Evaluation of acute scrotum in neonates is a surgical emergency since the most common diagnosis is testicular torsion. Other causes, such as epididymo-orchitis (EO), are very uncommon during neonatal age.1 We present a neonatal EO and review all similar cases reported in the literature.
A 19-day-old male was brought to the Emergency Department with an erythematous and firm swelling of his left scrotum associated with irritability and fever that had begun five hours before. He had been born healthy at 38 weeks of gestational age and prenatal ultrasounds were normal. Clinical examination revealed a firm and erythematous left hemiscrotum. Doppler ultrasound findings were compatible with bilateral EO, mainly in the left hemiscrotum with a right hydrocele and a left pyocele. Laboratory examinations showed a white blood cell count of 13,700mm–3 (neutrophils 55%), C-reactive protein 132mg/L and procalcitonin 4.5ng/mL. Urine and cerebrospinal fluid (CSF) analysis were normal. He was admitted and empirical treatment with intravenous ampicillin and cefotaxime was started. After Escherichia coli was isolated in urine and blood cultures, ampicillin was discontinued. CSF culture was sterile. Renal ultrasound was normal. Fever resolved within 24h. A new scrotal ultrasound after nine days of treatment showed improvement in inflammatory changes and pyocele resolution. He was discharged after ten days of intravenous cefotaxime with an almost full recovery of scrotal inflammatory signs.
In neonates presenting with acute scrotum it is mandatory to distinguish between testicular torsion and other conditions using Doppler ultrasound. Compared with testicular torsion, the majority of cases of EO present with fever, increased acute phase reactants and increased blood flow.2
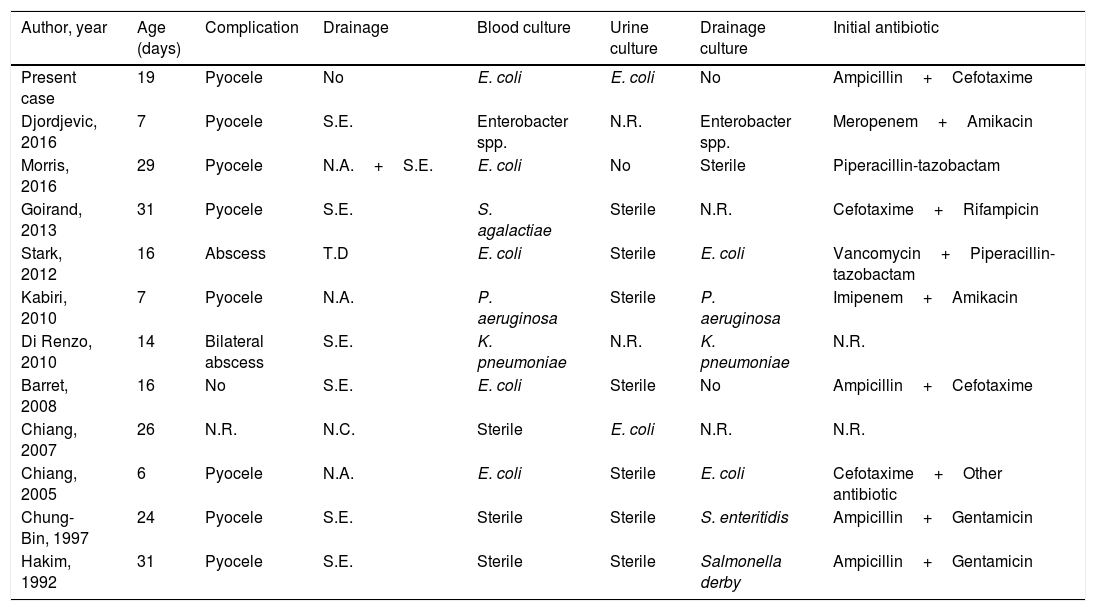
Only 11 cases of EO with a microbiological isolation in patients below 1 month of age have been reported in the literature in the last 30 years (1987–2016; Table 1).2–4 Hematogenous spread appears to be the causative mechanism in eight cases. Direct extension from a urinary tract infection has been described in one patient.
Characteristics of neonatal epididymitis/epididymo-orchitis with microbiological isolation published in the last 30 years.
| Author, year | Age (days) | Complication | Drainage | Blood culture | Urine culture | Drainage culture | Initial antibiotic |
|---|---|---|---|---|---|---|---|
| Present case | 19 | Pyocele | No | E. coli | E. coli | No | Ampicillin+Cefotaxime |
| Djordjevic, 2016 | 7 | Pyocele | S.E. | Enterobacter spp. | N.R. | Enterobacter spp. | Meropenem+Amikacin |
| Morris, 2016 | 29 | Pyocele | N.A.+S.E. | E. coli | No | Sterile | Piperacillin-tazobactam |
| Goirand, 2013 | 31 | Pyocele | S.E. | S. agalactiae | Sterile | N.R. | Cefotaxime+Rifampicin |
| Stark, 2012 | 16 | Abscess | T.D | E. coli | Sterile | E. coli | Vancomycin+Piperacillin-tazobactam |
| Kabiri, 2010 | 7 | Pyocele | N.A. | P. aeruginosa | Sterile | P. aeruginosa | Imipenem+Amikacin |
| Di Renzo, 2010 | 14 | Bilateral abscess | S.E. | K. pneumoniae | N.R. | K. pneumoniae | N.R. |
| Barret, 2008 | 16 | No | S.E. | E. coli | Sterile | No | Ampicillin+Cefotaxime |
| Chiang, 2007 | 26 | N.R. | N.C. | Sterile | E. coli | N.R. | N.R. |
| Chiang, 2005 | 6 | Pyocele | N.A. | E. coli | Sterile | E. coli | Cefotaxime+Other antibiotic |
| Chung-Bin, 1997 | 24 | Pyocele | S.E. | Sterile | Sterile | S. enteritidis | Ampicillin+Gentamicin |
| Hakim, 1992 | 31 | Pyocele | S.E. | Sterile | Sterile | Salmonella derby | Ampicillin+Gentamicin |
N.R.=not reported; N.A.=needle aspiration; S.E.=surgical exploration; T.D.=tube drainage.
Although uropathy can predispose to EO,5 only three cases were associated with genitourinary malformations. The pathogenesis is unclear in 2 patients with Salmonella isolation in scrotal pus but sterile blood cultures. Testicular involvement is commonly preceded by signs of severe infection and scrotal inflammation usually develops after an initial clinical improvement. The most commonly isolated bacteria was E. coli in five patients.
Nine cases presented suppurative complications (seven pyoceles and two abscesses), which were drained in all cases. Drainage can optimize microbiological diagnosis to guide antibiotic therapy. However, in the reviewed cases, blood cultures were usually positive and drainage fluid culture was the only positive sample in 2/11 newborns. To our knlowledge, this is the first report of non-surgical management of neonatal pyocele secondary to EO.6
Because of the high risk of bacteremia and systemic infection in neonatal EO, early diagnosis including Doppler ultrasound and a full sepsis workup before starting empiric antibiotic therapy seem to be necessary.