This is the first study reporting the epidemiological and molecular characterization of HCV/HIV coinfection in the central region of Argentina.
MethodCross-sectional, epidemiological study (2003-2004). Statistics: multivariate logistic regression analysis.
ResultsThe incidence of HCV/HIV coinfection was 12.3%. HCV genotype 1 was the most prevalent (73%). Intravenous drug use was the main independent risk factor for acquiring HCV infection. However, an alternative route (sexual) for viral transmission was suggested.
ConclusionsThese results underscore the potential public health impact of HCV/HIV coinfection in our region.
Primer reporte epidemiológico y molecular de la coinfección por el virus de la hepatitis C y el virus de la inmunodeficiencia humana (VHC/VIH) en la región central de Argentina.
MétodoEstudio epidemiológico transversal (2003-2004). Análisis: regresión logística multivariado.
ResultadosLa coinfección VHC/VIH fue 12,3%. El genotipo 1 fue el más prevalente (73%). El uso de drogas intravenosas fue el principal factor de riesgo asociado con HCV. Sin embargo, se sugiere una vía alternativa (sexual) de transmisión.
ConclusiónEstos resultados destacan el potencial impacto sanitario de la coinfección VHC/VIH en nuestra región.
It has been well established that exposure to infected blood is the main risk factor for HCV infection1. Epidemiological data from Buenos Aires, Argentina, describe prevalence rates between 32% and 58% among HIV-infected intravenous drug users (IVDU), while the prevalence of HCV infection in blood donors varies between 0.5 and 1%2,3
Despite these published data, there is no information about the epidemiology of HCV infection in other HIV groups of Argentina, and data about HCV genotype distribution in these groups is not available.
Currently, argentine patients infected with HCV have no access to Public Health Programs for confirmatory diagnosis of infection, genotyping and viral load measurement for beginning and follow up of anti-HCV therapy. In addition, in central Argentina epidemiological and molecular characteristics of HCV infection in HIV-coinfected individuals are still unknown.
Herein, we present the data from a study to gain insight into the epidemiology, molecular characteristics and risk factors for HCV infection in the HIV-infected population of central region of Argentina. These results are important to gain a better understanding of the public health issues in our region.
MethodsA cross-sectional study was conducted in 310 ambulatory HIV-infected patients [266 males; mean age 35.0 years old (r = 15-68), and 44 females; 35.4 years old (r = 13-61)] who had access to antiretroviral therapy at two public health centers of Cordoba (second most populated inland province of Argentina), between February 2003 and August 2004.
Blood was collected using vacutainer tubes. The material was then prepared for examination and/or stored in a -70 °C freezer according to standard procedures.
Demographic and risk behavior data were obtained from medical records.
The presence of anti-HCV antibodies was tested in duplícate by Hepatitis C (anti-HCV) EIA Wiener Lab., 2000 Rosario, Argentina.
Viral RNA was extracted from 100 μl of anti-HCV positive samples (plasma) with Trizol reagent (Invitrogen, Rockville, MD). The RT-Nested PCR for 5′-non-coding region was used to amplify a 280 nt fragment, as previously described4.
HCV genotyping was determined by the restriction length polymorphism analysis (RFLP) of the 5′-non-coding region (5′NCR)4.
We calculated mean values and crude rates with 95% exact binomial confidence intervals (CIs), after Pearson or Fisher tests for bivariate analysis approach. Statistical significance was established at p < 0.05. Odds ratios (ORs) and 95% CI were used to quantify the associations between risk factors and viral infection. Múltiple logistic regression models was used to identify factors associated with HCV infection and estimated risk coefficients. Variables associated with HCV infection in univariate analysis (p <0.05) were entered into the model by means of backward selection method. We tested potential confounders before selecting the final model, that is, we entered significant variables into selected multiple model and estimated their effects on the odd ratios (OD) of the independent variables. The statistical package STATISTIC version 6.0 (2300 EAST 14 th street, Tulsa, OK, USA, 2005) for windows from Satatsoft was used for the model fitting process.
ResultsThe estimated prevalence of anti-HCV antibodies was 12.6% (39/310). The HCV infection in the seropositive samples was confirmed by RT-Nested PCR in 97.4% (38/39) of the cases. Thirty subjects (78.9%) with positive anti-HCV/RNA HCV were males (mean age 36.5 years old, r = 22-50) and 8 (21.1%) females (mean age 30.4 years old, r = 13-42).
Overall 38 HCV-infected subjects, 14 (36.8%) were homosexual males and 35 (92.1%) drug users: 28 (73.6%) intravenous drug users (IVDU) and 7 (18.4%) inhaled cocaine users. Thirty of them (78.9%) reported promiscuity, 27 (71.0%) were sexual partners of HIV-infected subjects, 14 (36.8%) were sexual partners of IVDU and 16 (42.1%) had at least 1 tattoo.
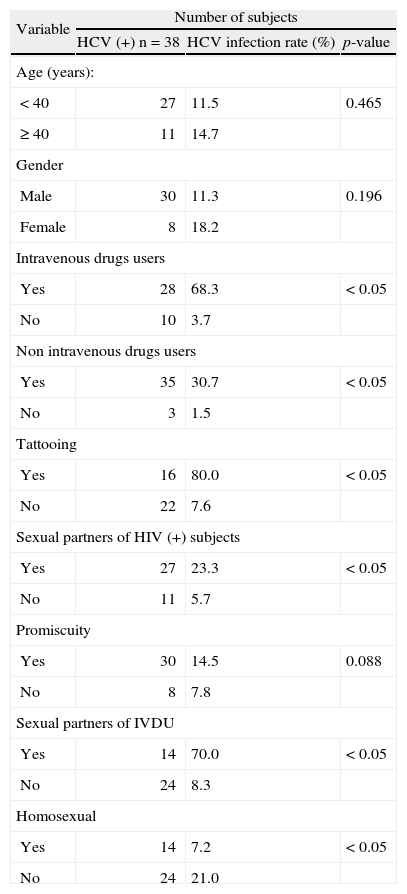
The variables associated (p < 0.05) with HCV infection in a bivariate analysis (covariate and response variable) are shown in Table 1. We did not observe a significant association between infection and age, sex or sexual promiscuity.
Bivariate analysis: variables associated with hepatitis C (HCV) infection, among HlV-infected individuals of Córdoba, Argentina
| Variable | Number of subjects | ||
| HCV (+) n = 38 | HCV infection rate (%) | p-value | |
| Age (years): | |||
| < 40 | 27 | 11.5 | 0.465 |
| ≥ 40 | 11 | 14.7 | |
| Gender | |||
| Male | 30 | 11.3 | 0.196 |
| Female | 8 | 18.2 | |
| Intravenous drugs users | |||
| Yes | 28 | 68.3 | < 0.05 |
| No | 10 | 3.7 | |
| Non intravenous drugs users | |||
| Yes | 35 | 30.7 | < 0.05 |
| No | 3 | 1.5 | |
| Tattooing | |||
| Yes | 16 | 80.0 | < 0.05 |
| No | 22 | 7.6 | |
| Sexual partners of HIV (+) subjects | |||
| Yes | 27 | 23.3 | < 0.05 |
| No | 11 | 5.7 | |
| Promiscuity | |||
| Yes | 30 | 14.5 | 0.088 |
| No | 8 | 7.8 | |
| Sexual partners of IVDU | |||
| Yes | 14 | 70.0 | < 0.05 |
| No | 24 | 8.3 | |
| Homosexual | |||
| Yes | 14 | 7.2 | < 0.05 |
| No | 24 | 21.0 | |
*Pearson's χ2 or Fisher's exact test (as suitable, based on expected cell size).
HIV: human immunodeficiency virus; IVDU: intravenous drugs users.
Due to the dependence structure between covariates, we fitted multiple logistic regression models in order to obtain the adjusted risk estimates. This analysis showed that gender (adjusted OR = 1.326; CI 95%: 1.086, 2.609), age (OR = 2.562, CI 95%: 2.445, 2.691), IVDU (OR = 25.0, CI 95%: 6.2, 100.1) and tattooing (OR = 25.6, CI 95%: 4.2, 154.6]) were risk factors for HCV infection (Table 2).
Multiple logistic regression analysis: variables associated with HCV infection among 310 HIV-infected individuals from Córdoba, Argentina
| Variable* | Number of HCV (+) subjects/ total number of subjects | Adjusted OR | CI 95% | p-value |
| Age (years) | ||||
| ≤ 40 | 11/75 | |||
| > 40 | 27/235 | 2.562 | 2.445-2.691 | < 0.01 |
| Gender | ||||
| Male | 30/266 | |||
| Female | 8/44 | 1.326 | 1.086-2.609 | < 0.05 |
| Intravenous drugs users | ||||
| Yes | 28/41 | |||
| No | 10/269 | 25.019 | 6.254-100.09 | < 0.0001 |
| Tattooing | ||||
| Yes | 16/20 | |||
| No | 22/290 | 25.627 | 4.249-154.56 | < 0.0001 |
Non-inhaled drug users: inhaled cocaine and/or marihuana users.
CI: confidence interval; HCV: hepatitis C virus; HIV: human immunodeficiency virus; OR: odds ratio.
HCV genotypes were tested in 37 of the 38 RNA-positive specimens. Genotype 1 was identified in 27/37 (73.0%), genotype 3 in 5/37 (13.5%) and genotype 2 in 1/37 (2.7%). One subject (2.7%) was coinfected with two genotypes of HCV (1/2), and three samples (8.1%) gave indeterminate patterns.
DiscussionThe confirmed prevalence of HCV infection using molecular methods was 12.3% in HIV infected subjects. This rate was lower than the 30 to 50% reported in other cohorts from Buenos Aires (capital of Argentina)3,5. These differences could be due to the fact that in Buenos Aires cohorts, infection rates were calculated based on detection of antibodies by serological test3,5. Furthermore in that study subjects enrolled were mostly IVDUs.
The HCV genotypes distribution is associated with certain stratification and population clusters. Several studies worldwide have reported that among HIV-infected IVDU individuals, genotype 1 is the most prevalent; however, genotype 3 is frequently found. In Cordoba, we demonstrated that the prevalence of genotype 1 was clearly higher (73.0%) compared to genotype 3 (13.5%). However, in this province, the prevalence of HCV genotypes is different (50% of genotype 2) among HIV (-) individuals4.
The HCV genotype impacts on the progression of HIV infection and has important implications in medical care and treatment of coinfected patients1,6. Thus, the data obtained from this study should be taken into consideration at the moment of planning an HCV antiviral therapy suitable for this country.
Our results show that among HIV-infected individuals, the use of intravenous drugs increases the risk of HCV infection at least 6 folds (Table 2). In other countries, the high prevalence (72-95%) of HCV has been closely related to the use of illegal injectable drugs1. In concordance, these results show that 13.2% of the HIV-infected subjects enrolled were IVDU, and of these, a high percentage (68.3%) was HCV (+). Moreover, other risk factors associated with HCV infection were: age over 40 years, female gender, and tattooing history (Table 2).
The association between age and HCV infection may reflect the accumulative effect of risk behaviors (for instance: duration and frequency of injection) or an interaction between risk behaviors1,7. We also found a high association between tattooing and HCV infection; however, this factor was always present among drug users. For this reason, we consider tattooing a variable that may increase the risk of HCV infection in this population; however, it is not a single associated risk factor.
Even though the association of the HCV infection and use of inhaled cocaine did not show values statistically significant by a multivariate analysis, we did find an important percentage (18%, 7/38) of individuals infected with HCV that were cocaine users. In this sense, some studies have proposed the use of inhaled cocaine as a risk factor for the acquisition of HCV infection8.
Even though we did not find significant evidences of sexual risk factors for HCV infection (Table 2), 4 individuals were not drug users and reported only risk factors related with sexual behaviors. Two individuals were homosexual males and 2 reported promiscuity. Despite the differences found, there are enough data to support that the sexual transmission of HCV can occur, but this virus would not be efficiently disseminated by this route9. Several publications have reported HCV RNA detection in semen and in lymphocytes of cervical smears of seropositive individuals9,10. Among HIV-infected individuals, the sexual transmission of HCV seems to be more efficient and significantly contributes to the incidence of the infection by this virus. It has been proposed that this could be due to the fact that the presence of the HIV and the concomitant immunosuppression would increase HCV replication9. However, the precise mechanism by which HIV increases risk of sexual transmission of HCV in still unknown.
In this study, the HCV RNA was detecting in 97.4% of seropositive individuals. It has been suggested that in individuals with higher viral loads, the risk of sexual transmission would increase. These findings, along with the epidemiological characteristics of these patients support the epidemiological evidence obtained from this study, which suggests that 10.5% individuals without risk of parenteral infection would get the infection by the sexual route.
Further studies should be carried out to go deep into sexual factors to confirm this hypothesis. Issues of critical importance are whether the level of HCV RNA predicts the risk of transmission, if STDs increase the risk of HCV acquisition, whether specific sexual practices (e.g. anal versus vaginal sex) affect the risk of HCV infection and whether the saliva could be involved in HCV transmission.