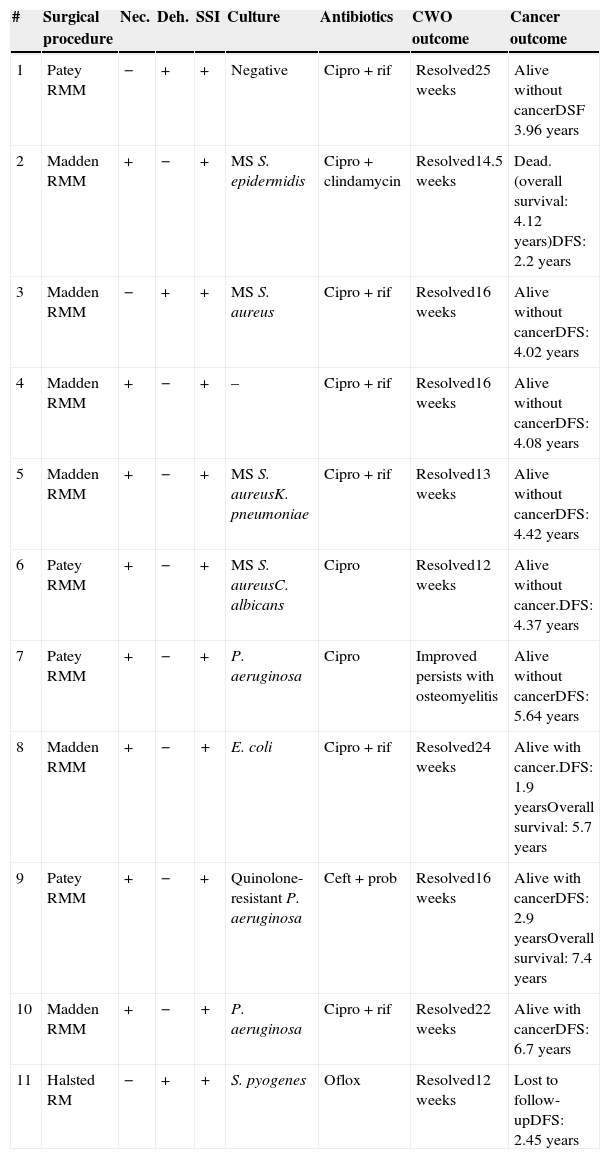
Patients with a non-healing wound and excruciating pain in 1 or more costal arches, not responding to standard clinical care were evaluated for CWO. Ten patients underwent radionuclide bone scan with 99m Technetium-Ubiquicidin (99mTc-UBI) and 1 with 99mTc-MDP, being abnormal in all cases. Wound cultures were obtained through swab technique in 10 (91%) patients. The most common pathogens were: Staphylococcus aureus (3, 33.3%) and Pseudomonas aeruginosa (3, 33.3%). At CWO diagnosis, 8 (88.8%) were treated with ciprofloxacin+rifampin, 3 with ciprofloxacin, and one with ceftibuten+probenecid. Mean duration of treatment was 19.8 weeks. Four patients (36.4%) underwent surgical lavage, 2 required infected rib extraction, and 2 underwent split thickness skin grafting for defect covering. CWO resolved in 10/11 patients. In Table 1, clinical, microbiology data and outcome related variables are shown for each case.
Clinical, microbiology and outcome information related to chest wall osteomyelitis in patients with breast cancer.
| # | Surgical procedure | Nec. | Deh. | SSI | Culture | Antibiotics | CWO outcome | Cancer outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | Patey RMM | − | + | + | Negative | Cipro+rif | Resolved25 weeks | Alive without cancerDSF 3.96 years |
| 2 | Madden RMM | + | − | + | MS S. epidermidis | Cipro+clindamycin | Resolved14.5 weeks | Dead. (overall survival: 4.12 years)DFS: 2.2 years |
| 3 | Madden RMM | − | + | + | MS S. aureus | Cipro+rif | Resolved16 weeks | Alive without cancerDFS: 4.02 years |
| 4 | Madden RMM | + | − | + | – | Cipro+rif | Resolved16 weeks | Alive without cancerDFS: 4.08 years |
| 5 | Madden RMM | + | − | + | MS S. aureusK. pneumoniae | Cipro+rif | Resolved13 weeks | Alive without cancerDFS: 4.42 years |
| 6 | Patey RMM | + | − | + | MS S. aureusC. albicans | Cipro | Resolved12 weeks | Alive without cancer.DFS: 4.37 years |
| 7 | Patey RMM | + | − | + | P. aeruginosa | Cipro | Improved persists with osteomyelitis | Alive without cancerDFS: 5.64 years |
| 8 | Madden RMM | + | − | + | E. coli | Cipro+rif | Resolved24 weeks | Alive with cancer.DFS: 1.9 yearsOverall survival: 5.7 years |
| 9 | Patey RMM | + | − | + | Quinolone-resistant P. aeruginosa | Ceft+prob | Resolved16 weeks | Alive with cancerDFS: 2.9 yearsOverall survival: 7.4 years |
| 10 | Madden RMM | + | − | + | P. aeruginosa | Cipro+rif | Resolved22 weeks | Alive with cancerDFS: 6.7 years |
| 11 | Halsted RM | − | + | + | S. pyogenes | Oflox | Resolved12 weeks | Lost to follow-upDFS: 2.45 years |
RMM, radical modified mastectomy; RM, radical mastectomy; Nec, necrosis; Deh, dehiscence; SSI, surgical site infection; CWO, chest wall osteomyelitis; Cipro: ciprofloxacin; Rif, rifampin; Ceft, ceftibuten; Prob, probenecid; Oflox, ofloxacin; DFS, disease free survival (from cancer diagnosis to recurrence or metastasis. In patients without recurrence or metastasis is as well, overall survival).
There are few reports of late CWO occurring years after breast irradiation.2 To the best of our knowledge, this is the first report of CWO after surgery in patients with breast cancer.
Patients described in this series share multiple characteristics. Most were women with tumors greater than 5cm, without an adequate response to neoadjuvant chemotherapy that further received concomitant chemoradiation and underwent radical surgery. During the postoperative period, all developed major surgical wound complications.
Diagnosis of CWO in previously radiated patients remains a challenge. Bone biopsies for culture are barely available, and osteonecrosis can mimic a bone infection. 99mTc-UBI scintigraphy has been used in our Institution for several years for evaluating osteomyelitis. 99mTc-UBI scintigraphy is an antimicrobial peptide, which selectively binds the bacterial wall and allows discrimination between inflammation and infection,3–7 most useful in these patients. Clinical studies have reported 96% sensitivity and 100% specificity3,8 when compared with conventional Tc-MDP scans and bone biopsy; however, its efficacy has not been proved in large randomized controlled trials.
Treatment of chronic osteomyelitis is challenging. Despite continued research, most aspects of antibiotic treatment are still poorly understood.9 In our series, most of the patients (88.8%) were treated with oral ciprofloxacin, which has excellent bioavailability and bone penetration. In 8 patients, a combination of ciprofloxacin+rifampicin was used, as rifampin enhance fluorquinolone regimens for staphylococci and to prevent resistance.10
This report has several limitations. As in any retrospective study some data was missing and different clinicians treated these patients. Although considered as the gold standard for osteomyelitis diagnosis, we were unable to obtain a bone biopsy for culture in any patient due to the high morbidity related to costal arch sampling in irradiated tissue. In these patients, there is an increased risk of a non-healing wound. Despite these biases, the high specificity of 99mTc-UBI scintigraphy, along with clinical improvement, and a decrease on inflammatory markers, supports CWO diagnosis.
CWO is uncommon, but is likely underestimated. It increases health-care costs and produces such disability that warrants timely recognition. This study provides information for clinicians involved in the treatment of patients with advanced breast cancer, wound complications and CWO.