HIV Patient care should include psychological and psychiatric care, which is necessary for early detection thereof. Should suicidal ideation occur, refer the patient to a psychiatric unit. Pharmacological treatment is recommended when there is comorbidity with moderate or severe depression. You should look for the aetiology of neuropsychiatric disorder before using psychoactive drugs in HIV patients. The overall management of the health of HIV adolescents should include an assessment of mental health, environmental stressors and support systems. Training in the management of the patient both own emotions is critical to getting to provide optimal care.
These new guidelines updated previous recommendations regarding psychiatric and psychological disorders, including the most common pathologies in adults and children.
La atención al paciente VIH debe incluir la atención psicológica y psiquiátrica para lo cual es necesario realizar su detección precoz. En caso de ideación suicida, remitir al paciente a una unidad de psiquiatría. Se recomienda el tratamiento farmacológico cuando hay comorbilidad con depresión moderada o severa. Se debe buscar la etiología del trastorno neuropsiquiátrico antes de usar psicofármacos en los pacientes VIH. El manejo global de la salud de los adolescentes VIH debe incluir una valoración de la salud mental, estresores ambientales y sistemas de apoyo. El entrenamiento en el manejo de las emociones tanto propias como del paciente es fundamental para conseguir proporcionar una asistencia óptima.
En este documento se actualizan las recomendaciones previas respecto a alteraciones psiquiátricas y psicológicas, incluyendo las patologías más frecuentes tanto en adultos como en niños.
Mental patient's particular features will have an influence on the development of the HIV-infection. Moreover, many of these patients live in a precarious social and economic position and are part of vulnerable populations. Therefore, these particular patients must receive multidisciplinary care, involving mental health specialists, internist-infectologists and different support services.1 The existence of an appropriate relationship between the patient, his or her family and the care team is also essential.
Recommendations
- 1.
HIV-patient care should include psychological and psychiatric care (strong recommendation, high quality evidence).
- 2.
Basic principles of the aforementioned care are listening and support, confidentiality, establishing a good therapeutic bond, psychoeducation, and coordinating and adjusting the different care settings (strong recommendation, high quality evidence).
- 3.
Early detection and treatment of psychiatric and psychological disorders are necessary (strong recommendation, high quality evidence).
Emotional responses must be detected primarily by health professionals to be able to perform a proper assisted counselling depending on the observed reaction, or in the absence thereof, make an appropriate referral to other services (e.g., psychology, psychiatry) or to organizations working with HIV patients.
Recommendation
- 1.
It is recommended that care for newly HIV-diagnosed patients includes psychological care, being its basic principles listening and support, confidentiality, psychoeducation, and coordinating and adjusting the different care settings (strong recommendation, low evidence level).
Psychopathological examination should assess the patient's orientation and the condition of his/her higher functions, as well as his/her behaviour, appearance and insight (medical and psychiatric). It should include questions about mood, anxiety level, thought, possible sensory perception disorders (hallucinations) and motor skills.
Recommendation
- 1.
When approaching any HIV-patient who shows a first psychiatric episode, organic causes should always be considered in the first place: delirium, cognitive impairment, substance abuse, secondary processes to systemic diseases or of the CNS's, etc (strong recommendation, moderate quality evidence).
In case of any life event, such as the notification of the diagnosis of infection, there may be an emotional response, which usually shows up as depression or anxiety. If this emotional response is excessive to what might be expected, it is called an adjustment disorder. One of the most severe complications of this reaction is the appearance of suicidal ideation.
Therefore, it is essential to be alert for any suicidal thoughts and refer the patient to a psychiatric unit. The treatment of choice is psychotherapy. The type of psychotherapy which has proved to be most effective is cognitive behavioural. Psychoactive drugs to be used are anxiolytics or antidepressants, depending on the predominance of anxiety or depression.
Recommendations
- 1.
One of the most severe complications of this reaction is the appearance of suicidal ideation. Therefore, it is essential to be alert for any suicidal thoughts and refer the patient to a psychiatric unit (strong recommendation, high quality evidence).
- 2.
The type of psychotherapy which has proved to be most effective is cognitive behavioural. Psychoactive drugs to be used are anxiolytics or antidepressants, depending on the predominance of anxiety or depression. Anxiolytics treatment should not be longer than two months (strong recommendation, moderate quality evidence).
Mood disorders include depression and dysthymia (basically differing in intensity and duration of symptomatology), mania (heightened mood) and bipolar disorder (with appearance of a manic episode, with or without previous depressive episode). It is recommended for the treatment of mania and bipolar disorder to refer the patient to a psychiatrist and to provide antipsychotics and mood stabilizers (lithium or valproic acid) while taking great care to control plasma levels of these drugs. Antidepressants and psychotherapy are used for the treatment of depression and dysthymia. The use of SSRI is recommended as first choice antidepressants. In case of association of anxiety or insomnia, it is recommended to add one benzodiazepine or to choose a sedative antidepressant.
Recommendations
- 1.
Depressive symptomatology should always be examined and an appropriate treatment should begin in case of a depressive episode (Strong RECOMMENDATION, low quality evidence).
- 2.
The use of antidepressants and psychotherapy is recommended for the treatment of depression and dysthymia. The use of SSRI is recommended as first choice antidepressants (strong recommendation, high quality evidence).
- 3.
In case of association of anxiety and insomnia, it is recommended to add one benzodiazepine or to choose a sedative antidepressant (strong recommendation, low quality evidence).
- 4.
In case of maniform symptomatology, and having ruled out a possible organic origin, it is recommended to urgently refer the patient to the reference psychiatrist (strong recommendation, low quality evidence).
There are different diseases that are accompanied by anxiety, such as posttraumatic stress disorder, obsessive-compulsive disorder, generalized anxiety disorder, social phobia or other specific phobias and panic disorder. Anxiety symptoms can also appear in association with a depressive disorder. Pharmacological treatment is recommended in cases of comorbidity with moderate or severe depression. Therapeutic measures include common healthy actions, psychotherapy (especially cognitive-behavioural oriented, counselling and support groups and self-help) and pharmacological treatment. SSRI are first-line drugs for the treatment of generalized anxiety disorders, social phobia, obsessive-compulsive disorders and posttraumatic stress. Benzodiazepines are the choice in acute conditions, severe anxiety and during short periods of time (between 2 and 6 weeks). However, they should always be used with caution and even be avoided in some patients because of pharmacological interactions, sensitivity to side effects in HIV patients and risk of habituation.
Recommendations
- 1.
Pharmacological treatment is recommended in cases of comorbidity with moderate or severe depression (strong recommendation, low quality evidence).
- 2.
SSRI are first-line drugs for the treatment of generalized anxiety disorders, social phobia, obsessive-compulsive disorders and posttraumatic stress. To assess the efficiency of SSRI it is necessary that pharmacological treatment with these drugs is maintained at least for 12 weeks, and if there has been any response at 12 weeks, it should be continued during 6 more months (strong recommendation, high quality evidence).
- 3.
Withdrawal of efavirenz should be assessed in patients with suicidal ideas or previous suicide attempts (strong recommendation, moderate quality evidence).
- 4.
Benzodiazepines are the choice in acute conditions, severe anxiety and during short periods of time (between 2 and 6 weeks). However, they should always be used with caution and even be avoided in some patients because of pharmacological interactions, sensitivity to side effects in HIV patients and risk of habituation (strong recommendation, moderate quality evidence).
- 5.
Psychological treatments are also useful as single or complimentary treatments (strong recommendation, high quality evidence).
Personality disorders are defined as a consistent pattern of internal experience and behaviour which diverges from the expectations of the subject's culture and which appears in two or more of the following areas: cognition, emotion, interpersonal relationships or impulse control.
Basically, there are three different groups of personality disorders:
- •
Group or cluster A or eccentric disorders (paranoid, schizoid and schizotypal);
- •
Group B or disorders characterized by exaggerated dramatization and severe behavioural disorders (antisocial, limit, histrionic and narcissist);
- •
Group C or anxious personality disorders (avoider, dependent and obsessive-compulsive).
Group B diseases are the most frequents in HIV patients, especially antisocial and limit. Regarding the treatment of personality disorders, it is recommended to apply a treatment that combines psychotherapy and pharmacological therapy, limiting the latter to symptomatic management.
Recommendations
- 1.
Regarding the treatment of personality disorders, it is recommended to apply a treatment that combines psychotherapy and pharmacological therapy, limiting the latter to symptomatic management (strong recommendation, high quality evidence).
- 2.
It is essential to consider hospitalization of HIV patients if there is suicidal or self-injurious risk (strong recommendation, high quality evidence).
Psychotic disorders are characterized by a combination of symptoms, which share the loss of judgement about reality: hallucinations (visual, auditory and corporal), delirious ideas (believing unreal things with full conviction) and ego feeling disorders (thoughts transmission and reading), which causes great anxiety for the individual.
Drugs of choice are atypical antipsychotics or second generation: clozapine (contraindicated with ritonavir), risperidone (increases its levels with ritonavir), olanzapine (decreases its levels with ritonavir), quetiapine (PI inhibit their metabolism and increase their toxicity, therefore their association is contraindicated. Non-nucleosides efavirenz, nevirapine and etravirine induce their metabolism and may reduce their efficacy), ziprasidone and aripiprazole (their interaction is comparable to that of quetiapine, however these are not contraindicated with PI), and amisulpride (low risk of interaction).
Recommendations
- 1.
The possible organic origin of psychotic symptoms should be taken into account. If there is no organic pathology, a pharmacologic or drug origin should be considered. Psychiatric pathology should be taken into account once the aforementioned origins are ruled out (strong recommendation, low quality evidence).
- 2.
It is recommended to carry out a brain-imaging test (cranial CT or brain MR) on patients who show a psychotic episode for the first time. In case of psychotic symptomatology it is necessary to immediately start a treatment with antipsychotic drugs. It is also advisable to hospitalize the patient to be able to carry out a proper differential diagnosis and adjust the treatment properly. It is recommended to be cautious with pharmacological treatment: start with low doses, maintain them the shortest period of time, and watch interactions and side effects (strong recommendation, low quality evidence).
Identification of nutritional disorders will assess if the aetiology of the disorder is organic, toxic or psychological or if it is an established disorder of nutritional behaviour. Every time emotional alterations are detected in the context of a nutritional disorder, it is recommended to refer the patient to a clinical psychologist and psychiatrist for assessment and treatment.
Sleep disorders are highly prevalent in HIV infected patients and include insomnia, hypersomnia and parasomnia, however the first one is the most common. Psychological treatment with cognitive behavioural orientation and pharmacological etiopathogenic treatment complete the therapeutic approach. The most broadly used psychoactive drugs are benzodiazepines. Efavirenz is a drug that is commonly associated with sleep alterations, especially during the first weeks of the treatment. In some patients, the first measure to treat insomnia should be the replacement of the aforementioned drug by an alternative.
The most common sexual disorders in HIV patients are erectile dysfunction and impotence in men and inhibited sexual desire in both men and women. The appropriate treatment is the multidisciplinary combination of organic, psychological and relational. In case of detection of sexual disorders, it is recommended to refer the patient to a sexologist, clinical psychologist or psychiatrist for a proper diagnosis and intervention, always in coordination between them.
Recommendations
- 1.
Every time emotional alterations are detected in the context of a nutritional disorder, it is recommended to refer the patient to a clinical psychologist and psychiatrist for assessment and treatment (strong recommendation, low quality evidence).
- 2.
Regarding sleep disorders, the professional should ask about lifestyle and environment factors, examine their relative contribution to insomnia and make the necessary recommendations. Even factors that may seem obvious should be taken into account (Weak recommendation, low quality evidence).
- 3.
In patients being treated with efavirenz, insomnia may be a justified cause for the withdrawal of this drug (strong recommendation, high quality evidence).
- 4.
In case of detection of sexual disorders, it is recommended to refer the patient to a sexologist, clinical psychologist or psychiatrist for a proper diagnosis and intervention, always in coordination between them (weak recommendation, low quality evidence).
Confusional syndrome or delirium is considered a medical emergency that requires a physical examination with neurological exploration, medical history and mental examination and laboratory tests to detect its cause. To treat it, its cause must be identified and treated specifically. It is recommended to identify the aetiology of the neuropsychiatric disorder before using psychoactive drugs in HIV patients. In states of agitation that require sedation, it is recommended to use antipsychotics such as haloperidol or risperidone first.
Recommendations
- 1.
It is recommended to identify the aetiology of the neuropsychiatric disorder before using psychoactive drugs in HIV patients (weak recommendation, low quality evidence).
- 2.
In states of agitation and delirium that require sedation, it is recommended to use antipsychotics like haloperidol or risperidone first (strong recommendation, moderate quality evidence).
Treatment for substance use disorder is useful for both primary and secondary HIV prevention.
UPS therapeutic approach is complex because it does not only have to consider addiction, but it also has to take into account family, social and employment implications.
General practitioner's or any non-specialist's fundamental role in substance abuse is detecting their use and referring to centres specialized in drug addiction, where the problem can be addressed in greater depth. An essential first step is to identify the patient's motivation to change.
Main treatments are based on psychological therapies and individual, group, social and family support therapies. Pharmacological treatment has proven to be efficient fundamentally in alcohol and opioids dependency. Lamotrigine has been considered for cocaine use in HIV patients. A study suggests that naltrexone and mirtazapine could be beneficial for cocaine and amphetamines use.
Recommendations
- 1.
It is recommended to transmit risk behaviour prevention messages in every medical visit in the context of substance use (weak recommendation, low quality evidence).
- 2.
UPS treatment should be individualized, combining different strategies (counselling, individual/social and family psychotherapy and pharmacological treatment) (weak recommendation, low quality evidence).
- 3.
Interventions should be maintained in time and coordinated between different services (medical, social healthcare, legal…) (weak recommendation, low quality evidence).
HIV diagnosis represents an emotional impact that requires a comprehensive and continuous assessment where not only biological aspects, but also psychological and social aspects, have to be taken into account. The goal of this assessment is to alleviate suffering and improve quality of life.
The professional should try to detect initial emotional responses and behaviour derived from the diagnosis and to evaluate signs that require a specialized intervention in Mental Health.
The way, time and place of diagnosis communication have a decisive influence in patients’ reaction. Diagnosis should be communicated individually and confidentially, dedicating the necessary time to evaluate the emotional state and allow the patient to explain his/her concerns and fears.
Any psychotherapeutic intervention, whether from an individual, group or family approach, is important for a positive clinical course of HIV infection. Evidence supports that psychotherapeutic interventions are more effective than pharmacological interventions, at least in low/moderate intensity depressive disorders.
Recommendations
- 1.
Psychological support can be performed by different health professionals and should start with diagnosis. For communication to be effective, it should comply with the general principles of “good communication” (strong recommendation, high quality evidence).
- 2.
Psychological interventions, particularly the ones that include cognitive behavioural techniques (cognitive restructuration and stress management techniques) have proved to be effective both to decrease depressive symptomatology and anxiety and to improve confrontation with stressors associated with HIV infection (strong recommendation, moderate quality evidence).
- 3.
Interventions aimed at specific topics of HIV infection like risk reduction and prevention and adherence to antiretroviral treatment have shown promising but not conclusive results (strong recommendation, low quality evidence).
General guidelines, especially applicable in HIV patients in symptomatic state, include:
- 1.
Administration of lower doses initially and slower increase.
- 2.
Least complex dosage programming.
- 3.
Taking into account the side effects profile to prevent unnecessary adverse events.
- 4.
Considering metabolic pathways and of drug elimination to reduce to a minimum both interactions between medications and damage to target organ.
Studies about their efficacy and clinical trials indicate that antidepressants are usually well tolerated by HIV patients, even those with symptomatic HIV infection.
Antipsychotics and mood stabilizersAdministration of antipsychotics to patients in advanced stages of HIV infection is associated with an increase in the impact of extrapyramidal side effects (stiffness, hypokinesia and dystonia). High potency neuroleptic medication (haloperidol is the most used in published studies) has a greater tendency to cause extrapyramidal side effects.
Atypical antipsychotic drugs or second generation (clozapine, risperidone, paliperidone, sertindol, olanzapine, ziprasidone, quetiapine and aripiprazole) have a similar efficacy and lower tendency of causing extrapyramidal side effects.
Antipsychotic treatment of choice is paliperidone, given its lower risk of extrapyramidal side effects, low risk of pharmacokinetic interactions and lower risk of causing metabolic syndrome in respect to other antipsychotics.
Some of them (clozapine, olanzapine and quetiapine) may cause metabolic syndrome.
Regarding clozapine, it is especially necessary to supervise it in HIV+ patients, given the risk of agranulocytosis. There is also a risk of epileptic seizure, especially when combined with ritonavir because the latter can inhibit different cytochrome P450 isoenzymes involved in clozapine's metabolism. The association of clozapine with protease inhibitors enhanced with ritonavir is contraindicated.
Anxiolytics and other hypnotic sedative drugsBenzodiazepinesIt is preferable to avoid this type of medication in patients with alcohol dependency and in those that have substance abuse history.
If certain benzodiazepines with cytochrome P450s isoenzyme 3A inhibitors are administered, a reduction in the elimination of benzodiazepine with the resultant increase in sedation has to be expected, which could even cause respiratory depression. Loracepam is the only benzodiazepine metabolized only by glucuronidation commercialized in Spain.
Gabapentin and pregabalinPregabalin is indicated for anxiety disorder. These drugs have low risk of pharmacologic interaction, because they are not metabolized. Some studies point out their usefulness in HIV+ patients with neuropathic pain.
Zolpidem and zopicloneThese are used as hypnotics.
Alternative treatmentsTo treat symptoms such as insomnia, depressed mood, fatigue or neurocognitive deficit
HIV patients tend to take substances called “natural” or alternative medicines. Hypericum perforatum (St. John's wort), valerian, S-adenosylmethionine (SAM-e), melatonin, Gingko biloba and kava-kava are some of these substances. It has been proven that St. John's wort contains a substance with a powerful inducer effect of cytochrome P450s isoenzyme 3A and may therefore reduce plasma concentrations and effectiveness of certain antiretroviral medication.
Recommendations
- 1.
In general terms, it is recommended: (strong recommendation, low quality evidence):
- a.
Administration of lower doses initially and slower increase.
- b.
Least complex dosage programming.
- c.
Taking into account the side effects profile to prevent unnecessary adverse events.
- d.
Considering metabolic pathways and of drug elimination to reduce to a minimum both interactions between medications and damage to target organ.
- a.
- 2.
Psychopharmacologic treatment of depression in HIV+ patients should apply Adams & co.’s measurement-based care (MBC) (strong recommendation, moderate quality evidence).
- 3.
Treatments of choice for depression are selective serotonin reuptake inhibitor antidepressants (strong recommendation, high quality evidence).
- 4.
Antipsychotic treatment of choice is paliperidone, given its lower risk of extrapyramidal side effects, low risk of pharmacokinetic interactions and lower risk of causing metabolic syndrome in respect to other antipsychotics (weak recommendation, moderate quality evidence).
- 5.
Use of benzodiazepines in patients with history of alcohol and substance use disorder should be avoided (strong recommendation, moderate quality evidence).
- 6.
It is not recommended to simultaneously administer St. John's wort and protease inhibitors or non-nucleosides reverse transcriptase inhibitors to treat depression (strong recommendation, high quality evidence).
In general, many psychoactive drugs have hepatic metabolism mediated by cytochrome P450 and studies available are scarce. As a general rule, in case of prescription of any psychoactive drug to a patient receiving antiretroviral treatment it is recommended to start the treatment with low doses and increase them slowly until reaching the desired clinical effect. It is recommended to review contraindicated or non-recommended associations with psychoactive drugs. Metabolism of antiretroviral drugs and their inducer and inhibitor effect, as well as contraindications with other drugs, can be looked up in detail on GESIDA's Consensus Document/National Plan about AIDS regarding retroviral treatment in adults with human immunodeficiency virus infection.
The reader is advised to consult the different available web pages about pharmacological interactions, including the following:
Recommendations
- 1.
All medication (antiretroviral, psychoactive drugs and others), natural products and alternative medicines the patient are taking should be registered in his/her clinical history to assess possible interactions among them (strong recommendation, moderate quality evidence).
- 2.
Contraindications should be taken into account and adjust the corresponding doses when necessary (strong recommendation, high quality evidence).
- 3.
Monitoring of plasma levels should be considered when possible when administering two or more medications with possible relevant pharmacokinetic interactions to avoid toxicity or therapeutic inefficiency (strong recommendation, moderate quality evidence).
- 4.
When using psychoactive drugs with narrow therapeutic margin (like tricyclic antidepressants) or that may produce high toxicity (like prolongation of the QT interval) together with antiretroviral drugs that may increase plasma levels (in general, HIV protease inhibitors or elvitegravir/cobicistat) it is recommended to start the treatment with low doses of psychoactive drug and increase them on a very gradual basis depending on efficacy/tolerability (strong recommendation, moderate quality evidence).
Currently, neurocognitive functioning impairment is a frequent complication in HIV infection. The most popular form of cognitive decline is HIV-associated dementia (HAD), which represents the most severe disorder. Two other milder disorders have been defined: asymptomatic neurocognitive impairment (ANI) and mild neurocognitive disorder (MND).
Neuropsychological exploration is the necessary assessment method for HIV-associated neurocognitive disorder diagnosis. Nevertheless, other methods are essential to reach this diagnosis, such as daily functioning assessment, ruling out other comorbidities, or emotional state assessment, basically including depressive and anxiety symptoms.
Recommendations
- 1.
In view of neurocognitive impairment symptoms, a neurocognitive screening proved in HIV population should be performed. In case of a positive result, and having ruled out other comorbidities, it is advised to perform a complete neuropsychological exploration (strong recommendation, moderate quality evidence).
- 2.
Complete neuropsychological exploration should be performed by a specialized professional, who will basically conduct a set of validated and standardized neuropsychological tests with which he/she will be able to determine the existence of a neurocognitive impairment (strong recommendation, high quality evidence).
- 3.
Recommended cognitive domains for the neuropsychological exploration are the following: attention/working memory, speed of information processing, verbal memory, learning, executive function, verbal fluency and motor function. Results in these domains should always offer standardized scores, depending on availability of normative data and basically according to age, sex and education level (strong recommendation, high quality evidence).
- 4.
The existence of cognitive impairment will be considered when: (a) there is a score in a standardized test lower than, at least, one standard deviation, lower than the average in at least 2 cognitive domains; (b) lack of delirium or causes previous to the HIV infection that may have caused the cognitive impairment are ruled out; and (c) interference in daily life functioning is assessed, which is basically useful to differentiate between asymptomatic neurocognitive impairment (ANI) and mild neurocognitive disorder (MND) (strong recommendation, low quality evidence).
- 5.
It is necessary to differentiate between the existence of cognitive impairment caused by the virus's own activity or, instead, by the influence of other risk conditions, or both. This may sometimes be difficult, depending on the patient's clinical history. However, it is essential to at least perform a differential diagnosis where other causes that may be causing the cognitive impairment are assessed (strong recommendation, high quality evidence).
A greater prevalence of psychopathological diseases has been detected in children who have acquired the infection perinatally than in general population not infected by HIV.
Most prevalent diagnostics are: anxiety disorders (40%) which include social phobia, separation anxiety, agoraphobia, generalized anxiety disorder, obsessive compulsive disorder and specific phobias, attention deficit hyperactivity disorder (21%), behavioural disorders (13%) and oppositional defiant disorder (11%).
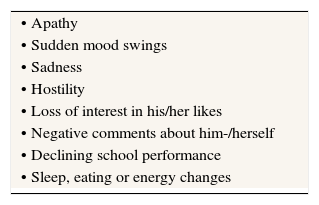
Referral to mental health should be assessed in the following situations: school conflicts, interpersonal conflicts, parents’ illness or loss of significant persons or in case of appearance of the following symptoms (Table 1).
The infection's disclosure should start prematurely and always before adolescence (crisis stage). Spanish and English guides recommend starting before 9 years of age. However, it will possibly start a little later in boys than in girls, because of man's developmental delay component. The paediatrician will take an active role, encouraging and advising the family in this process. He/she will also assess the necessity of family psychological support in cases with difficulties (resistance to disclosure).
Keeping the diagnosis in secret causes psychological stress and interferes in the appropriate confrontation of the disease. Communicating the diagnosis to significant persons increases social support and improves adherence. Adolescents must know and consider the benefits and potential costs of communicating the diagnosis. Given the difficulty and complexity of this topic, it is advised to give psychological support oriented to the development of specific confrontation strategies.
Transition; switching to the adults doctor officeTransition programmes have shown to be effective in improving assistance, adherence, morbidity/mortality and patient's and carer's satisfaction.
There is neither an established chronological age to perform the transition nor a specific transition model.
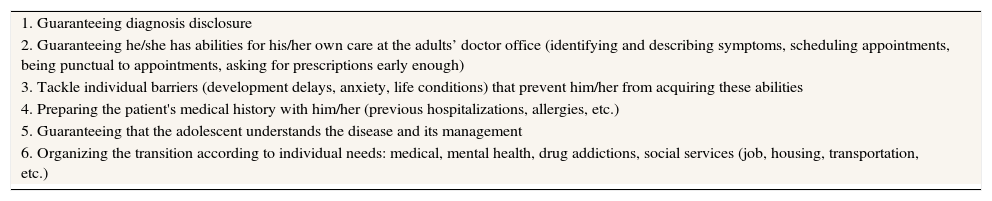
Transition should be a deliberate and planned process that will start at the paediatric office, at least two years before this transfer, and will be aimed at the patient's medical and psychosocial needs (Table 2).
Transition plan from children to adults doctor office.
| 1. Guaranteeing diagnosis disclosure |
| 2. Guaranteeing he/she has abilities for his/her own care at the adults’ doctor office (identifying and describing symptoms, scheduling appointments, being punctual to appointments, asking for prescriptions early enough) |
| 3. Tackle individual barriers (development delays, anxiety, life conditions) that prevent him/her from acquiring these abilities |
| 4. Preparing the patient's medical history with him/her (previous hospitalizations, allergies, etc.) |
| 5. Guaranteeing that the adolescent understands the disease and its management |
| 6. Organizing the transition according to individual needs: medical, mental health, drug addictions, social services (job, housing, transportation, etc.) |
The transition team will be a multidisciplinary team composed by the paediatrician, the reference adult specialist, psychology, social work and nursing.
The transition will be considered successful when the patient has accepted he/she has a chronic disease, has learned the necessary abilities for his/her own care and has adjusted to the adult healthcare system with proper adherence.
Recommendations
- 1.
The paediatrician's office will need to have a screening instrument that allows the quick detection of psychopathologies to refer to mental health (weak level and moderate quality evidence).
- 2.
Global management of HIV adolescents’ health should include an assessment of mental health, environmental stressors and support systems (weak level and moderate quality evidence).
- 3.
During adolescence, the existence of a non-treated psychopathology will prevent the appropriate adherence to the treatment (weak level and moderate quality evidence).
- 4.
It is important to include an assessment of the neuropsychological state in the paediatric follow-up (weak level and moderate quality evidence).
- 5.
Diagnosis disclosure should start prematurely, before adolescence. The explanation of the disease will be adjusted to the patient's age and cognitive maturity (weak level and moderate quality evidence).
- 6.
Transition should be a deliberate and planned process that will start at the paediatric office and will be aimed at the patient's medical and psychosocial needs (weak level and moderate quality evidence).
The well-known burnout syndrome basically affects people working for and in contact with other people and, especially, social and healthcare professionals.
Interventions based on cognitive behavioural approaches and mindfulness techniques (training full attention focused on the present) have had a lot of success to decrease anxiety and stress levels both for medical and nursing staff. In particular, mindfulness programmes have been one of the interventions that have generated a larger number of studies and that have produced the most renowned benefits, both in diminishing burnout as well as in increasing wellbeing, job satisfaction and professionalism.
Recommendations
- 1.
In case of burnout, cognitive behavioural intervention and mindfulness techniques can help decrease anxiety and depression levels, as well as burnout (strong recommendation, high quality evidence).
- 2.
It is important that both health professionals individually as well as social and healthcare teams perform self-assessments aimed at detecting possible burnout situations, which are negative for them and for their patients (strong recommendation, low quality evidence).
- 3.
Training in managing both own and patients’ emotions is essential to be able to provide optimum care (strong recommendation, low quality evidence).
This document was financed with funds from the National Public Health System.
Conflict of interestIn order to avoid and/or minimize potential conflicts of interest, people form the panel of experts/as have made a formal declaration of interest. In this statement the authors have received funding to participate in conferences and to conduct research and have received payments as speakers by public institutions and pharmaceutical companies. These activities do not affect the clarity of this document by no conflict of interest with fees recommended and/or grants received. Significantly regarding drugs in document speaks only active ingredient and no trademark.
The National Plan on AIDS and the boards of the participating scientific societies, appreciate the contributions and opinions of: Juan Emilio Losa and Carlos Duenas, who have contributed to improve the wording and enrich the content of the document.
List of members of Experts Panel from the Secretary of the National AIDS Plan (SPNS), Spanish Society of Psychiatry (SEP), AIDS Study Group (GeSIDA), and Spanish Society of Pediatric Infectious Diseases (SEIP) are listed in the Appendix.
Writing Committee: Rosa Polo. Especialista en Medicina Interna. Secretaría Plan Nacional sobre el Sida. Madrid. Jordi Blanch. Especialista en Psiquiatría. Servicio de Psiquiatría y psicología. Hospital Clínico. Barcelona. Jaime Locutura. Especialista en Medicina Interna. Hospital Universitario de Burgos. Piedad Arazo. Especialista en Medicina Interna. Unidad de VIH. Hospital Miguel Servet. Zaragoza. Pablo Bachiller. Especialista en Medicina Interna. Consulta de Enfermedades. Infecciosas. Hospital Universitario Rio Hortega. Valladolid. Carmen Bayon. Especialista en Psiquiatría. Hospital Universitario La Paz. IdiPaz. Madrid. Vicente Estrada. Especialista en Medicina Interna. Unidad de VIH. Hospital Clínico Universitario. Madrid. Jose Luis Fernández. Especialista en Psiquiatría. Servicio de Interconsulta del Complejo Hospitalario Universitario de Vigo. Carmina Fumaz. Especialista en Psicología Clínica. Hospital de Día de VIH. Hospital Universitario Germans Trias i Pujol. Badalona. Mª José Galindo. Especialista en Medicina Interna. Unidad de VIH. Hospital Clínico Universitario. Valencia. Maribel Gonzalez Tomé. Especialista en Pediatría. Hospital 12 de Octubre. Madrid. Jose Antonio Iribarren. Especialista en Medicina Interna. Unidad de VIH. Hospital Universitario de Donostia. San Sebastian. Fernando Lozano. Especialista en Medicina Interna. Unidad Clínica de Enf. Infecciosas y Microbiología. Hospital Universitario de Valme. Sevilla. Ana Mariño. Especialista en Medicina Interna. Unidad de Enfermedades Infecciosas. Complejo Hospitalario Universitario de Ferrol. Mª José Mellado. Especialista en Pediatría. Hospital Universitario La Paz. Madrid. Jose A. Muñoz-Moreno. Psicólogo Clínico y de la Salud. Fundación Lucha contra el SIDA - Hospital Universitario Germans Trias i Pujol. Badalona (Barcelona). Maria Luisa Navarro. Especialista en Pediatría. Hospital Universitario Gregorio Marañon. Madrid. Ricard Navinés. Especialista en Psiquiatría. Servicio de Psiquiatría y Psicología Hospital Clínico. Barcelona. Juan Francisco Pérez Prieto. Especialista en Psiquiatría. Servicio de Psiquiatría Hospital clínico Universitario. Valencia. Agueda Rojo. Especialista en Psiquiatría. Unidad de Hospitalización Psiquiátrica del Complejo Hospitalario Universitario de Vigo. Araceli Rousaud. Especialista en Psicología. Servicio de Psiquiatría y Psicología Hospital Clínico. Barcelona. Jesús Sanchez Hernandez. Especialista en Psicología Clínica. Hospital Universitario de Burgos. Jesús Santos. Especialista en Medicina Interna. Unidad de VIH. Hospital Universitario Virgen de la Victoria. Málaga Montse Tuset. Farmacéutica. Servicio de farmacia del Hospital Clínico. Barcelona.