The clinical presentation of dermatomycoses caused by the genus Neoscytalidium is similar to that caused by dermatophyte fungi. This genus is endemic to tropical regions1 and the cases described in Spain and in other non-endemic countries are usually natives or people who have recently travelled to these places. In relation to this, we present four cases of superficial infection caused by fungi of the genus Neoscytalidium in patients who have travelled to South America.
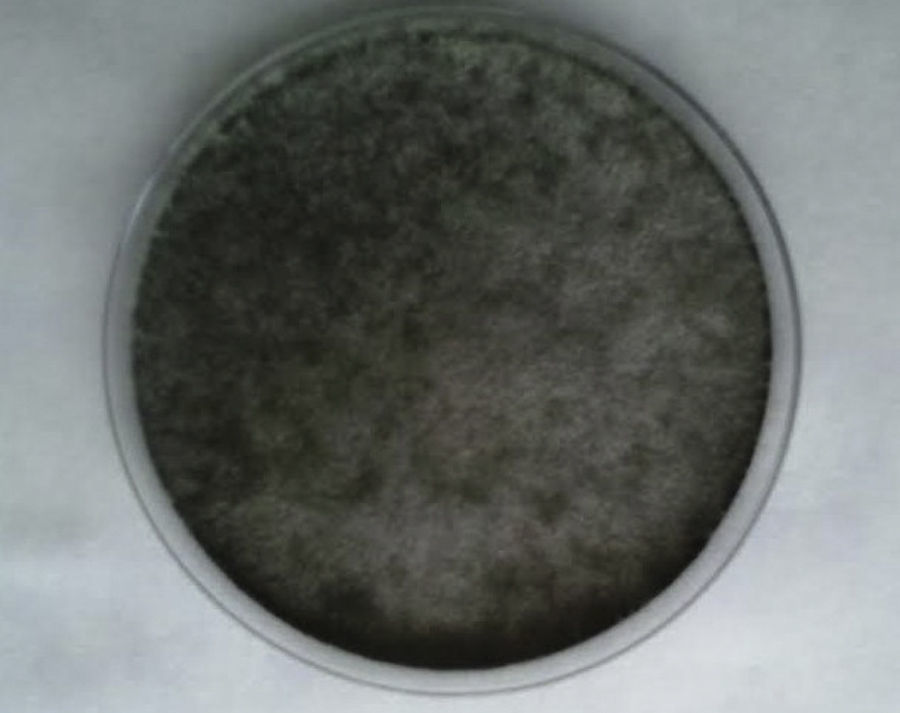
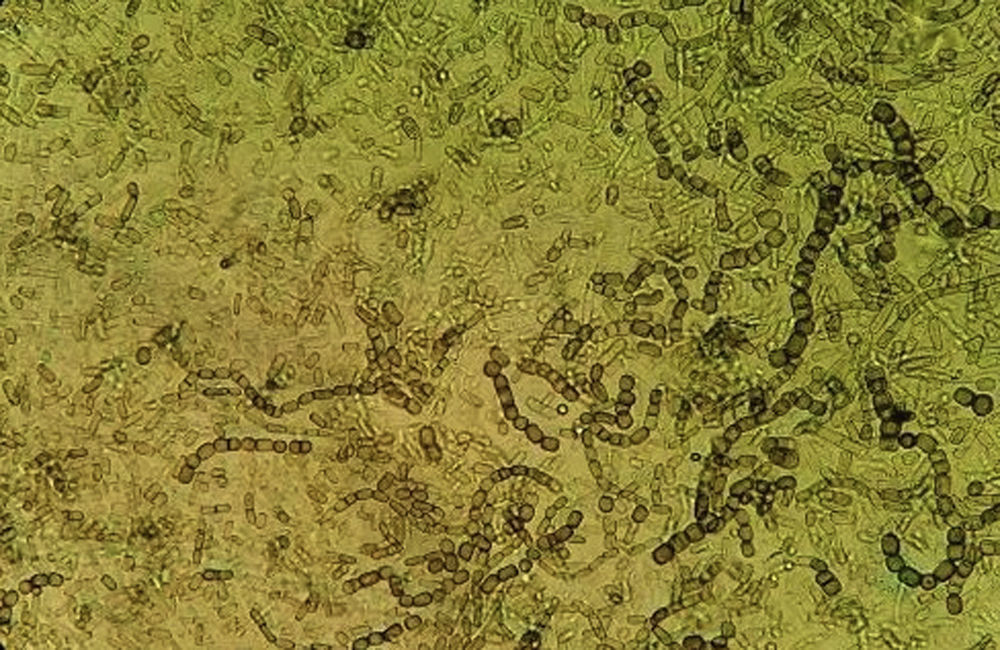
The first patient was a woman aged 59, originally from Colombia, who had signs of onycholysis on the first toes of both feet. Due to the suspicion of onychomycosis, fragments of the affected nails were collected and sent to our laboratory for mycological study. Empiric therapy with terbinafine was prescribed. After one week of incubation, the growth of a filamentous fungus was observed on Sabouraud Chloramphenicol-Gentamicin agar plates; not on Sabouraud Chloramphenicol Actidione agar. The appearance of the colony was initially white and fluffy, and turned a grey-green colour and darkened to form a black discoloration (Fig. 1). The microscopic image was quite characteristic: abundant unicellular and bicellular arthroconidia in chains.1 Arthroconidia – hyaline type became brown and the wall thicker when maturing (Fig. 2). The hyphae were generally pigmented and thick-walled. The diagnosis was performed by observing the macroscopic and microscopic characteristics of the fungus and, in order to confirm its identification, the strain was sent to the Majadahonda National Reference Centre (CNM) where it was molecularly identified as Neoscytalidium dimidiatum by ITS region sequencing. The sequences thus obtained were edited and assembled using the SeqMan II and EditSeq (Lasergene, DNASTAR, Inc., Madison, WI, USA) programs. They were subsequently compared with the Mycology Department database using the InfoQuest FP program, version 4.50 (BioRad, Madrid, Spain). (It has recently been reported that N. dimidiatum is a synonym of Neoscytalidium hyalinum2). The epidemiological characteristics and evolution of the lesion was not possible because the patient did not attend the screening visit.
The second case also corresponds to a 31-year-old woman from Colombia. She also presented lesions in the toenails of both feet. This was done in the same manner as the previous case. This time, the diagnosis was exclusively carried out by observing the macroscopic and microscopic characteristics of the colony: rapid growth in Sabouraud Chloramphenicol Gentamicin Agar – white in colour and cottony appearance (Fig. 3). Under the microscopic, chains of hyaline arthroconidia – that were unicellular or bicellular – were also observed. The strain was identified as N. hyalinum. It was not possible to observe the evolution of the patient as she did not attend the medical check-up.
The third case is a man who, like the two previous cases, was born in Colombia and made frequent visits to his country. This 42-year-old patient presented scaly and itchy eczema type lesions on the soles of both feet 6 months prior to his consultation. In suspicion of dermatomycosis, the same procedure described above was carried out for mycological study, though in this case the sample was obtained by scraping the lesion. The species was identified as N. dimidiatum according to morphological characteristics, similar to the features in the first case. The patient initially received topical treatment with terbinafine and, subsequently, this antifungal agent orally with topical clotrimazole, when the identity of the causative agent was revealed. Evolution was good, with no lesions.
The last case corresponds to a 55-year-old man from Spain who had made trips to endemic countries such as Mexico and Costa Rica several times. The patient presented a lesion in the toenail of left foot. The lesion had been present for 4 years and he had received topical azol treatment without recovery. Fragments of the affected nail were collected and mycology study was carried out as described in the previous cases. Diagnosis of N. dimidiatum was performed by observing the macroscopic and microscopic characteristics of the fungus and the species was confirmed by The National Microbiology Reference Center using the same procedure mentioned in the first case. When the identification was made the patient started to receive oral terbinafine. This has recently occurred and it is soon to observe the evolution of the lesion.
Nail and skin infections caused by Neoscytalidium spp. those mainly affecting the feet represent a common disease in tropical and subtropical countries. In this study, the patients were residents in Spain, and had travelled to endemic areas. Its frequency in Spain is low,3 although an increase has been observed in recent years mainly due to increased immigration from endemic areas, increased tourist travel to these areas and also due to improved clinical and microbiological diagnosis of ringworm caused by non-dermatophyte fungi. The increase in cases of this fungus leads us to believe it is a causing agent of nail and skin infections.
It must be considered that for the isolation of this dematiaceous, a medium without actidione must be used. Thus, adequate processing of the sample in the laboratory will help ensure this pathogen is not overlooked.
Moreover, skin lesions caused by Neoscytalidium are clinically indistinguishable from dermatophytosis (ringworm)3,4; hence the initial empiric treatment of choice is usually terbinafine. However, while this fungus is sensitive to various antifungal agents in vitro – including terbinafine – in vivo the response is quite low, particularly in ungual infections.4,5 Treatment with topical azoles (isoconazole, clotrimazole) and amphotericin B solution, they tend to be more responsive, especially in lesions that do not affect nails.5
In conclusion, we would like to highlight the increasing isolation of unusual fungi in our environment and whose suspicion will help in the etiologic diagnosis of dermatomycosis.
Conflict of interestThe authors declare no source of funding for the development of this document or conflict of interest.
We would like to thank Dra. M. del Carmen García García (dermatologist at the García Noblejas specialty centre, Madrid) and Dra. Ana Alustrey (Mycology Laboratory at the CNM) for their collaboration.