Staphylococcus aureus is the cause of 11–33% of nosocomial bloodstream infections and has a complication rate close to 50%. S. aureus accounts for 31% of isolates in the Instituto Nacional de Cancerología (INC), in Bogotá, Colombia, and is the main etiological agent of bacteremia. This study describes the risk factors for mortality caused by S. aureus bacteremia in cancer patients.
MethodsThis is a retrospective, analytical, observational cohort study of 267 cases of bacteremia caused by S. aureus. Data from all bacteremic patients with proven cancer were extracted, and variables were introduced in a multivariate analysis using a Cox proportional hazards model.
ResultsA total of 354 bacteremic patients were identified between 2001 and 2005, and 267 patients met the specified inclusion and exclusion criteria. Among these, death was considered secondary to S. aureus infection in 31%. Independent predictors of mortality related to S. aureus bacteremia in the multivariate analysis were: severity of sepsis at onset of bacteremia (HR 6.5, 95% CI 3.1–13.6), age (HR 1.03, 95% CI 1.01–1.04), non-eradicable source of infection (HR 36.3, 95% CI 5.2–254.1), heart failure (HR 10.6; 95% CI 1.8–63.7), and primary bacteremia (HR 6.3, 95% CI 1.3–31.0).
ConclusionSeverity of sepsis at the time bacteremia was detected, a non-eradicable source of infection (including primary bacteremia), and comorbid conditions were risk factors for mortality caused by S. aureus bacteremia in cancer patients. These risk factors do not differ considerably from those of patients who do not have cancer.
Staphylococcus aureus es responsible por el 11 al 33% de las bacteriemias nosocomiales y tiene una tasa de complicaciones cercana al 50%; S. aureus es responsible de 31% de los aislamientos en el Instituto Nacional de Cancerología (INC) en Bogotá, Colombia, y es el agente etiológico más importante de las bacteriemias. Este estudio tenía como objetivo describir los factores de riesgo de mortalidad ocasionada por la bacteriemia por S. aureus en pacientes con cáncer.
MétodosEste es un estudio de cohorte retrospectiva, analítico, observacion de 267 casos de bacteriemia ocasionada por S. aureus. Los datos clínicos de los pacientes con cáncer fueron obtenidos y las variables introducidas en un análisis multivariado utilizando un modelo de riesgos proporcionales de Cox.
Resultados354 pacientes bacteriemicos fueron detectados entre 2001 y 2005; 267 pacientes cumplieron con los criterios de inclusión y no fueron excluidos. 31% de los pacientes tuvieron como desenlace mortalidad secundaria a la infección por S. aureus. Los factores de riesgo de mortalidad independientes en el análisis multivariado fueron: estado de sepsis al inicio de la bacteriemia (razón de riesgos RR 6.5), edad (RR 1.03), fuente no erradicable de infección (RR 36.3), falla cardíaca (RR 10.6) y bacteriemia primaria (RR 6.3).
ConclusiónLos factores de riesgo para mortalidad ocasionada por bacteriemia por S. aureus fueron el estado de la sepsis al momento de la detección de la bacteriemia, una fuente no erradicable de infección (incluyendo bacteriemia primaria) y las patologías comórbidas. Estos factores de riesgo no varían considerablemente con respecto a pacientes sin cáncer.
Staphylococcus aureus is the second most common etiological agent of nosocomial bloodstream infections after coagulase‐negative Staphylococcus. S. aureus was responsible for 20.2% of the 24,179 cases of nosocomial bloodstream infections included in the SCOPE project, yielding an incidence rate of 10.3 cases of bacteremia per each 10,000 admissions.1S. aureus bacteremia can become complicated and progress to metastatic infection, recurrence, severe sepsis, septic shock, and death.2 The mortality rate associated with S. aureus bacteremia (11–43%) has not varied over the last few decades.3–10 Six to 12% of cases present recurrence3,11,12 and up to 31% of patients may present metastatic infection.4,13,14
Staphylococcus aureus is also reported to be the second most common cause of bloodstream infection after coagulase-negative Staphylococcus in patients with neoplastic disease.15 Among the oncological patients seen at Instituto Nacional de Cancerología (INC) during 2002, 57% of the 261 episodes of bloodstream infections were Gram-positive, and S. aureus was the main microorganism isolated (31% of all isolates).16 Similar data were reported by Carney et al at the beginning of the 1980s in the oncology unit of the Veterans Administration Medical Center in Washington, DC, where S. aureus was the main causative agent of bloodstream infection (responsible for 23% of all cases).17 However, more recent reports in developed countries have shown a lower prevalence of S. aureus bacteremia: 13% in 1998 and 8% in 2004.18
The risk factors predicting complications and mortality in patients with S. aureus bacteremia have been extensively described over the last few decades; however, the related information regarding cancer patients is scarce.19–22 The aim of the present study was to determine the mortality-predicting risk factors of S. aureus bacteremia in cancer patients.
MethodsThe INC is a 162-bed, fourth-level reference hospital for cancer patients in Bogotá, Colombia. A retrospective, analytical, observational cohort study was designed.
Patients were included if they were hospitalized and had one or more S. aureus-positive blood cultures. Patients had to have a histological diagnosis of cancer during the preceding year or have received anti-neoplastic treatment. Patients for whom clinical or microbiological information was lacking were excluded from the study, as were those with polymicrobial bacteremia.
The criteria for bloodstream infection were established according to the CDC/NHSN surveillance definition.23 Sepsis criteria consisted of at least 2 of the following inflammatory signs in the presence of infection: tachycardia (more than 90 beats per minute), tachypnea (more than 20 respirations per minute), leukocytosis or leukopenia (more than 12,000 neutrophils per microliter, less than 4000 neutrophils per microliter, or more than 10% banded neutrophils), and fever or hypothermia (more than 38°C or less than 36°C). Severe sepsis was established by documentation of organ failure secondary to infection. Septic shock was defined by the presence of severe sepsis plus hypotension that did not reverse with fluid resuscitation. Catheter-related bacteremia was defined by the differential time needed for blood samples to yield positive results or by simultaneous colonization of catheter tip and bacteremia. Significant colonization of the catheter tip was defined as a positive semi-quantitative catheter culture by the roll-plate method, in which ≥15 colony-forming units were cultured from the catheter tip.24 Catheter care was standardized during the study period and no changes were introduced.
All isolates were processed and identified with the use of automated identification cards (MicroScan, Dade Behring, USA). Clinical and Laboratory Standards Institute (CLSI) guidelines were used for the interpretation. Methicillin resistance was confirmed manually by disk diffusion testing.
Antibiotic management was standardized during the study period, particularly for neutropenic patients. Routine prophylaxis was not used, and antimicrobial formulation followed published guidelines.25 Patients hospitalized for more than 48h who developed Gram-positive bacteremia were empirically treated with vancomycin or linezolid (available after 2002) until susceptibility results were available.
Data regarding clinical aspects, microorganism characteristics, and information related to bacteremia (independent variables) were obtained from the medical records of each patient included in the study. Identified sources of infection were classified as being eradicable or non-eradicable. Eradicable sources of infection included abscesses and foreign bodies such as central venous catheters and prosthetic devices. Non-eradicable sources included skin and soft tissue, respiratory tract, urinary tract, gastrointestinal tract, endocarditis, osteomyelitis, meningitis, and the osteoarticular system. Unknown sources of infection were considered non-eradicable.
Antibiotic treatment was considered appropriate if in vitro testing showed susceptibility, and was considered opportune if started in the first 48h after identification of the bloodstream infection. The time from bacteremia detection to establishment of appropriate treatment was also recorded, as well as the duration of appropriate treatment.
The outcome (S. aureus bacteremia-related death) was analyzed over a 90-day follow-up after the onset of bacteremia, defined as the time when blood was drawn for the first culture that resulted positive. A death was considered to be S. aureus bacteremia-related when other plausible causes were excluded and when at least 1 of the following criteria was present: S. aureus-positive blood cultures at the time of death, death occurring before resolution of the signs and symptoms of bacteremia, death occurring 14 days before the onset of bacteremia, or necropsy findings confirming mortality related to bacteremia complications.
In patients who died during follow-up, the date of death caused by S. aureus bacteremia was recorded as an endpoint. All patients who died due to other causes, who were transferred to another hospital, or whose follow-up time had ended, were excluded from the data analysis, and the date of the event was recorded.
Student's t-test and the signed-rank test were used for the univariate analysis when comparing means or medians, respectively. Fisher's exact test and the chi-square test were used for comparing categorical variables. Incidence rates per 1000 patient-days (with time-to-outcome as denominator) were estimated across the different strata of independent variables. Kaplan–Meier survival functions were estimated and compared using the log-rank and Wilcoxon tests. Candidate variables for the multivariate analysis were those having a P value of 0.2 or less in the univariate analysis.
A Cox proportional hazards model, with stepwise analysis, was used for the multivariate analysis. The number of independent variables was limited to have a maximum of 10 observations per independent variable, to avoid overfitting the multivariate models. The probabilities for entering and removing variables were set at 0.15 and 0.2, respectively. Except in the construction of the stepwise model, two-tailed P values of <0.05 were considered statistically significant. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated. STATA software (version 9) was used for the statistical analysis.
This investigation was approved by the Research and Ethics Committee of each of the participating institutions (Instituto Nacional de Cancerología and Universidad Nacional de Colombia) and was classified as low risk according to Colombian legislation.
ResultsThe INC microbiology laboratory reported 354 cases of S. aureus bacteremia from January 2001 to October 2005 in its blood culture record-base; 267 complied with the inclusion and exclusion criteria and were admitted to the study. The final outcome was unknown in 15 cases, and these patients were excluded from the multivariate analysis.
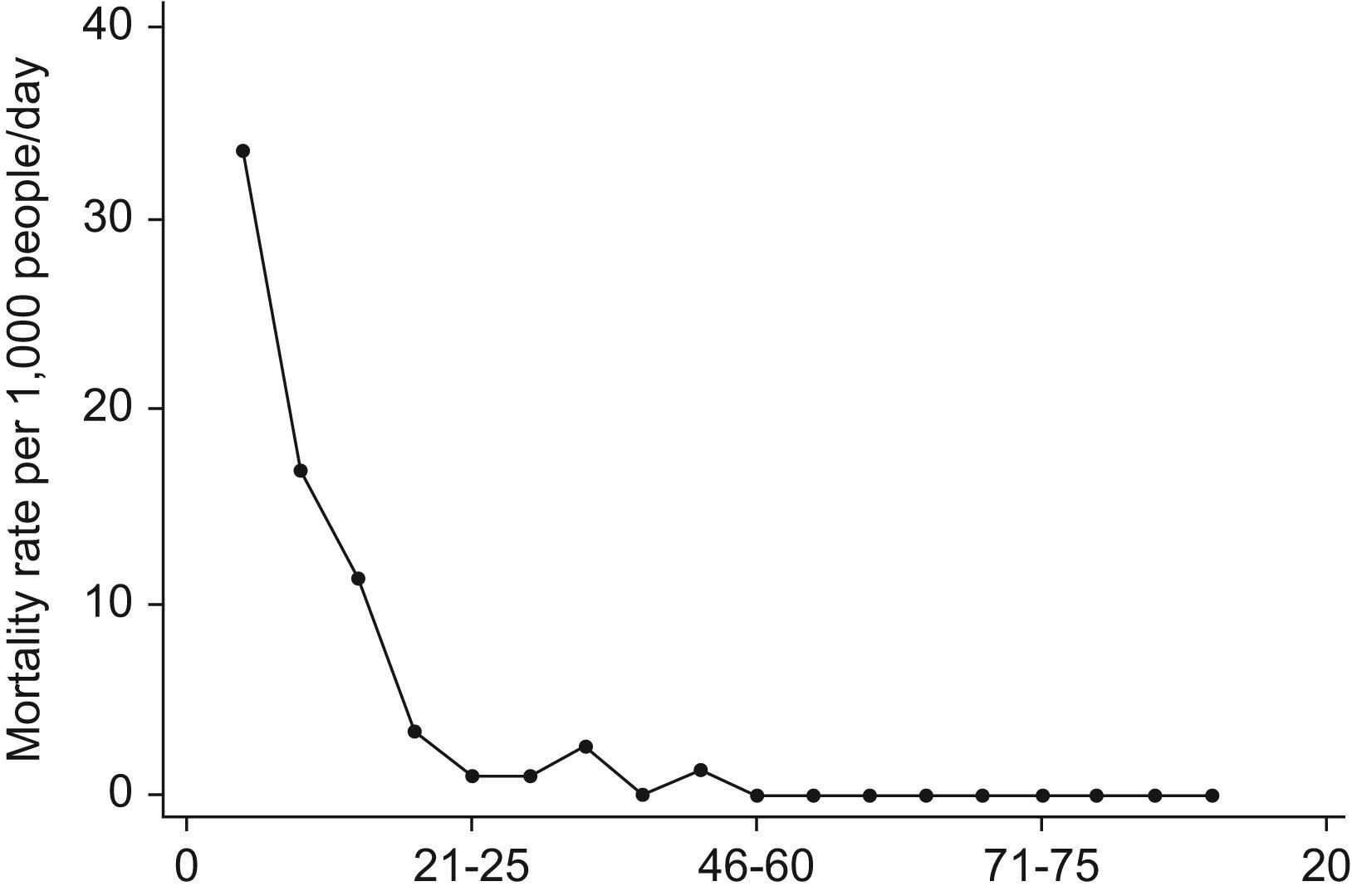
The main characteristics of the patients are shown in Table 1. Age ranged from 11 months to 82 years, with a median of 44 years. Death was the outcome in 114 patients (45.2%); 48 cases of complicated bacteremia were recorded (18%). There were 78 bacteremia-related deaths (31%) over a total at-risk time of 14,693.5 days per person. This implied a bacteremia mortality rate of 5.3 per 1000 patient-days (95% CI 4.3–6.7). The survival function of the cohort showed that mortality was highest during the first 15 days: the mortality rate during the first 5 days was 33.5 per 1000 patient-days, twice that of days 5–10, 3-fold greater than that of days 10–15, and 10-fold greater than that of days 15–20 (Fig. 1). Complicated bacteremia was present as a recurrence in 8 patients (16.7% of complicated bacteremias, 3% of all cases) and a secondary focus was found in 40 patients (15% of all cases). Metastatic seeding of bacteremia resulted in a pleuropulmonary focus (22 patients, 8.2%), kidney infection or abscess (8 patients, 3%), soft tissue abscess (7 patients, 2.6%), osteomyelitis (3 patients, 1.1%), meningitis or brain abscess (2 patients, 0.7%), and endocarditis (2 patients, 0.7%).
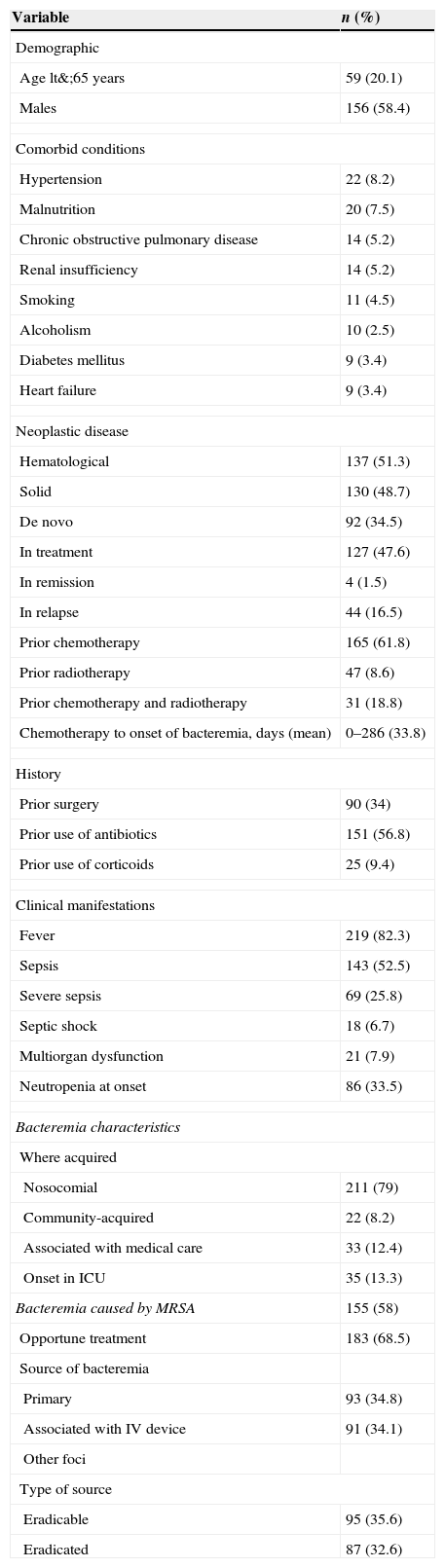
Demographic, oncological, clinical, and microbiological variables in 267 patients with cancer and Staphylococcus aureus bacteremia
| Variable | n (%) |
| Demographic | |
| Age lt&;65 years | 59 (20.1) |
| Males | 156 (58.4) |
| Comorbid conditions | |
| Hypertension | 22 (8.2) |
| Malnutrition | 20 (7.5) |
| Chronic obstructive pulmonary disease | 14 (5.2) |
| Renal insufficiency | 14 (5.2) |
| Smoking | 11 (4.5) |
| Alcoholism | 10 (2.5) |
| Diabetes mellitus | 9 (3.4) |
| Heart failure | 9 (3.4) |
| Neoplastic disease | |
| Hematological | 137 (51.3) |
| Solid | 130 (48.7) |
| De novo | 92 (34.5) |
| In treatment | 127 (47.6) |
| In remission | 4 (1.5) |
| In relapse | 44 (16.5) |
| Prior chemotherapy | 165 (61.8) |
| Prior radiotherapy | 47 (8.6) |
| Prior chemotherapy and radiotherapy | 31 (18.8) |
| Chemotherapy to onset of bacteremia, days (mean) | 0–286 (33.8) |
| History | |
| Prior surgery | 90 (34) |
| Prior use of antibiotics | 151 (56.8) |
| Prior use of corticoids | 25 (9.4) |
| Clinical manifestations | |
| Fever | 219 (82.3) |
| Sepsis | 143 (52.5) |
| Severe sepsis | 69 (25.8) |
| Septic shock | 18 (6.7) |
| Multiorgan dysfunction | 21 (7.9) |
| Neutropenia at onset | 86 (33.5) |
| Bacteremia characteristics | |
| Where acquired | |
| Nosocomial | 211 (79) |
| Community-acquired | 22 (8.2) |
| Associated with medical care | 33 (12.4) |
| Onset in ICU | 35 (13.3) |
| Bacteremia caused by MRSA | 155 (58) |
| Opportune treatment | 183 (68.5) |
| Source of bacteremia | |
| Primary | 93 (34.8) |
| Associated with IV device | 91 (34.1) |
| Other foci | |
| Type of source | |
| Eradicable | 95 (35.6) |
| Eradicated | 87 (32.6) |
A hematological neoplasm was diagnosed in 137 patients (51.3%): 54 (20.2%) acute lymphoid leukemia, 28 (10.5%) acute myeloid leukemia, 27 (10.1%) non-Hodgkin's lymphoma, 12 (4.5%) Hodgkin's lymphoma, and 6 (2.2%) multiple myeloma. Solid tumors were diagnosed in 130 patients (46.7%): 19 (7.1%) colorectal cancer, 12 (4.5%) gastric cancer, 8 (3%) breast cancer, 7 (2.6%) cervical cancer, and 84 cases (31.5%) of a variety of different tumors.
The bivariate analysis showed no differences in time between chemotherapy and bacteremia, or the average temperature, mean duration of fever, opportune time to start antibiotics, time between fever onset and detection of bacteremia, time taken to eradicate the bacteremia source, or median duration of neutropenia according to the outcome. There was no association between recurrence and outcome, or between the median or total number of complications and outcome. No treatment-related variable (appropriate treatment, opportune treatment, time to start appropriate treatment or duration of appropriate treatment) was statistically significant in the bivariate analysis.
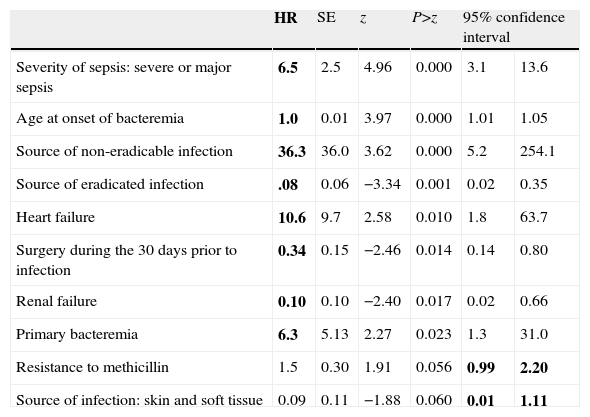
Table 2 shows the group of variables that best explained outcome in the multivariate analysis. The model shows that the severity of sepsis and age at the time bacteremia was detected (HR 6.5, 95% CI 3.1–13.6 and HR 1.03, 95% CI 1.01–1.04, respectively), the presence of a non-eradicable infection source (HR 36.3, 95% CI 5.2–254.1), heart failure (HR 10.6, 95% CI 1.8–63.7), and primary bacteremia (HR 6.3, 95% CI 1.3–31.0) were independent predictors of mortality due to S. aureus bacteremia. Having an eradicated source of infection (HR 0.08, 95% CI 0.02–0.35) or a history of surgery within 30 days before S. aureus bacteremia was detected (HR 0.33, 95% CI 0.14–0.8) independently predicted survival at 90 days.
Multivariate analysis of risk factors for mortality caused by Staphylococcus aureus bacteremia in 267 cancer patients. Instituto Nacional de Cancerología, Bogotá, Colombia (January 2001–October 2005).
| HR | SE | z | P>z | 95% confidence interval | ||
| Severity of sepsis: severe or major sepsis | 6.5 | 2.5 | 4.96 | 0.000 | 3.1 | 13.6 |
| Age at onset of bacteremia | 1.0 | 0.01 | 3.97 | 0.000 | 1.01 | 1.05 |
| Source of non-eradicable infection | 36.3 | 36.0 | 3.62 | 0.000 | 5.2 | 254.1 |
| Source of eradicated infection | .08 | 0.06 | −3.34 | 0.001 | 0.02 | 0.35 |
| Heart failure | 10.6 | 9.7 | 2.58 | 0.010 | 1.8 | 63.7 |
| Surgery during the 30 days prior to infection | 0.34 | 0.15 | −2.46 | 0.014 | 0.14 | 0.80 |
| Renal failure | 0.10 | 0.10 | −2.40 | 0.017 | 0.02 | 0.66 |
| Primary bacteremia | 6.3 | 5.13 | 2.27 | 0.023 | 1.3 | 31.0 |
| Resistance to methicillin | 1.5 | 0.30 | 1.91 | 0.056 | 0.99 | 2.20 |
| Source of infection: skin and soft tissue | 0.09 | 0.11 | −1.88 | 0.060 | 0.01 | 1.11 |
This study presents the outcome of one of the largest series of cancer patients affected with S. aureus bacteremia. The prevalence of this complication seems higher than would be expected according to the results from other centers in developed countries.18,20 Despite the advances in antimicrobial therapy, and in care and support for cancer patients, S. aureus bacteremia implies an increased risk of death in this population; 45.2% of patients who presented S. aureus bacteremia in this study died, and 30.9% died of bacteremia-related causes, rates that are similar to those seen in patients without cancer.3,9,26–29 Most patients died during the first five days.5,9,29
In keeping with the observations of Wisplinghoff et al,30 Soriano et al,31 and Guilarde et al,32 the presence of severe sepsis, septic shock, or multiple organ dysfunction was an independent predictor of mortality (HR 6.5, 95% CI 3.1–13.6; P<0.001).
Mortality occurred in non-elderly adult patients in this cohort (49.9±22.2 years, vs. 34.6±28.8 years) and age was an independent predictor of mortality in the multivariate model, with a HR of 1.03 (95% CI 1.01–1.04; P<0.0000), a previously described finding3,5–7 that was also reported in the study by Skov et al33 in patients with hematological neoplasms.
Primary S. aureus bacteremia has been cited as a predictor of death4,5,27,34 and hematogenous complications.35 The presence of a non-eradicable or non-eradicated source of infection was also an independent predictor of mortality in this study, corroborating the findings of Fowler et al36 (4.2 OR; 1.1–17 95% CI) and Jensen et al3 (OR 6.7, 95% CI 2.1–21) these factors facilitate persistence and/or recurrence of bacteremia, sepsis control, and increased risk of hematogenous spread. Heart failure was also a mortality-associated risk factor (10.6 HR; P=0.01), as has been reported by Cosgrove et al9 (OR 4.5; P=0.01).
The role of methicillin resistance as predictor of mortality and complications caused by S. aureus bacteremia is controversial. Our findings showed that methicillin resistance was one of the variables that best explained the model, even though the 95% CI was not significant (HR 1.5; 95% CI 0.99–2.2). A meta-analysis of 31 cohort studies by Cosgrove et al37 showed that methicillin resistance predicted mortality (HR 1.4, 95% CI 1.3–1.6; P<0.001), although there was significant heterogeneity (P=0.03). Currently there is no consensus on this issue: most experts believe that methicillin resistance is not an independent predictor of mortality after adjusting for other variables. In our study, multivariate analysis showed a non-significant effect of this variable on mortality, thereby reinforcing the hypothesis that associated medical conditions rather than methicillin resistance (older age, greater comorbidity, inopportune start of antibiotics, lesser intrinsic bactericidal capability of vancomycin) may be the true determinants of outcome.
In some studies, cancer is reported to be a predictor of mortality in S. aureus bacteremia.5,27 Although the design of our study did not allow us to define the weight of this association, we did evaluate variables related to neoplastic disease that could explain outcome. None of these was independently associated with mortality, and the risk factors found in the multivariate analysis were those classically described in S. aureus bacteremia in cancer-free patients. Nonetheless, the bivariate analysis enabled some aspects to be identified. When mortality related to S. aureus bacteremia was calculated according the status of each neoplastic disease, we found that de novo or relapsing neoplasm presented 37% related mortality whereas neoplasms in remission or in treatment presented 24.8% related mortality (P=0.03), although the 95% CIs for these variables were not significant.
On multivariate analysis of a cohort of 30 patients with cancer, neutropenia, and S. aureus bacteremia (from a cohort of 438 neutropenic patients with bacteremia) Gonzalez-Barca et al20 reported that septic shock, pneumonia, uncontrolled neoplasm, and absence of fluoroquinolone prophylaxis were factors predicting mortality. Moreover, mortality was lower in patients with an absolute neutrophil count (ANC) of <100 neutrophils/109/L in the bivariate analysis than those with an ANC of 100–500 neutrophils/109/L (22% vs. 33%, P=0.02). This study shows that the degree of control of the neoplastic disease rather than the interventions used were the factors determining the prognosis in these patients.
In a retrospective study of patients with S. aureus bacteremia, Venditti et al22 found that non-neutropenic patients had higher overall and attributable mortality than neutropenic patients (overall mortality 36.1% vs. 11.1%, respectively; P=0.01; attributable mortality 25% vs. 2.7%, respectively; P=0.006). Even though the analysis was bivariate, the authors postulated that the presence of neutropenia in these patients might be associated with a less intense inflammatory response and slower progression of inflammatory phenomena leading to severe sepsis and septic shock. The fact that patients with febrile neutropenia might benefit from earlier establishment of antibiotics compared to neutropenia-free patients may be another factor that would explain this tendency. Thus, later analyses should adjust the weight of neutropenia according to the beginning of appropriate or opportune antibiotic treatment, with all the difficulties involved in defining this variable.38
Our findings were similar to those of Venditti. A history of chemotherapy (HR 0.7) and neutropenia at the start (HR 0.7) or at any time during disease evolution (HR 0.6) all showed a trend to act as protective factors in the bivariate analysis, although the 95% CI was non-significant.
Our study has several limitations. The first is the fact that the number of cases proposed when calculating the sample size was not obtained. This limitation could not be avoided because the exclusion criteria eliminated a large percentage of patients with polymicrobial bloodstream infection and clinical records lacking information. Thus, the INC's active file of clinical histories was exhausted without completing the sample. Although the results of our study are consistent with reported findings and the overall behavior of the model was satisfactory, we cannot rule out that some real associations may not have been detected because of this loss of power. In addition, the nature of the data was imprecise on occasions because of the retrospective nature of the study. It is thus worth noting that no association with outcome was found involving continuous variables (with the exception of age).
In addition, the study's retrospective nature limited obtaining relevant data, such as the Karnofsky performance index or the Eastern Cooperative Oncology Group (ECOG) performance scale. Lesens et al7 used the Charlson weighted index of comorbidity (WIC) risk scale and found that a score more than or equal to 3 positively correlated to mortality (OR 3, 95% CI 1.3–5.5; P=0.006). This aspect should be clarified in future studies of patients with cancer and bacteremia.
In patients with cancer and S. aureus bacteremia, the severity of sepsis, age at the time bacteremia was detected, presence of a non-eradicable source of infection, heart failure and primary bacteremia were independent predictors of mortality due to S. aureus bacteremia. Since most of these factors cannot be modified, prevention, particularly of catheter-related infection39 early identification of colonized patients, and implementation of preventive strategies40 may the most feasible ways of avoiding the high mortality associated with this complication.
The variables explaining survival did not differ from those reported in the literature for cancer-free patients; nevertheless, methods that are more precise must be used for quantifying the degree of morbidity related to oncological disease and its relationship with the prognosis in this scenario.