Patients with HIV infection have a higher cardiovascular risk than the general population. The identification of patients with high CVR, the implementation of preventive measures and the control of modifiable risk factors, especially in patients on antiretroviral therapy should be part of the management of HIV infection.
This document updates the recommendations published in 2014, mainly regarding lipid, glucose, arterial hypertension alterations and cardiovascular risk (CVR). The objective of metabolic monitoring is A1C ≤7%, similar to that of non-infected population, individualising by age, life expectancy, comorbidities, hypoglycaemia risk and costs. Cardiovascular risk should be calculated in all HIV patients with a risk calculator available for clinical use, even though we recommend the use of REGICOR tables as we are treating the Spanish population. Proper measurement of blood pressure should be a routine practice in the care of patients with HIV infection.
The aim of this document is to provide tools for the diagnosis and appropriate treatment of the main metabolic alterations to serve as a reference to professionals who care for people with HIV infection.
Los pacientes con infección por el VIH presentan un riesgo cardiovascular (RCV) mayor que la población general. La identificación de los pacientes con elevado RCV, la puesta en marcha de medidas preventivas y el control de los factores de riesgo modificables, especialmente en pacientes en tratamiento antirretroviral, deben formar parte del manejo del VIH.
El presente documento actualiza las recomendaciones publicadas en el año 2014, sobre todo en lo referente a las alteraciones lipídicas, glucídicas, de hipertensión arterial y RCV. El objetivo de control metabólico es una A1c ≤ 7%, similar a la de la población no infectada, individualizando según edad, expectativa de vida, comorbilidades, riesgo de hipoglucemias y costes. En todos los pacientes con VIH debe calcularse el RCV con alguna calculadora de riesgo disponible para uso clínico, si bien recomendamos el uso de las tablas de Regicor, al tratarse de población española. La medición correcta de la tensión arterial debe ser una práctica rutinaria en la atención a los pacientes con infección por el VIH.
El objetivo de este documento es proporcionar herramientas para el diagnóstico y tratamiento adecuado de las principales alteraciones metabólicas para que sirvan de consulta a los profesionales que atienden a personas con el VIH.
The importance of hydrocarbon and lipid metabolic disorders, and their impact on the systems of patients with Human Immunodeficiency Virus (HIV) infection requires a customized study and continuous updating.
The objective of this document is to provide practical information, from a treatment perspective, about the main metabolic disorders produced by the HIV infection, in order to describe appropriate treatment strategies for each patient. At the same time, this document is intended to serve as a reference tool for all professionals treating patients with HIV infection and who present or may present any of the metabolic disorders contained in this document1.
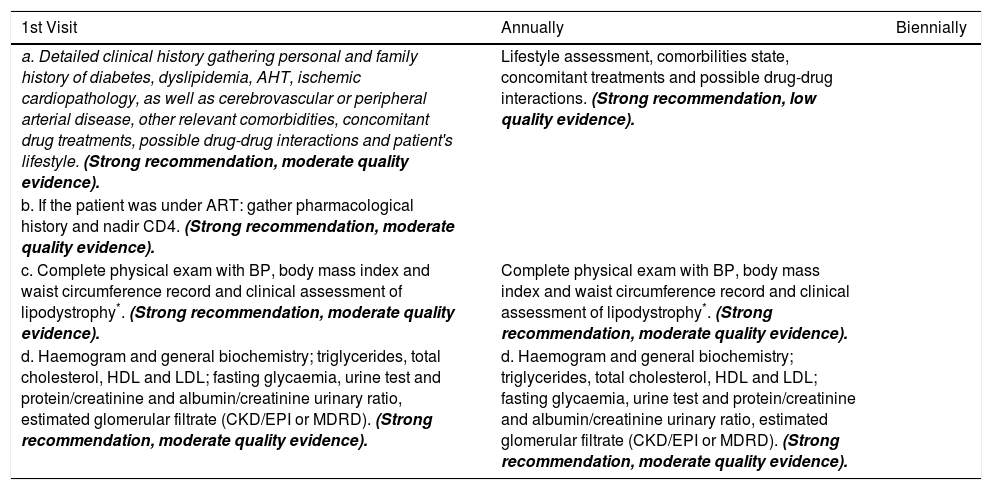
Clinical assessmentTable 1 contains recommendations for the clinical assessment of metabolic disorders in patients with HIV infection.
Recommendations for the clinical assessment of metabolic disorders in patients with HIV infection.
| 1st Visit | Annually | Biennially |
|---|---|---|
| a. Detailed clinical history gathering personal and family history of diabetes, dyslipidemia, AHT, ischemic cardiopathology, as well as cerebrovascular or peripheral arterial disease, other relevant comorbidities, concomitant drug treatments, possible drug-drug interactions and patient's lifestyle. (Strong recommendation, moderate quality evidence). | Lifestyle assessment, comorbilities state, concomitant treatments and possible drug-drug interactions. (Strong recommendation, low quality evidence). | |
| b. If the patient was under ART: gather pharmacological history and nadir CD4. (Strong recommendation, moderate quality evidence). | ||
| c. Complete physical exam with BP, body mass index and waist circumference record and clinical assessment of lipodystrophy*. (Strong recommendation, moderate quality evidence). | Complete physical exam with BP, body mass index and waist circumference record and clinical assessment of lipodystrophy*. (Strong recommendation, moderate quality evidence). | |
| d. Haemogram and general biochemistry; triglycerides, total cholesterol, HDL and LDL; fasting glycaemia, urine test and protein/creatinine and albumin/creatinine urinary ratio, estimated glomerular filtrate (CKD/EPI or MDRD). (Strong recommendation, moderate quality evidence). | d. Haemogram and general biochemistry; triglycerides, total cholesterol, HDL and LDL; fasting glycaemia, urine test and protein/creatinine and albumin/creatinine urinary ratio, estimated glomerular filtrate (CKD/EPI or MDRD). (Strong recommendation, moderate quality evidence). |
| e. ECG, specially at the start of ART with drugs that may have an impact on cardiac conduction, and when there are several drugs with the same effect. (Strong recommendation, low quality evidence). | ECG (Strong recommendation, moderate quality evidence) | |
| f. CVR estimation**(Strong recommendation, moderate quality evidence). | In patients with cardiovascular risk factors and, in general, in men ≥ 40 years old and women ≥ 50 years old. (Strong recommendation, moderate quality evidence). | |
| g. In selected cases of patients with an intermediate VR, it may be desirable to measure the ankle-brachial index or the carotid-intima media thickness to detect subclinical atherosclerosis. (Weak recommendation, low quality evidence). | ||
| h. In selected cases of patients with an intermediate VR, it may be desirable to measure CRP plasma concentrations and/or D-dimer to detect proinflammatory state and/or maintained procoagulant. (Weak recommendation, low quality evidence). |
With the objective of determining the body composition, it would be convenient to perform a DEXA where available. If it is not possible, body mass index and waist circumference will be measured and a clinical assessment of lipodystrophy will be performed.
See Cardiovascular Risk section to decide which scale to use.
AHT (Arterial Hypertension). ART (Antiretroviral treatment). ECG (electrocardiogram). HDL (High-density lipoprotein). LDL (low-density lipoprotein). Modification of Diet in Renal Disease (MDRD). Creatinine equation (CKD/EPI), BP (Blood pressure). CVR (Cardiovascular risk). VR (Vascular risk).
Patients with HIV infection have a higher risk of cardiovascular disease than the general population. Even though the mechanism that produces the vascular injury is unclear, various factors intervene, including genetic factors, traditional cardiovascular risk factors, Antiretroviral Treatment (ART) and parameters related to the HIV itself, like inflammatory and immune changes, even in patients with a good immunovirologic control.
The individual risk of suffering a cardiovascular disease can be estimated through conventional equations, even though they lack from precision in HIV population; specifically, Framingham equation overestimates cardiovascular risk in these patients, compared to others like SCORE. Strategies to lower cardiovascular risk include controlling HIV replication with ART and identifying and monitoring traditional cardiovascular risk factors. Other strategies like the use of statin drugs (anti-inflammatory or immunomodulator action) or antiaggregation with aspirin as primary prevention have yet to be clarified.
Recommendations- 1.
The individual risk of suffering cardiovascular disease should be estimated as accurately as possible. (Strong recommendation, low-quality evidence).
- 2.
Diet and lifestyle should be modified. Action should be taken on all modifiable factors, especially smoking, with a higher or lower intensity, depending on the estimated risk. (Strong recommendation, moderate-quality evidence).
- 3.
Patients with a history of cardiovascular disease should be referred to a cardiologist. Also, those with a high risk of cardiovascular disease should be considered to be referred to a cardiologist. (Strong recommendation, low-quality evidence).
Lifestyle is the key health determinant and the most modifiable one through primary prevention or health promotion activities. There is scientific evidence proving the importance of changing lifestyle habits in cardiovascular disease prevention and of health promotion in HIV patients. Nevertheless, in high-risk cases, interventions may be complex and their benefits subtle and complicated to prove in the short term.
According to the American Heart Association, smoking is in itself the greatest modifiable cardiovascular risk factor that contributes to premature morbidity. We should not forget that around 60-80% of HIV patients smoke. Cohort studies, like the ART-CC one, demonstrate that well-monitored HIV patients may lose more years of their life as a result of smoking than because of the HIV infection itself. Mortality rate among smokers was 1.94 times higher than among non-smokers.
There is a series of additional risks in women that are worthwhile pointing out because the probability of suffering a heart attack is multiplied by 10 in women who smoke and use oral contraceptives. Among women who smoke, menopause occurs an average of 2 to 3 years earlier than in women who have never smoked. The risk of suffering osteoporosis also rises.
This data emphasises the need to prioritize interventions to promote a decline in smoking. Non-smoking advice falls within Primary Health Care, while there are also tobacco withdrawal units in specialized attention to address the most complex cases or those with comorbidities.
Safety and effectiveness of electronic cigarettes as an aid to quit smoking have not been demonstrated. The World Health Organization (WHO) warns there is not enough scientific evidence to exclude health risks associated to their use and to the exposure to electronic cigarettes’ steam. There is even less evidence of them being an effective substitution therapy.
The Spanish Interdisciplinary Committee for Cardiovascular Prevention (CEIPC) recommends the increase of physical activity and its promotion among all age groups. Even high-risk patients should receive professional counselling to perform physical activity in a safe and controlled manner.
Recommendations- 1.
It is recommended to modify behaviours to obtain a healthy lifestyle. (Strong recommendation, moderate-quality evidence).
- 2.
It is recommended not to smoke or to quit smoking, with the objective of diminishing the effects on health. (Strong recommendation, high-quality evidence).
- 3.
As a general guideline, it is recommended to perform at least 30minutes of aerobic exercise a day. (Strong recommendation, moderate-quality evidence).
Incidence of lipodystrophy has decreased with the new antiretrovirals. Its prevalence is estimated between 10% and 80%. This variability is explained by the methodology used for its diagnosis and by the frequency of antiretroviral use associated to lipodystrophy in the different cohorts depending on the year of study. Even though there are pure lipoatrophy or lipoacumulus symptoms, in some patients both coexist.
RecommendationsDiagnosis- 1.
It is recommended to use DEXA as diagnostic method for body fat distribution. (Strong recommendation, low-quality evidence). If DEXA is not available, anthropometric measures, as well as other imaging tests like computed tomography and magnetic resonance, could be used instead. (Weak recommendation, high-quality evidence).
- 2.
It is recommended to follow a healthy lifestyle. (Strong recommendation, low-quality evidence).
- 3.
It is recommended to avoid thymidine-analogous in any ART guideline. (Strong recommendation, high-quality evidence).
- 4.
In patients with lipoatrophy, facial reconstructive surgery with autologous fat or synthetic substances is recommended. (Strong recommendation, moderate-quality evidence).
- 5.
Ultrasonic liposuction is only recommended to correct dorsum-cervical fat accumulation in cases where it translates into a decrease of quality of life for patients. (Strong recommendation, very low-quality evidence).
- 6.
Surgical resection is recommended in cases of localized fat deposits. (Strong recommendation, very low-quality evidence).
The prevalence of hydrocarbon metabolic disorders is high in patients with HIV infection (5-25%), with an incidence of 5-10% of new diabetes mellitus (DM) diagnostics. While for the general population DM is a coronary equivalent, this association is not so clear in HIV.
DM-HIV association also increases the risk of chronic kidney disease. A higher incidence of neuropathy and nerve damage in seropositive patients with DM has also been profiled.
HCV coinfection has a bidirectional relation with DM, thus, DM fosters hepatic fibrosis and hepatitis C virus infection (HCV) produces insulin-resistance, DM progression and worse metabolic control, conditioning also the use of potential hepatotoxic drugs.
In general, type 2 DM treatment is the same as for non-HIV population, with some considerations, since it is recommended to determine glucose levels on an empty stomach upon diagnosis of HIV infection, before starting the treatment, 3 to 6 months after a change, and every 6 to 12 months once the treatment has been stabilized. The possibility of screening every 3 months in patients younger than 45 without cardiovascular risk factors is questionable.
The objective of metabolic monitoring is A1C ≤7%, similar to that of non-infected population, individualising by age, life expectancy, comorbidities, hypoglycaemia risk and costs.
Recommendations- 1.
Hyperglycaemia is a cardiovascular risk factor that should be treated. (Strong recommendation, high-quality evidence).
- 2.
It is recommended to perform periodic screening, at the start of ART, 3 months into ART and every 6 to 12 months once the treatment is stabilized. (Strong recommendation, low-quality evidence).
- 3.
Fasting glycaemia and glycated hemoglobin (A1C) are useful for diagnosis and monitoring. (Strong recommendation, high-quality evidence). A1C objective is the same as for the general population (HbA1c<7%). (Strong recommendation, moderate-quality evidence).
- 4.
Screening of complications associated to diabetes in patients with HIV infection is similar to that of non-HIV population. (Strong recommendation, moderate-quality evidence).
- 5.
It is recommended to use the same therapeutic algorithm that in non-HIV population, taking into account interactions with ART. Metformin is the drug of choice except in patients with pronounced lypoatrophy, risk of lactic acidosis or advance kidney disease. (Strong recommendation, moderate-quality evidence).
- 6.
After metformin or if this is contraindicated, sulfonylureas (in non-obese patients) or pioglitazone (if lypoatrophy is pronounced) can be used. There is not enough experience with the rest of drugs (incretins and SGLT2 inhibitors). (Weak recommendation, low-quality evidence).
- 7.
When antidiabetic drugs fail, there are clear symptoms of hyperglycaemia, or in cases of type-1 diabetes, insulin is the drug of choice, with a similar management and adjustment as that of the general population. (Strong recommendation, high-quality evidence).
- 8.
The treatment of the rest of associated cardiovascular risk factors (dyslipidemia, arterial hypertension) is key to prevent cardiovascular events and should be taken into account. (Strong recommendation, high-quality evidence).
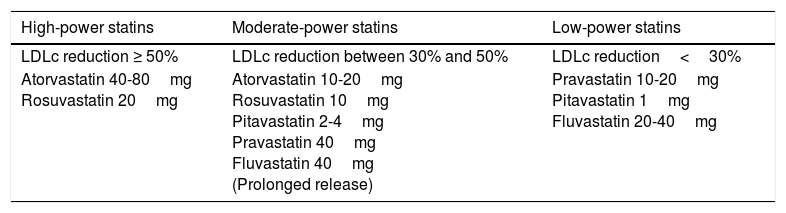
Dyslipidemia in patients with HIV infection is very frequent and is associated to an increase in cardiovascular risk. This is due, in part, to ART and to an increase of the inflammation and of the immune activation caused by HIV chronic infection. There is considerable amount of data that suggests the HIV infection is associated with an increase of cardiovascular disease. Therefore, the different cardiovascular risk factors should be evaluated as part of the medical visit, and especially, in patients under antiretroviral treatment. The evaluation of cardiovascular risk factors will be used to predict the individual risk of developing cardiovascular risk diseases. Currently, there are various methods to calculate risk, such as the Framingham Risk Score equation, REGICOR (calibration of Framingham's Tables applied to Spain), SCORE (Systematic Coronary Risk Evaluation) or DAD study. The current approach is to decide who should be treated with statin drugs, of high or moderate power (Table 2), depending on their cardiovascular risk, regardless basal lipids levels, and with the objective of reducing basal LDL levels by 50% or between 30% and 50%. This consensus document recommends starting the treatment with statin drugs if the estimated cardiovascular risk is higher than 7.5% at 10 years, even though there is no solid evidence supporting these recommendations in patients with HIV infection. In general, it is recommended to individualize cardiovascular risk management in HIV patients, on the basis that they have a higher risk than the general population.
Statin drugs classification according to their LDLc reduction power.
| High-power statins | Moderate-power statins | Low-power statins |
|---|---|---|
| LDLc reduction ≥ 50% | LDLc reduction between 30% and 50% | LDLc reduction<30% |
| Atorvastatin 40-80mg Rosuvastatin 20mg | Atorvastatin 10-20mg Rosuvastatin 10mg Pitavastatin 2-4mg Pravastatin 40mg Fluvastatin 40mg (Prolonged release) | Pravastatin 10-20mg Pitavastatin 1mg Fluvastatin 20-40mg |
| Statin treatment guidelines ACC/AHA Guidelines 2014 | ||
|---|---|---|
| Clinical situation | 10-year CVR assessment | Statins treatment |
| Established CVD LDLc ≥190mg/dl | Not necessary | High power High power |
| Type 1 and 2 DM 40-75 years of age | ≥7,5 ≤7,5 | High power Moderate power |
| Primary prevention and LDLc <190mg/dl 40-75 years of age | ≥7,5 | Moderate power |
- 1.
Always evaluate the presence of dyslipidemia in patients with HIV infection, as this is a frequent complication in patients under ART. (Strong recommendation, high-quality evidence).
- 2.
Always start dyslipidemia treatment with specific dietary and lifestyle recommendations depending on the lipid disorder detected. (Strong recommendation, moderate-quality evidence).
- 3.
Cardiovascular risk should be calculated in all HIV patients with a risk calculator available for clinical use, even though we recommend the use of REGICOR tables as we are treating the Spanish population. Treatment with statin drugs should be started in patients with confirmed cardiovascular disease, such as type-2 DM or cardiovascular risk>5% at 10 years. (Strong recommendation, moderate-quality evidence).
- 4.
Atorvastatin is recommended as a first choice, although pitavastatin, rosuvastatin or pravastatin may be considered as a safer drug treatment in primary and secondary prevention of hypercholesterolemia. (Strong recommendation, moderate-quality evidence).
- 5.
Fibrate are recommended as the most efficient drug treatment for severe hypertriglyceridemia (>500mg/dL) refractory to dietary treatment. (Strong recommendation, moderate-quality evidence).
- 6.
Systematic use of statin and fibrate combination treatment is not recommended, because it promotes toxicity of both drugs. (Strong recommendation, moderate-quality evidence).
- 7.
It is recommended to consider the association of ezetimibe and statins, since this may improve dyslipidemia in some patients. (Strong recommendation, moderate-quality evidence).
A large number of observational studies has analysed the relation between blood pressure (BP) and cardiovascular (CV) and kidney complications. BP measured both at the medical office and outside of it implies an independent relation between the incidence of severe CV complications, sudden death, cardiac insufficiency (CI) and peripheral arterial disease (PAD), as well as with end-stage kidney disease. This is true for all age and ethnic groups. This same data suggests that systolic blood pressure (SBP) is a more powerful indicator of complications than diastolic blood pressure (DBP) from 50 years of age on. Arterial hypertension prevalence in patients with HIV is between 15% and 25%, being more or less equivalent to that observed in the general population 10 to 15 years older.
Proper measurement of BP should be a routine practice in the care of patients with HIV infection. It is recommended to perform it during the initial visit and, later, once a year if levels are normal (SBP <130mmHg and DBP <85mmHg) and with a higher frequency if they are in the upper limit of normality (SBP 130-139mmHg and DBP 85-89mmHg) or if there are cardiovascular risk factors.
The main benefit of this treatment is the lowering of BP per se and said benefits are, to a large extent, independent from the drug used. Evidence shows that starting a treatment with thiazide diuretics, ACEi, AIIRA and calcium channel brokers properly reduces BP and CV risk. Betablokers are not recommended as a starting treatment because of data associating it with a higher risk of cardiovascular diseases or stroke.
There is evidence that, in high-risk patients, BP control is harder and requires a more frequent combination of antihypertensive drugs with other treatments like intensive hypolipidemic agent treatment. The only combination that cannot be recommended due to the results of the studies is that of two different renin-angyotensin system blockers.
Recommendations- 1.
Currently, recommendations for diagnosis and therapeutic management of arterial hypertension in patients with HIV infection should be the same as those of the general population. For that purpose, it is recommended to implement lifestyle changes and, if necessary, a treatment with antihypertensive drugs, aimed at reducing CV risk and cardiovascular disease morbimortality. (Strong recommendation, high-quality evidence).
- 2.
In population older than 60 years of age, treatment should be started to reduce SBP to less than 150mmHg and DBP to less than 90mmHg. (Strong recommendation, high-quality evidence).
- 3.
In population younger than 60 years of age, treatment should be started to reduce SBP to less than 140mmHg and DBP to less than 90mmHg. (Strong recommendation, high-quality evidence).
- 4.
When selecting antihypertensive drugs for patients under ART, it is recommended to take into account potential drug-drug interactions and adverse effects. ACEi and AIIRA antihypertensive drugs are tolerated best and have the lowest risk of interaction. (Strong recommendation, high-quality evidence).
Sexual dysfunction (SD) prevalence in patients with HIV infection is higher than that of HIV-negative population at any age. Among men, erectile dysfunction (ED), diminished libido and ejaculation and orgasm disorders are the most frequently described. Among women, decreased sexual desire and diminished sexual satisfaction are most common.
In the case of ED, the most frequent factors causing it are age and psychological and psychiatric disorders, basically depression and some of its treatments.
Hormonal disorders may be caused by the direct effect of HIV on endocrine organs (especially in advanced stages of the infection), due to systemic effect mediated by cytokines, by opportunistic infections and neoplasms associated to HIV, by drugs used in their treatment or by drug abuse.
Hormonal assessment should be personalized and driven by the clinic. Many times, symptoms are nonspecific or common to the HIV infection itself or the associated diseases and require a high level of suspicion for their diagnosis.
Recommendations- 1.
SD evaluation should be part of comprehensive care for patients with HIV infection, due to its high prevalence. (Strong recommendation, low-quality evidence).
- 2.
If phosphodiesterase-5 inhibitors are used, interactions with antiretroviral drugs should be taken into account, especially those strengthened by ritonavir and cobicistat. (Strong recommendation, moderate-quality evidence).
- 3.
Hormonal treatment recommendations in patients with HIV are limited and, therefore, general recommendations used in the general population not infected by this virus should be applied. (Strong recommendation, very low level of evidence).
HIV infection and certain ARV produce adverse effects similar to those observed in metabolic syndrome, including hepatic steatosis. Its prevalence in HIV-positive patients is between 30% and 50%.
Obesity and especially insulin resistance are key pathogenic factors. Hepatitis C virus infection and alcohol abuse are relatively prevalent in patients with HIV and may have an influence on pathogenesis. Biochemical methods to diagnose steatohepatitis are being investigated, however for the time being accurate diagnosis is based on histological confirmation.
Patients with steatosis and especially those with steatohepatitis have a higher risk of mortality in relation to comorbidity and advanced liver damage.
DM should have a special consideration, because it has been demonstrated that it is associated with a higher risk of developing hepatocellular carcinoma and the benefit related to a good metabolic control.
Eliminating genotype-3 HCV infection is associated with a significant improvement in steatosis, not so in other genotypes or without sustained viral response.
Recommendations- 1.
It is recommended to rule out hepatic steatosis in patients with diabetes or metabolic syndrome and with elevated transaminases levels without defined etiology. (Strong recommendation, low level of evidence).
- 2.
In the case of patients with risk factors for hepatic steatosis progression, measures for early diagnosis and treatment should be taken to prevent the progression of liver damage. (Strong recommendation, low level of evidence).
- 3.
It is recommended to perform at least one imaging method for diagnosis confirmation. (Strong recommendation, moderate level of evidence).
- 4.
The treatment is aimed at changing unhealthy lifestyle habits and treating diabetes and dyslipidemia properly, if they exist. (Strong recommendation, moderate level of evidence).
- 5.
In patients with steatosis or steatohepatitis, it is recommended for them to loose at least 10% of their weight. (Strong recommendation, moderate level of evidence).
The preparation of this document has been financed with the funds from the SPNS (Spanish National AIDS Plan Secretariat).
Conflicts of interestsIn order to avoid and/or minimize any conflicts of interests, the individuals who make up this Expert Group have made a formal declaration of interests. In this declaration, some of the authors have received funding to take part in conferences and to conduct research, as well as having received payments as speakers for public institutions and pharmaceutical companies. These activities do not affect the clarity of the present document as the fees and/or grants received do enter into the recommended conflict of interests.
It must be pointed out, as regards the drugs in this document, that it only mentions the active ingredient and not the commercial brand.
The Board of GEAM (Study Group on AIDS metabolic disorders) and GeSIDA (AIDS Study Group), and the SPNS (Spanish National AIDS Plan Secretariat) are grateful for the support and opinions of Emely García Carrasco, Gabriela Fagúndez, Saúl Barreales, Cristina Gómez-Chacon Galán and Mª Dolores Perea Aceituno, that have contributed to improve the writing and enrich the contents of the document.
Writing Committee
Rosa Polo Rodríguez. Secretaría Plan Nacional sobre el Sida. Madrid. María José Galindo Puerto. Unidad de Enfermedades Infecciosas. Hospital Clínico Universitario. Valencia. Julian Olalla. Unidad de Enfermedades Infecciosas. Hospital Costa del Sol. Marbella. Málaga. Félix Gutiérrez. Unidad de Enfermedades Infecciosas. Hospital General Universitario. Elche. Carmen Gómez Candela. Servicio de Endocrinología y Nutrición. Hospital Universitario La Paz. Madrid. Vicente Abril. Unidad de Enfermedades Infecciosas. Hospital general Universitario. Valencia.Sergio Serrano. Unidad de Enfermedades Infecciosas. Hospital Ramon y Cajal. Madrid. Jose Ramón Blanco. Unidad de Enfermedades Infecciosas. Hospital San Pedro CIBIR. Logroño. Noemí GP Villar. Servicio de Endocrinología y Nutrición. Hospital Universitario La Paz. Madrid. Celia Miralles. Consulta de VIH. Complejo hospitalario Xeral de Vigo. Angel Merchante. Servicio de Endocrinología y Nutrición. Hospital General Universitario. Castellón. Vicente Estrada. Unidad de Enfermedades Infecciosas Hospital Clínico Universitario San Carlos. Madrid. Carlos Dueñas. Unidad de Enfermedades Infecciosas. Hospital Universitario. Valladolid. Jesús Sanz Sanz. Unidad de Enfermedades Infecciosas. Hospital Universitario de La Princesa. Madrid. Rosario Palacios. Unidad de Enfermedades Infecciosas Hospital Virgen de la Victoria. Málaga. Fernando Lozano. Unidad de Enfermedades Infecciosas. Hospital Universitario de Valme, Sevilla. Ana Mariño. Unidad de Enfermedades Infecciosas Hospital Arquitecto Marcide. Ferrol. Victor Asensi. Unidad de Enfermedades Infecciosas. Hospital Universitario Central de Asturias. Oviedo. Miguel Ángel Von Wichmman. Unidad de Enfermedades Infecciosas Hospital Donostia. San Sebastian. Enrique Ortega. Unidad de Enfermedades Infecciosas. Hospital Universitario Valencia. Esteban Martínez Chamorro. Especialista en Medicina Interna. Unidad de Enfermedades Infecciosas. Hospital Universitario Clinic.Barcelona.
See writing Committee in Appendix A. All members of the panel are authors of this publication
The entire version of the document can be found online as supplementary material in the journal official website (Appendix B).