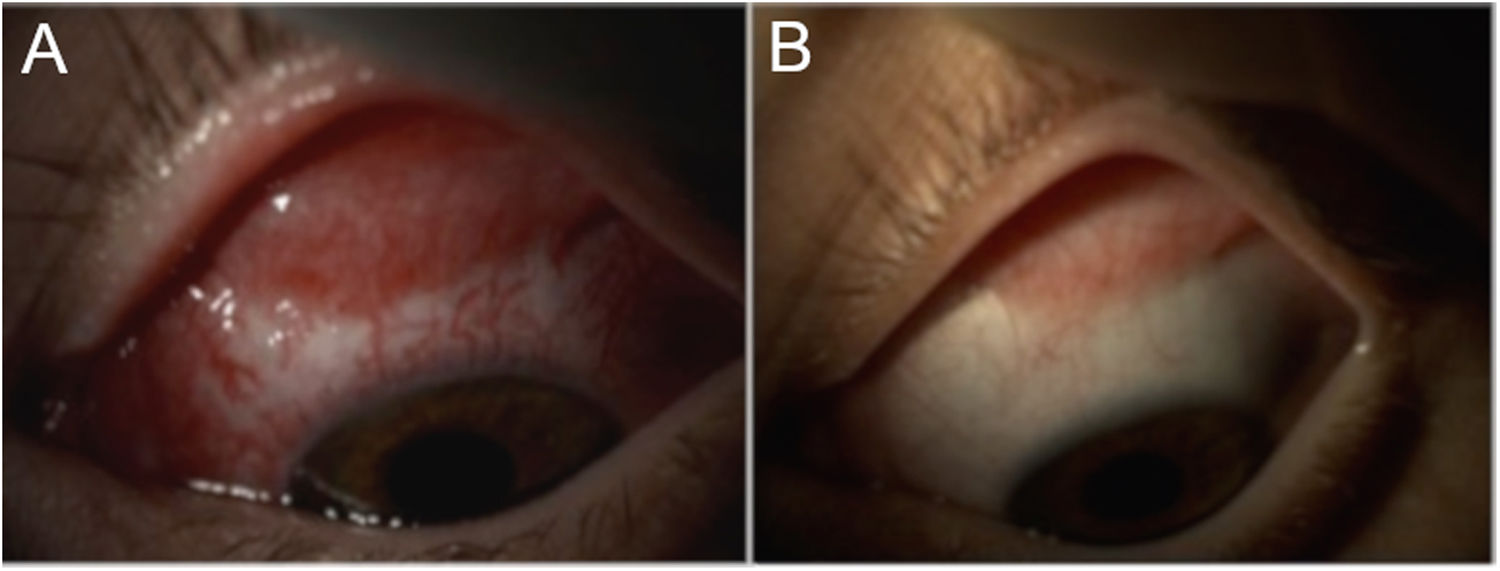
A 20-year-old female was being treated for bacterial vaginosis with doxycycline and metronidazole. She sought emergency ophthalmology treatment for pain, secretion and inflammation in her left eye. Examination revealed periocular oedema, conjunctival hyperaemia and abundant purulent secretion (Fig. 1). Extraocular motility appeared to be affected, so an orbital CT scan was ordered and confirmed solely preseptal involvement. The patient reported that she did not have a regular sexual partner and that she occasionally had unprotected sexual relations with different partners, but did not maintain contact with them and therefore could not locate them.
Secretion samples were taken for staining and culture, and empirical treatment was started with 1 g of intravenous ceftriaxone, ofloxacin eye drops 3 mg/mL 6 times daily and frequent eye flushes. Gram staining showed Gram-negative cocci arranged in pairs.
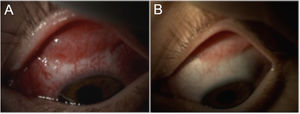
Clinical courseOther sexually transmitted diseases (STDs) were ruled out. The patient followed a favourable clinical course with rapid improvement of her signs and symptoms. Given her severe conjunctival inflammation, serious adhesions developed, particularly in the fundus of the superior sac (Fig. 2A), whereupon it was decided to start treatment with oral corticosteroids. Following 2 weeks of treatment, the patient's signs and symptoms remitted entirely. As sequelae the patient had persistent eye surface dysfunction (due to damage to the conjunctival lacrimal glands and in calciform cells), symblepharon (conjunctival adhesions) (Fig. 2B) in the fundus of the superior conjunctival sac and ptosis of the superior eyelid. The culture tested positive for Neisseria gonorrhoeae resistant to ciprofloxacin and tetracycline and sensitive to penicillin and cefotaxime.
Diagnosis: gonococcal conjunctivitis.
Closing remarksNeisseria gonorrhoeae is a Gram-negative diplococcus that often causes STDs. Gonococcal conjunctivitis (GC) is caused by this pathogen. GC primarily affects neonates and sexually active individuals.1–3 The neonatal form is transmitted from infected mothers through contact with birth canal secretions.1 In adults, GC is considered an uncommon STD; it is transmitted through ocular contact with secretions from infected patients.1,2,4
In recent years, some countries have reported an increase in the incidence of Neisseria gonorrhoeae infection,1–5 although this has not been reflected in a proportionate increase in numbers of cases of ocular involvement,1,2,5 possibly due to hand-washing.5 McAnena et al. reported an incidence of GC in adults of 0.19 per 1000 inhabitants from 2011 to 2013.2 Rothschild et al. found that of 4325 cases of bacterial conjunctivitis, just 0.55% (n = 24) were caused by Neisseria gonorrhoeae, and 5.11 % (n = 221) were caused by Chlamydia trachomatis (CT).5 Concomitant CT infection was present in 50% of patients with Neisseria gonorrhoeae infection.3,4 Different studies have shown that GC predominantly occurs in young men1,2,5 and appears to be particularly linked to homosexual practices.2,4
GC is usually unilateral and presents with hyperaemia and oedema of the conjunctivae and eyelids, abundant purulent secretion and preauricular lymphadenopathy; its clinical picture is more florid than that of other types of bacterial conjunctivitis, and it may cause serious ocular complications.1,2,4,6 Occasionally, severe oedema and periocular swelling require differential diagnosis with orbital cellulitis using neuroimaging techniques.1
In these patients it is imperative to rule out other STDs; in some cases, urethral symptoms predate ocular symptoms by one to several weeks,2,4,6 though GC may also present with no evidence of genital infection.
PCR is considered the gold standard for the diagnosis of Neisseria gonorrhoeae infection. Culture (in chocolate agar and Thayer-Martin agar) is less sensitive due to the organism's lability, but enables preparation of an antibiogram.2
Most clinical guidelines recommend the use of 1−2 g of intramuscular or intravenous ceftriaxone as a treatment of choice, along with oral azithromycin, given the frequency of concomitant CT infection. As regards the eyes, it is recommended that they be flushed with plenty of normal saline to remove secretions and decrease the bacterial load, since the presence of abundant germs on the eye surface, combined with their capacity to invade the healthy corneal epithelium, could promote ulceration and subsequent eye perforation.1–4,6,7
In patients with signs and symptoms of purulent hyperacute conjunctivitis with abundant inflammation, a gonococcal aetiology should be suspected. These patients should be managed jointly with ophthalmologists, microbiologists and infectious disease specialists to prevent ocular complications and rule out other STDs. Conjunctival symblepharon is a possible complication associated with GC that has not been previously reported and may cause eye surface problems in these patients.
Conflicts of interestNone.
Please cite this article as: Lacorzana J, Ortiz-Perez S, Galvez Prieto-Moreno C, Gutierrez-Fernandez J. Conjuntivitis hiperaguda en paciente joven. Enferm Infecc Microbiol Clin. 2021;39:98–99.