The aim of this study was to assess the prevalence of occult HBV infection in HIV-positive patients in a centre in Southern Spain.
MethodsThe HBV serological markers were investigated in all the patients and the presence of HBV-DNA was tested by PCR in patients with isolated anti-HBc.
ResultsAn isolated anti-HBc pattern was detected in 144/520 (27.7%) patients. HBV-DNA was detected in one of these patients (0.7%).
ConclusionsIn Southern Spain, there is a low prevalence of occult HBV infection among HIV-infected patients, despite increasing immigration from endemic countries.
El objetivo de este estudio fue evaluar la prevalencia de infección oculta por VHB en pacientes infectados por VIH del sur de España.
MétodosSe investigaron los marcadores serológicos para VHB y se analizó la presencia de ADN-VHB en los anti-HBc “solo”.
ResultadosEl patrón anti-HBc “solo” fue detectado en 144/520 (27,7%) pacientes. El ADN-VHB fue detectado en un paciente (0,7%).
ConclusionesLa prevalencia de infección oculta por VHB es baja entre los pacientes infectados por VIH a pesar del aumento en la inmigración desde países endémicos.
Hepatitis B virus (HBV) infection is a major health problem, affecting more than 350 million of people around the world. Occult HBV is defined as the presence of HBV-DNA without detectable surface antigen (HBsAg). This condition is particularly common among patients with isolated anti-HBc pattern.1 Co-infection with HBV is also common in HIV-infected patients, due to shared spreading ways, being a significant cause of death in this setting.2 Lamivudine and emtricitabine are extensively used in HIV infection and these drugs may lead to the emergence of mutations in HBV of immune escape, which are a cause of HBsAg non-detection.3
A high prevalence of occult HBV infection in HIV-coinfected patients, with an increased frequency (10–22%) of immune escape mutants has recently been reported in several countries of Africa.4,5 On the contrary, in most European countries the prevalence of HBV occult infection has been reported to remain at a low level.1,6 However, Spain has been a through route or the final destination for an increasing number of African immigrants. Consequently, there is a potential risk for a growth in the prevalence of occult HBV infection in Spain. The aim of this study was to evaluate the current prevalence of occult HBV infection among HIV-infected patients in Spain.
2Methods2.1PatientsAll HIV infected patients, older than 18 years, attending the Infectious Diseases Unit of a tertiary care centre in Seville, Southern Spain, from September 2008 to February 2009, were enrolled in this prospective cross-sectional study. All patients underwent a clinical evaluation and filled in an epidemiological questionnaire on the day of blood testing.
2.2Laboratory testsHIV infection was diagnosed by ELISA and confirmed by western-blot. HCV infection was diagnosed by COBAS® Amplicor HCV Test, V2 (Roche Diagnostics, Germany). Patients were tested for HBsAg, anti-HBc and anti-HBs using EIA (ADVIA Centaur XP, Siemens Healthcare Diagnostics S.L. USA). Positive Anti-HBc, with negative HBsAg and anti-HBs samples were tested for HBV-DNA with COBAS® AmpliPrep/COBAS® Taqman HBV Test (Roche Molecular Systems Inc., France; detection limit, approximately 100copies/ml). HBV genotype was determined by Trugene HBV Genotyping (Siemens Healthcare Diagnostics Inc., USA).
2.3EthicsThis study was designed and conducted according to the principles of the declaration of Helsinki. It was approved by the Ethics Committee of the Hospital.
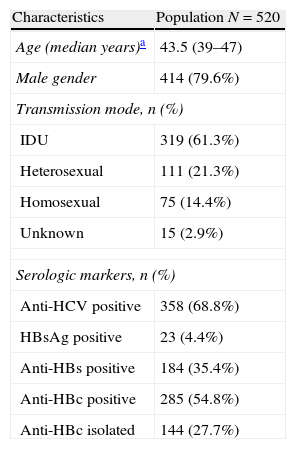
3ResultsA total of 520 HIV-positive patients were included in the study. Epidemiological characteristics and serological markers of the population are shown in Table 1. One hundred and forty four patients (27.7%) were HBsAg negative, anti-HBs negative and anti-HBc positive. Among these patients, 126 (87.5%) were male with a median (interquartile range) age of 45 (42–48) years. As regards the transmission route, 128 (88.8%) were intravenous drugs users and 12 (8.4%) reported sexual risk factors for HIV infection. All these patients with anti-HBc alone were Caucasian and born in Spain, except for one who was born in Portugal. One hundred and thirty nine (95.3%) patients were treated with antiretroviral therapy including a drug with anti-HBV activity. Among these patients, lamivudine or emtricitabine was prescribed to 101 (70.1%) patients and tenofovir to 64 (44.4%) patients. HBV DNA was detected only in one (0.7%) case. This HBV DNA-positive patient was a 45-year-old Spanish man, co-infected with HCV, without HAART. The HBV DNA load was 1350IU/mL and the HBV genotype was D without mutations on ‘a’ determinant.
Characteristics of the study population.
| Characteristics | Population N=520 |
| Age (median years)a | 43.5 (39–47) |
| Male gender | 414 (79.6%) |
| Transmission mode, n (%) | |
| IDU | 319 (61.3%) |
| Heterosexual | 111 (21.3%) |
| Homosexual | 75 (14.4%) |
| Unknown | 15 (2.9%) |
| Serologic markers, n (%) | |
| Anti-HCV positive | 358 (68.8%) |
| HBsAg positive | 23 (4.4%) |
| Anti-HBs positive | 184 (35.4%) |
| Anti-HBc positive | 285 (54.8%) |
| Anti-HBc isolated | 144 (27.7%) |
IDU, intravenous drug user.
A low prevalence of HBV DNA was found among HIV-infected patients with isolated anti-HBc in Southern Spain in this study. Indeed, only one case of occult HBV infection was observed. It was a native patient, harbouring HBV genotype D, the most common genotype in the Mediterranean countries, without mutations on ‘a’ determinant. This means that HBV infection is still scarcely introduced in this area, despite increasing immigration from endemic countries.
The HBsAg prevalence was 4.4%. This value represents a similar prevalence with respect to other study of HBV infection among HIV-positive patients in Spain.7 The prevalence of isolated Anti-HBc in the study population was relatively high, and this high prevalence of isolated Anti-HBc led us to expect an increased frequency of HBV-DNA detection. Perhaps, the fact that the majority of patients included in this study were treated with antiretroviral therapy, including some drugs, such as tenofovir that also have an effect on HBV replication, has contributed to this finding, and could explain the difference compared to African countries. This fact might have led to an underestimation of the actual frequency of occult HBV infection. This hypothesis is reinforced by the fact that the only patients with occult HBV were not under antiretroviral treatment.
The circulation of HBV has decreased, but remains considerable in some countries, such as Italy and Australia, because of the significant high prevalence of HBV markers in the migratory population.1,8 In this way, occult HBV infection could be spread through Southern Europe, since this area is a major receptor of immigrants from Sub-Saharan Africa. Because of this, HBV occult needs periodic surveillance studies in this area, such as that presented here, since the existence of growing migratory movements may lead to an increase in the prevalence of occult HBV. However, we cannot ignore that the main source of liver disease in patients infected with HIV is the HCV coinfection and therefore, its treatment should be monitored.9
This study has two limitations. Firstly, no patients with status other than isolated anti-HBc were tested, and some cases of occult HBV infection may have gone unnoticed. However, given the minimum prevalence found among subjects with anti-HBc alone, it is very unlikely that a significant number of cases of occult HBV infection among patients with other serological status were found. Secondly, although the technique used by us to determine the presence of HBV DNA is the standard for the detection of HBV DNA, perhaps by using more sensitive procedures, such as nested PCR, some additional cases of occult HBV infection may have been detected.10
In conclusion, the prevalence of occult infection among HIV-infected patients is still low in Southern Spain, perhaps due to extensive use of antiretroviral therapy active against HBV. However, given that this area is at risk for a higher number of cases, surveillance programs for this disease should be implemented, since using serum HBsAg test is of little use for detecting this disease.
Conflict of interestsThe authors declare no conflicts of interest related to this study.
The authors wish to thank Carmen Roldán for her technical support. This study has been supported in part by a grant from the Spanish Health Ministry (ISCIII-RETIC RD06/006 and projects PI10/01664). JAP is the recipient of an extension grant from the Fundación Progreso y Salud of the Consejería de Salud de la Junta de Andalucía (Reference AI-0021).