HIV-immigrant use of health services and related cost has hardly been analysed. We compared resource utilisation patterns and direct health care costs between Spanish and immigrant HIV-infected patients.
MethodsAll HIV-infected adult patients treated during the years 2003–2005 (372 patients) in this hospital were included. We evaluated the number of out-patient, Emergency Room (ER) and Day-care Unit visits, and number and length of admissions. Direct costs were analysed. We compared all variables between immigrant and Spanish patients.
ResultsImmigrants represented 12% (n=43) of the cohort. There were no differences in the number of out-patient, ER, and day-care hospital visits per patient between both groups. The number of hospital admissions per patient for any cause was higher in immigrant than in Spanish patients, 1.3 (4.4) versus 0.9 (2.7), P=.034. A high proportion of visits, both for the immigrant (45.1%) and Spanish patients (43.0%), took place in services other than Infectious Diseases. Mean unitary cost per patient per admission, out-patient visits and ER visits were similar between groups. Pharmacy costs per year was higher in Spanish patients than in immigrants (7351.8 versus 7153.9 euros [year 2005], P=.012). There were no differences in the total cost per patient per year between both groups. The global distribution of cost was very similar between both groups; almost 75% of the total cost was attributed to pharmacy in both groups.
ConclusionsThere are no significant differences in health resource utilisation and associated costs between immigrant and Spanish HIV patients.
La utilización y coste de los servicios sanitarios por parte de los pacientes inmigrantes con infección por VIH apenas se ha estudiado. Se evaluó la asistencia sanitaria y su coste directo asociado entre los pacientes con VIH españoles e inmigrantes.
MétodosSe incluyeron todos los pacientes adultos infectados por el VIH atendidos durante los años 2003-2005 (372 pacientes) en el hospital. Se evaluó el número de consultas, visitas a Urgencias (UR), a Hospital de Día (HD) y el número y duración de los ingresos. Se analizaron los costes directos. Se comparan todas las variables entre los inmigrantes y los españoles.
ResultadosLos inmigrantes representan un 12% (n = 43) de la cohorte. No hubo diferencias en el número de consultas, visitas a UR y HD por paciente entre ambos grupos. El número de ingresos por cualquier causa por paciente fue mayor en los inmigrantes que en los españoles, 1.3 (4.4) versus 0,9 (2,7), p = 0.034. Una alta proporción de consultas se realizaron en servicios diferentes de Infecciosas, tanto en los inmigrantes (45,1%) como en los españoles (43,0%). Los costes medios por paciente fueron similares en ambos grupos respecto a hospitalización, consulta y UR. El coste de farmacia por año fue mayor en los españoles que los inmigrantes (7.351,8 € frente a 7,153.9 € [€ año 2005], p = 0,012). No hubo diferencias en el coste total por paciente por año entre ambos grupos. La distribución total del coste fue muy similar entre ambos grupos; casi el 75% del coste total se atribuyó al tratamiento farmacológico en ambos grupos.
ConclusionesNo hay diferencias significativas relevantes en la atención sanitaria y coste asociado entre los pacientes con infección por VIH inmigrantes y españoles.
Immigration is a growing and relatively new phenomenon in Spain. HIV-infected patients born abroad are an increasing proportion of HIV patients treated in Spain. In some series, HIV-infected immigrants reach almost 50% of the new HIV diagnosis.1
It is well known that a highly active antiretroviral therapy reduces the incidence of opportunistic infections but its cost is high. Direct costs of HIV health care have been evaluated in the literature, especially after the introduction of HAART.2–4 It is assumed that immigrants may demand a higher use of healthcare services because of socio-economic vulnerability. However, the specific impact of the immigrant population with HIV infection on health services use and related cost has hardly been analysed.5,6 An understanding of healthcare use patterns is important for optimisation of care and resource allocation.
This study was designed to compare resource use patterns between immigrant and Spanish HIV-infected patients and to estimate the direct health care costs of HIV/AIDS care in both groups of patients.
Patients and methodsAll adult patients with HIV infection treated during the years 2003–2005 (from 01/01/2003 to 12/31/2005) in our institution were included. HIV patients were actively identified by electronic records. An immigrant was considered a patient not born in Spain. Basic epidemiological data were registered for each patient: sex, age, risk group, continent of origin, year of diagnosis of HIV infection, year of AIDS diagnosis, CDC classification at diagnosis of HIV, description of first opportunistic disease, and mean CD4 count and viral load during the period of the study.
The study was carried out in an urban secondary teaching hospital with 400 beds, in Madrid,. The hospital is the only public referral centre and serves a population of about 250,000 inhabitants. All types of HIV patients from this population are seen in our hospital. All major medical and surgical subspecialties are available on both an inpatient and outpatient basis, except for cardiac and thoracic surgery, and neurosurgery. To provide care of patients with HIV-infection, the hospital has an out-patient HIV clinic, and an inpatient ward attended by Infectious Diseases experts associated to Internal Medicine. Patients with HIV infection are hospitalised according to the same physicians who provide medical care in the out-patient clinic and they are treated during hospitalisation by the same clinicians. Specific physicians belonging to Emergency Room (ER) Department attend visits, and they occasionally decide admissions as well.
We analysed the health care data of the overall use of health-care resources and pharmaceutical costs during the period of the study. Specifically, we evaluated the number of out-patient visits, both scheduled and unscheduled, ER visits, visits to the Day-care Unit, out-patient surgery, and number and length of admissions. Clinical and health care information is registered in an electronic patient record. For the purpose of this study, an episode was defined as any of the following: admission, out-patient visit, ER visit, Day-care Unit visit, out-patient surgery and drug dispensation (Pharmacy). All admissions to hospital for patients with HIV were included, regardless of the admitting diagnosis. The clinical diagnosis corresponding to hospital admissions was coded according to DRG [All patient Diagnosis Related Groups (AP-DRGs) version 14th].
Out-patient visits were classified as first visit and successive visits. We included all out-patient visits (any speciality) and specific Infectious Diseases visits. Other available out-patient resources were Day-care Unit and out-patient surgery.
The Spanish healthcare system is open and free for all the population. Reimbursement is based on health care activity: each episode has an associated standardised cost according to disease severity and time involved. Antiretroviral therapy is available without charge.
The cost of individual out-patient visits was calculated by the officially assigned standard costs published by the Spanish Official Health Authorities during the period of the study. Fees for first visit were 69.45 € for the years 2003–4 and 81€ for 2005. Fees for successive visits were 41.7€ (years 2003–4) and 48.6€ (2005). Out-patient visits scheduled, but not performed were not included.
For the hospitalisation costs, a unitary cost for diagnostic related group (DRG) was calculated from the standardised assigned cost per admission (Hospital Cost Unit, HCU). The HCU is a specific Spanish measure of hospitalisation cost regarding case-mix.7 Case mix is a standard and international measurement of the types of cases being treated by a particular health care provider that is intended to reflect the patients’ different needs for resources. The use of these measurements allows comparison of performance and quality across organisations, practitioners, and communities. The HCU is calculated using the means of the number, type, and severity of illness of hospital admissions, and it is used for each hospital to allocate the cost of the admissions to the provider (Spanish Health Ministry or similar institution). Costs include the direct costs associated with patient care such as, physician fees, nursing care, laboratory and diagnostic testing, and supplies, equipment, etc. ER visits that ended as hospital admissions were included in the hospitalisation cost (HCU). The HCU fee for the study period was 1425.8€, 1578.1€ and 1741.0€ for the years 2003, 2004 and 2005, respectively.
Pharmacy cost was calculated by adding the unitary cost of each antiretroviral treatment dispensation every month. The cost of laboratory tests (CD4 cell count, viral load determination, serology and chemistry) was obtained from the standard rate. Total costs during the period of the study were calculated by adding the cost of each episode (hospitalisation, out-patient visit, ER visits, pharmacy, etc.) by year.
Unitary fees for ER were 80€ for the years 2003–4 and 102€ (2005); and for Day-care hospital 323€ (2003–4) and 393€ (2005). Cost per patient per year was calculated by adding the individual cost of each episode each year and dividing it by the total number of patients treated in the same period.
We performed a cost analysis from the health system perspective. In this study, only direct costs were included and the societal perspective was not considered.8
We compared all variables between immigrant and Spanish patients. CD4 count was stratified: <200; 201–500 and >500CD4cell/cc. Results are expressed by mean, standard deviation and percentage as appropriate, and compared using the chi-squared test for categorical variables, Student's t-test for quantitative variables, and Mann–Whitney test for non-parametric variables.
A multiple linear regression analysis was performed to estimate the effect of immigration on the total health spending. We did not find any interaction between variables, and a final model was constituted by immigrant status and all confounding variables. In addition, the standardised total spending was calculated with the means of the population and coefficients obtained in the multiple linear regression analysis.
ResultsA total of 372 patients were seen during the period of study, 88% (n=329) Spanish. They were 24% women, mean age 40.3 (7.8) years, and the most frequent risk group was illicit drug use (60%). At the diagnosis of HIV, a total of 23.7% had AIDS. The most frequent opportunistic diseases were extrapulmonary tuberculosis, pneumonia, and Pneumocystis jirovecii pneumonia. During the period of the study, patients had a mean CD4 count of 466.2 (307.6)cell/cc and viral load 2.4 (1.2)logcop/ml.
Immigrants represented 12% of the cohort (n=43), mean age 37.8 (11.5) years. The majority were women, 55.8%, and heterosexual transmission was the main risk group, 81.4%. The continents of origin were Africa 72%, Europe (East) 2.5%, and Central-South America 25.5%.
On the contrary, Spanish patients were more frequently men, 24%, (P<.001 for the comparison with immigrants), with a similar mean age, 40.5 (7.6) years (P=.311), and intravenous drug users, were the main risk group (65%).
Mean time with HIV infection was lower for immigrant 1.9 (2.3) years than Spanish patients 9.9 (6.0) years P<.001. Immigrants showed a trend to a higher proportion of AIDS at the diagnosis of HIV, 30.2% (P=.713). The most frequent opportunistic diseases for immigrants were pulmonary tuberculosis, extrapulmonary tuberculosis, HIV encephalopathy, and wasting syndrome. During the period of the study, immigrant patients had similar CD4 counts and viral loads to Spanish patients: CD4 count 423.0 (252.9)cell/cc and viral load 2.6 (1.3)log cop/ml.
The 372 patients generated a total of 9662 episodes of health resource use, 88.6% (n=8509) by Spanish and 11.4% (n=1102) by immigrant patients. All patients had more than one episode of health resource use after HIV diagnosis. Among the 9662 episodes, a very small number of them, n=158, corresponded to patients without HIV diagnosis at the beginning of the study, so we did not exclude these episodes from the analysis. In addition, fifty-one episodes were difficult to classify and were excluded.
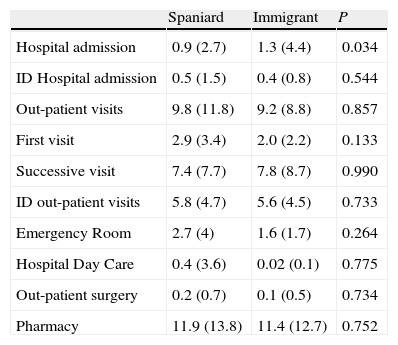
The number of hospital admissions per patient for any cause was higher in immigrants than in Spanish patients (Table 1). There were no differences in case-mix between immigrant and Spanish patients: mean case mix 2.2 (1.4) and 2.1 (1.5), respectively, P=.755. The most frequent DRGs in immigrant patients were 709 (major diagnosis HIV related with major multiple diagnosis related to tuberculosis), 710 (major diagnosis HIV related with major multiple diagnosis unrelated to tuberculosis) and 714 (HIV related significant diagnosis). In Spanish patients, the most frequent DRGs corresponded to 714, 710, 715 (HIV with other related diseases), and also 542 (bronchitis and asthma with major complications), 206 (hepatic disease) and 541 (respiratory diseases and asthma).
Use of health care resources per patient during the 3 years of study. Data represent the number of times (SD) that different health resources were used during the period of study. ID: Infectious Diseases. Pharmacy represents visits to Pharmacy.
| Spaniard | Immigrant | P | |
| Hospital admission | 0.9 (2.7) | 1.3 (4.4) | 0.034 |
| ID Hospital admission | 0.5 (1.5) | 0.4 (0.8) | 0.544 |
| Out-patient visits | 9.8 (11.8) | 9.2 (8.8) | 0.857 |
| First visit | 2.9 (3.4) | 2.0 (2.2) | 0.133 |
| Successive visit | 7.4 (7.7) | 7.8 (8.7) | 0.990 |
| ID out-patient visits | 5.8 (4.7) | 5.6 (4.5) | 0.733 |
| Emergency Room | 2.7 (4) | 1.6 (1.7) | 0.264 |
| Hospital Day Care | 0.4 (3.6) | 0.02 (0.1) | 0.775 |
| Out-patient surgery | 0.2 (0.7) | 0.1 (0.5) | 0.734 |
| Pharmacy | 11.9 (13.8) | 11.4 (12.7) | 0.752 |
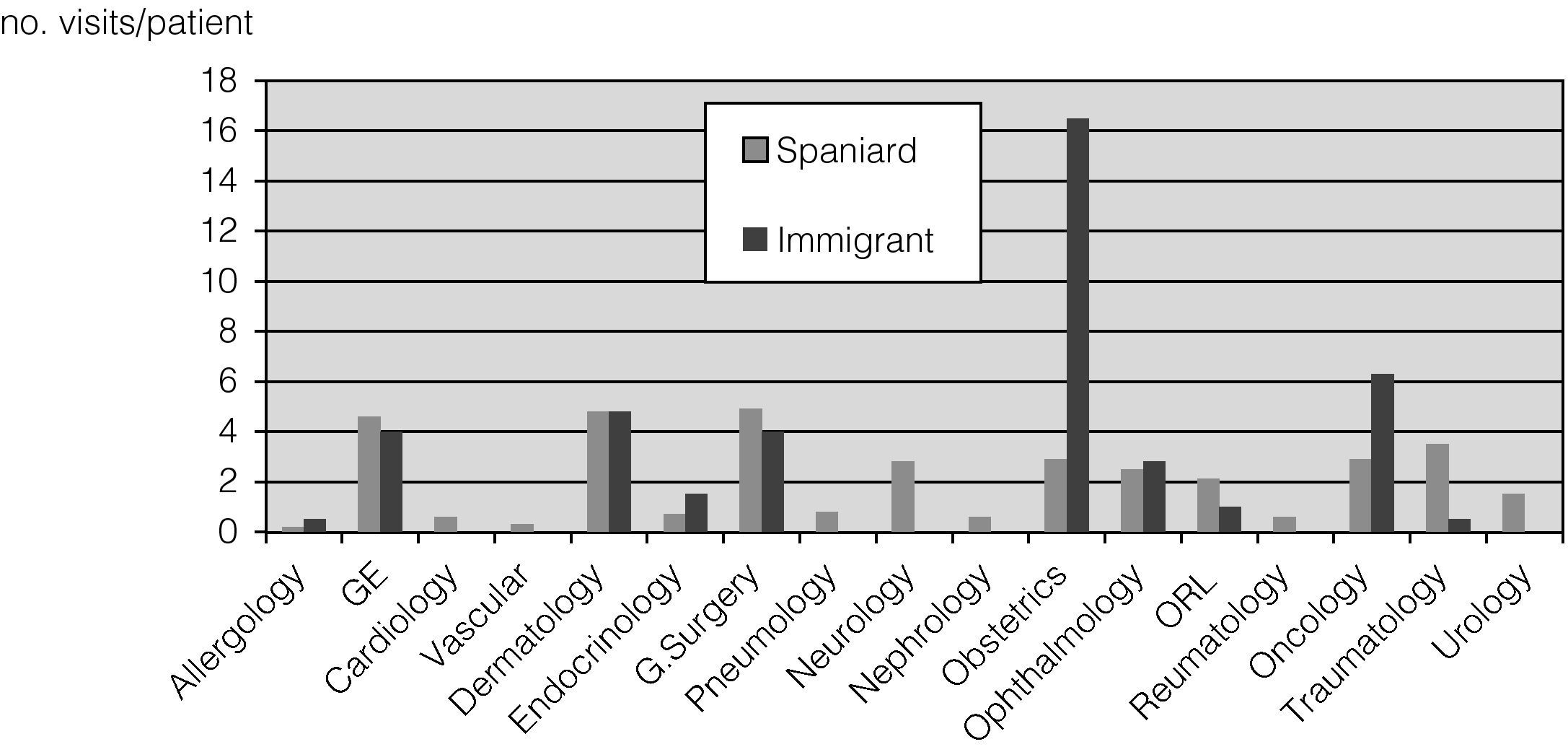
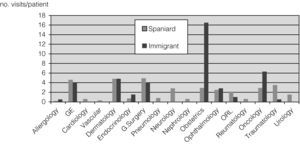
Regarding out-patient clinic visits, a high proportion of them (almost 50%), took place in services other than Infectious Diseases, both for immigrant (45.1%) and Spanish (43%) patients. However, there was a different pattern in the use of out-patient clinics; immigrants were more frequently seen in Obstetrics and Oncology, and Spànish patrients in Surgery, Dermatology and Gastroenterology (Fig. 1). There was no difference in the number of out-patient visits per patient between the groups (Table 1).
There was a tendency towards a lower number of ER visits per patient in immigrants but it was not statistically significant (Table 1). We did not find differences in the use of Day-care hospital and Out-patient Surgery (Table 1) and these resources were hardly used.
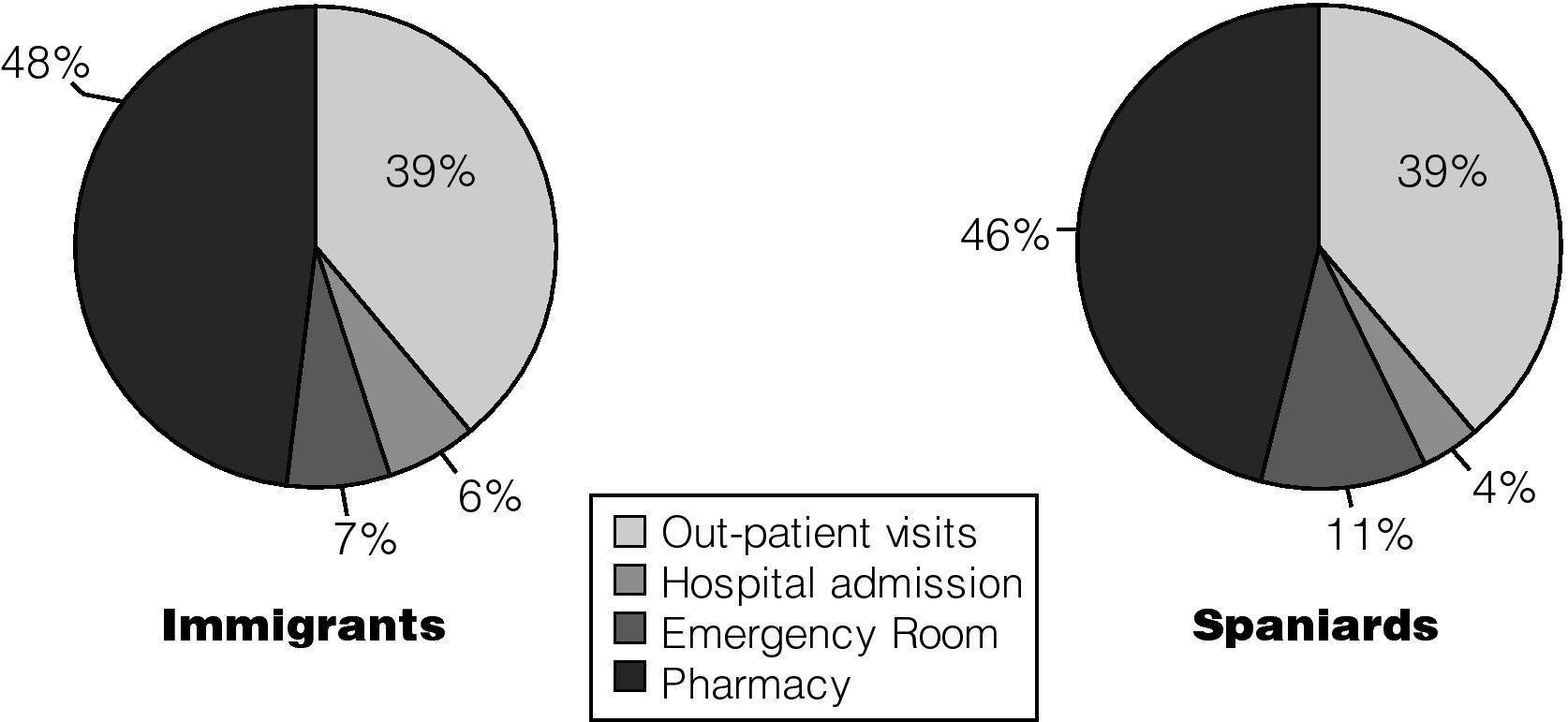
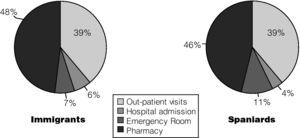
The proportional distribution of health resources usage in both groups was similar regarding Pharmacy visits (almost 50%) and out-patient visits (more than 35%), but hospitalisation was more used in immigrants (Fig. 2).
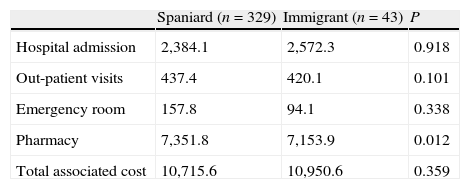
The mean unitary cost per admission was similar for Spanish and immigrant patients. In addition, there was no difference in the cost of out-patient visits and ER visits per patient between both groups. The cost of pharmacy per patient was slightly higher in Spanish than in immigrant patients (Table 2).
Cost per patient – year during the 3 years of study (€ 2005) according to the use of different health resources. Pharmacy includes all types of out-patient pharmacy drugs delivered at Hospital Pharmacy (virtually all HAART and Hepatitis C treatment).
| Spaniard (n=329) | Immigrant (n=43) | P | |
| Hospital admission | 2,384.1 | 2,572.3 | 0.918 |
| Out-patient visits | 437.4 | 420.1 | 0.101 |
| Emergency room | 157.8 | 94.1 | 0.338 |
| Pharmacy | 7,351.8 | 7,153.9 | 0.012 |
| Total associated cost | 10,715.6 | 10,950.6 | 0.359 |
There was no difference in the total cost per patient during the 3 years between immigrant (11,849€; 95% CI, 7173–15,056€) and Spanish patients (10,957€; 95%CI, 7015–14,899)€.
The difference in costs (not adjusted) attributed to immigrants was 893€ (95% CI, −3784 to 4099)€.
The adjusted overall cost for health care was 89.6€ cheaper for immigrants; 95% CI, −4710.4 to 4531.3; P=.969 (multiple linear regression analysis). Variables included in the final model were: sex, age, CD4 cell count, AIDS at diagnosis and time living with HIV infection.
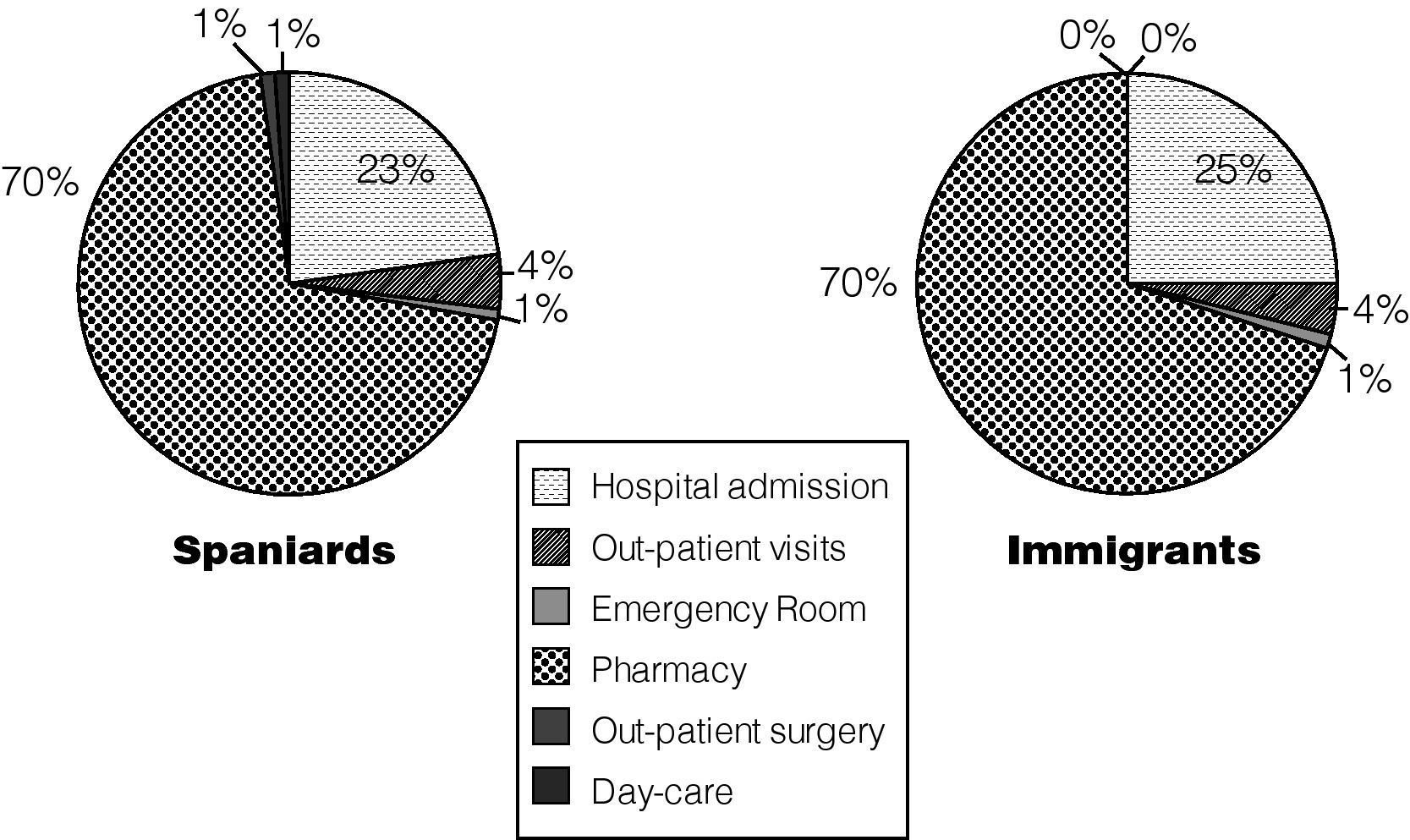
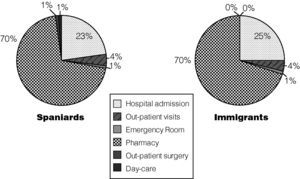
The overall distribution of cost was very similar between both groups, and almost 75% of the total cost was attributed to pharmacy in both groups (Fig. 3).
Distribution of global costs. Proportions represent the distribution of total spending for all concepts along the 3 years of the study. ER: Emergency Room. Pharmacy: Pharmacy includes all types of out-patient pharmacy drugs delivered at Hospital Pharmacy (virtually all HAART and hepatitis C treatment).
In the present study, we have analysed the distribution of resource use in immigrant and Spanish HIV patients, and we have not found large differences in the overall pattern of usage. It has been argued that immigrants make greater use of healthcare services, but there is a lack of published data to support this contention. Even though, some studies have indicated that health services use is lower among the immigrant population than among the host population.9–11 Our finding of similar healthcare use has special relevance as this fact contradicts the expectation that immigrant status leads to higher health resources consumption.
Access of care in Spain is public, free and universal, independently of nationality and length of residence. However, primary and specialised care presents several administrative barriers to irregular immigrants.
Hospital admissions were higher in immigrant than in the Spanish group (1.3 [4.4] versus 0.9 [2.7], P=.034). Several reasons may underlie the higher proportion of hospitalisation in immigrants. A lower perception of prevention, a delay in the diagnosis of HIV-AIDS (higher proportion of immigrants than Spanish presented with AIDS at the HIV diagnosis), and the use of health system when real symptoms arise.12–14
The most frequent diagnoses were related to HIV in both groups, although there were other reasons for hospitalisation more frequently in the Spanish group. As previously reported, in the HAART era, AIDS-defining conditions and diseases related to HIV continue to have the highest hospitalisation rate among the diagnosis categories examined.15,16 In the Spanish group, a significant proportion of hospitalisation was due to respiratory infections and hepatic diseases, as well stated in the literature.17 This result emphasises the importance of vaccination for pneumonia and influenza, as well as prophylaxis for P. jirovecii. In addition, hospitalisation for reasons other than AIDS conditions illustrates the importance of managing comorbid conditions in this population.
A similar case mix was noted between the immigrant and Spanish group. A possible confounding factor is that hospitalisations due to labour have a lower case mix, and are more frequent in immigrant patients.18
Immigrants exhibited a trend for a lower use of ER visits and their associated costs. Although the differences did not reach statistical significance, this should be interpreted with caution given the low number of ER visits.
Similar healthcare usage by the immigrant and the Spanish-born population may be attributable to the “survivor effect”, also known as the “healthy immigration effect”, according to which recently arrived immigrants have better health status than native-born residents.19
Similar to another published study, a cross-sectional Spanish National Health Survey, immigrants had similar diseases to those of the Spanish population but registered higher percentages of hospitalisation, although the investigators did not find evidence of excessive and inappropriate use of other healthcare resources.20 Similarly, in a case-mix study from Spain, the resource usage per discharge was lower among immigrants from low-income countries.21
An interesting finding in this work is the high proportion of use of health care resources other than from Infectious Diseases Unit in both groups. The clinical care of HIV patient has shifted to include a higher proportion of other classical medical specialities other than Infectious Diseases.7 Of note, we found a different distribution of the specialities, with a prevalence of Obstetrics in the immigrant, and diversified care in Spaniard patients. Epidemiological and social characteristics of the immigrant population22 explain these differences.
The Spanish patients showed a slightly higher pharmacy usage. This group of patients has a longer span of HIV infection, which means more time on HAART, and consequently use more expensive drug combinations. In spite of this, the total cost between the immigrant and Spanish group was similar, and time with HIV infection did not affect this result. Similar access to HAART for both immigrant and Spanish patients may be the explanation. It has been previously published that access to HAART by foreign HIV patients in Spain is similar to that of the Spanish population.23 Pharmacy made up two thirds of direct costs during the study, which balances the higher cost of hospitalisation in immigrants (23.5% of cost, Fig. 3). Similar figures have been shown in other European studies.24,25
An obvious limitation of our study is that immigrants are a mobile population and the total number of patients may change (actually increase). In any event, it is difficult to overpass the weight of pharmacy usage with an increase of hospitalisation by immigrants population. The number of patients is not high, but a complete recording of all health resource consumption was performed. We do no have data of entry into Spain, although we do register data of HIV infection diagnosis and AIDS. Immigrants with longer periods of stay in Spain may progress to a disease and consumption pattern similar to the Spanish-born population. Furthermore, subjects with a longer duration of HIV infection were not more likely to have higher costs, as assessed in regression analysis.
In conclusion, we did not find significant differences in total health resource consumption and associated cost between HIV immigrant and Spanish HIV patients. A high proportion of health care is provided by non-Infectious Diseases specialists in both groups. Our study provides data to help in provision of services to immigrant HIV patients.
FundingThe study was supported in part by a grant from FIPSE 36296/02 and FIPSE 36690/07 (Fundación para la Investigación y Prevención del SIDA en España), program of stabilisation of researchers 2007 from Instituto de Salud Carlos III (María Velasco) and funds from Instituto Madrileño de Salud, Comunidad Autónoma de Madrid.
Conflict of interestThe authors declare no conflict of interest.
We thank Dr Martin Ríos for critically reviewing the Methods section of the manuscript.