Selling antibiotics without prescription is common in many countries; beyond the administrative restrictions, this practice is a risk for patients and society. The aim of the study was to evaluate the information provided by the staff of the pharmacy to a simulated patient requesting an antibiotic.
Material and methodsA prospective study was carried out in January 2013 – February 2014 in the Health Region of Tarragona, in which a mystery shopper visited 220 pharmacies requesting an antibiotic to be sold.
ResultsThe actress was not asked about allergies in 73.9% of cases and never was asked about possible pregnancy. Recommendation to see a doctor was observed in 36.1% of cases. When antibiotics were not sold, the explanation provided by the staff was reasoned only in 9.9% of the cases.
ConclusionIt is necessary and urgent to improve the training of pharmacists in dispensing antibiotics but also strengthen basic health knowledge among the population.
La dispensación de antibióticos sin receta es un hecho habitual en nuestro país sin tener en cuenta el riesgo que supone para el paciente y la sociedad. El objetivo del estudio fue evaluar la información suministrada por el personal de la oficina de farmacia a una paciente simulada que pedía un antibiótico.
Material y métodosEstudio prospectivo realizado en el período de enero de 2013 a febrero de 2014 en la Región Sanitaria de Tarragona (Cataluña), donde una compradora simulada visitó 220 farmacias pidiendo que se le vendiera un antibiótico.
ResultadosEn un 73,9% de los casos no se preguntó por las alergias y en ninguno si estaba embarazada. En un 36,1% de los casos se recomendó ir al médico. Cuando no se vendió el antibiótico, la respuesta facilitada fue razonada solo en un 9,9% de los casos.
ConclusiónEs necesario y urgente mejorar la formación profesional de los farmacéuticos en la dispensación de antibióticos y también los conocimientos básicos de salud de la población.
Since antibiotics were introduced into clinical practice in the 1940s, they have become essential drugs to treat the majority of bacterial infectious processes. Development of antibiotic resistance, especially the appearance and dissemination of multiresistant bacteria and the lack of alternative treatments, are two of the largest public health problems that currently need to be addressed.1 One of the first principles in medicine since Hippocrates is to do no harm. All interventions can potentially cause unwanted harm at the same time as benefits. However, antibiotics are sometimes sold without prescription, thinking that if they do not work, there is no risk of causing damage. This assumption is mistaken, as antibiotics used incorrectly have a risk, for both the patient and society.2
Between January 2013 and February 2014 we conducted a prospective study in the Health Region of Tarragona (Catalonia, Spain) through the mystery shopper method, detecting an important percentage of antibiotic sales without prescription. The aim of this article is to evaluate the information provided by the staff of the pharmacy when a patient requests an antibiotic.
Materials and methodsThe methodology used in this study was published recently.3 Overall, 220 pharmacies were visited. The mystery shopper stated that she was passing through and did not live in that location. She requested medication for the corresponding symptoms, feigning one of the following 3 infections: urinary tract infection, a sore throat or acute bronchitis. To ensure maximum homogeneity, there was only one mystery shopper (the principal researcher for the study [MG]), a young woman (32 years old), important characteristics for performing the sub-analysis presented herein. Four requirement levels were designed to obtain the antibiotic: in the first, medication to treat the symptoms was required; in the second, a stronger medication was required; in the third, an antibiotic was required; and in the fourth and final one, a specific antibiotic was required (amoxicillin/clavulanic acid for a urinary infection and amoxicillin for a sore throat and acute bronchitis).
After leaving the pharmacy, the researcher filled in the data collection form with all the variables of the study, including the necessary requirement level, the antibiotic sold, questions and advice given by the pharmacist (if any) and causes for non-selling when the antibiotic was not sold. We classified the antibiotics based on the teratogenic risk categories published by the Food and Drug Administration.4
ResultsIn 119 of 220 pharmacies that were visited (54.1%) an antibiotic was sold without prescription. In 88 cases (73.9%) the patient was not asked about a background of allergies to any antibiotics; moreover, in almost half of these cases (38; 43.2%) the given antibiotic was a β-lactam antibiotic. In none of the cases was the patient asked if she was pregnant before selling the antibiotic. Considering the category of the sold antibiotics according to the FDA risk classification,4 more than half of them (68; 57.1%) belonged to category B (“safe for use during pregnancy”), 39 (32.8%) were drugs classified as A (“remote risk of foetal harm”), but 12 (10.1%) were classified as C (“their use during pregnancy must be evaluated according to risk/benefit”). In two cases (1.7%) the pharmacist asked whether the patient was taking contraceptive treatment, telling her that, if so, she needed to use barrier contraceptive methods during the month when the antibiotic treatment was taken.
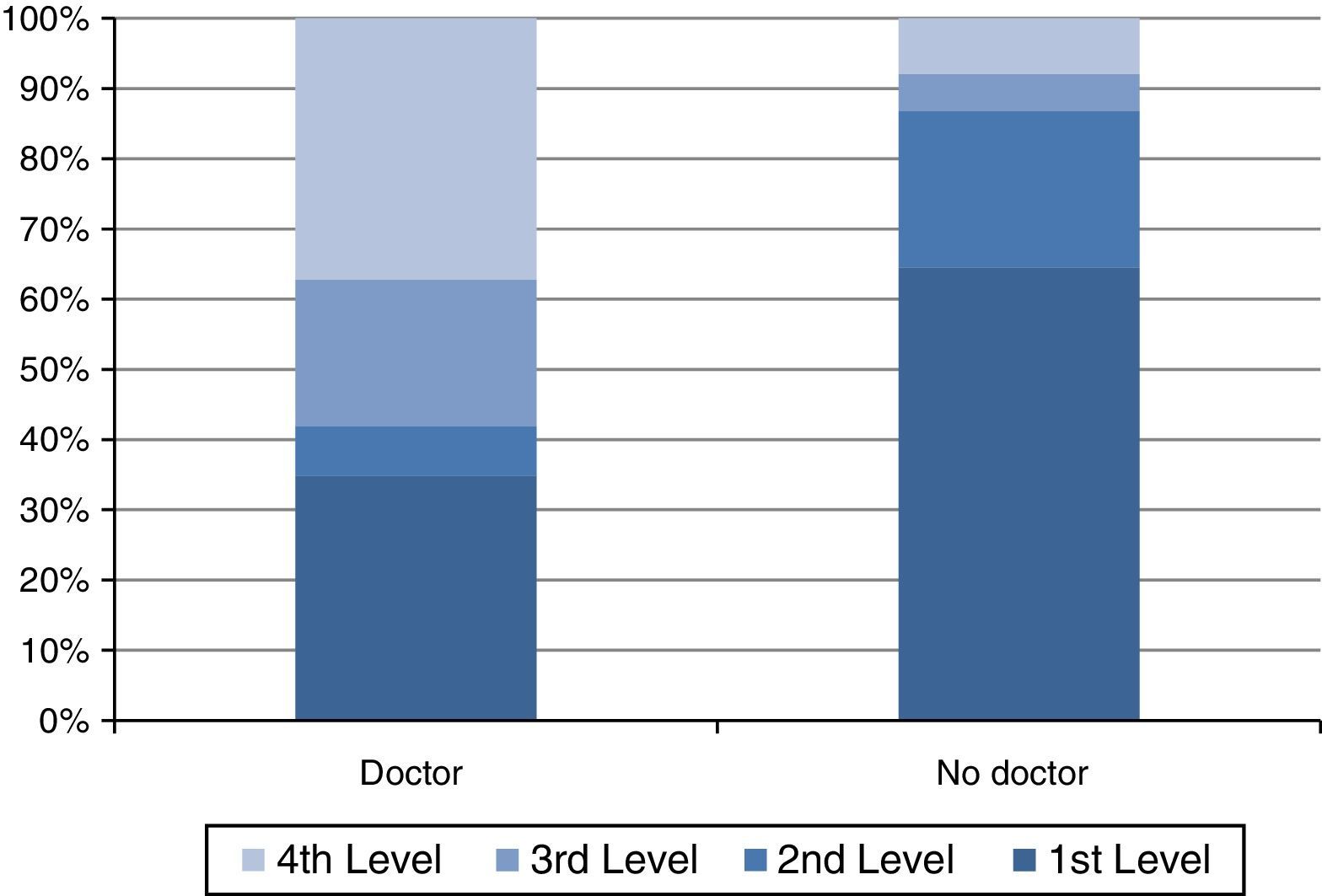
Only in 36.1% of the cases in which antibiotics were sold (43) the pharmacy staff advise, the patient to see a doctor. When consulting a doctor was not recommended, the antibiotic was sold easier (it was supplied in the first or second level) than when it was recommended in 86.6% and 41.9%, respectively (Fig. 1). An analysis according to the pathology showed that urinary infection were the case where seeing a doctor was less recommended (68.3%), followed by acute bronchitis (62.5%). The duration and treatment were explained to the patient spontaneously in almost all of the simulations (114; 95.8%) and these indications were correct, except in one case (0.9%), in which treatment with amoxicillin/clavulanic acid was recommended for 4 days.
After analysing the 101 pharmacies where antibiotics without prescription were not sold, the results showed that the justification given was an administrative reason in 70.3% of the cases (71), they referred to the prohibition of selling an antibiotic without an official prescription. In the present study, a reasoned answer was given only in 9.9% (10) of the cases, and the pharmacy staff imparted healthcare education to the patient by explaining that they could not give her the antibiotic because they did not know her medical history and they could not give her a diagnosis, which could only be given by her family doctor. In the remaining cases (20; 19.8%) both arguments were given.
DiscussionThe present study showed that in 54.1% of cases an antibiotic was dispensed without prescription. The results were even slightly worse than those obtained in a previous study with a similar methodology, which showed that antibiotics were supplied in 45.2% of the cases.5
In most cases in which an antibiotic was sold, the patient was not asked about her previous history of allergy or possible pregnancy. Apparently not asking for allergies or pregnancy when an antibiotic without prescription is dispensed is a regular practice; in Spain only in 16.9% of the cases asked about allergies and in 3.6% of cases about pregnancy in 20085; in Riyadh only 23% asked about pregnancy when dispensing antibiotics for UTI-simulated cases6; in Bogotá in any case pharmacists asked for allergies.7 Non-prescription antimicrobial and antituberculosis use is common outside of North America and northern Europe and must be accounted for in public health efforts to reduce antimicrobial resistance.8
Moreover, only one third of the pharmacies that supplied an antibiotic advised the patient to see a doctor to obtain a specific diagnosis and an appropriate treatment, even though symptoms could hide potentially serious pathologies, such as pyelonephritis, acute sinusitis or pneumonia.
Immediacy is one of the main characteristics of the present society; therefore, the accessibility to antibiotics in pharmacies has its advantages and disadvantages. Patients benefit from the sale of antibiotics without prescription as they can start treatment earlier. Nonetheless, this celerity carries an inherent risk for patients and society. Amongst the negative consequences for society we find the alarming increase of resistance to antibiotics on a global scale. For patients, the immediate risks are unnecessary antibiotic exposure and the fact that the selected treatment may not be the most appropriate one for their pathology. These variables must be considered when an antibiotic is sold without prescription, as the pharmacist does not know the patient and the patient's medical history; he/she does not have access the medical record and has not been trained to diagnose pathologies. According to the results of our study, the limitation of not knowing the patient's medical history is not replaced by making a good anamnesis before selling the antibiotic, a matter which exacerbates the practice of supplying antibiotics without prescription.
The pharmacy staff explained how to take the antibiotic in practically all of the cases, but not many recommended consulting a doctor, or asked about allergies or possible pregnancy, even though antibiotics that can be a risk for the foetus were sold (category C of the FDA). It is important to bear in mind that allergy to β-lactam antibiotics is the most frequent cause of side effects to drugs mediated by a non-specific immune mechanism and that is related to an important morbi-mortality, apart from the healthcare expenses incurred by the different manifestations of hypersensitivity and the risk to life implied for the patient.9
Probably one of the most important findings of this study is the fact that pharmacies do not comply with one of the essential roles of the community pharmacist: being the first health professional that the patient reaches out to, and whose duty it is to guide the patient appropriately to contribute to the mitigation of its symptoms and facilitate recovery from the illness. This problem is even more relevant if we take into account that the drugs involved were antibiotics and that one of the main causes of the development of resistance is their inappropriate or irrational use.
The results suggest that, in an important number of cases, pharmacy staff are either unaware of the necessary information on the medicines that are sold, as they assume that patients know the drugs they need, which aggravates in the case of antibiotics without prescription,10 or they have the knowledge but they do not apply it. Owing to the above, health education that does not only include factual aspects related to the rational use of antibiotics and the risks of selling them without prescription outside the law, but which also modifies the staff's attitude in real daily practice is clearly needed.
FundingThis study was supported by internal funding. The authors paid for the antibiotics obtained at the pharmacies. They all have been delivered to Fundació Humanitària Dr. Trueta, a non governmental organisation in charge of providing medicines to developing countries
Conflict of interestCL has received research grants from the European Commission (Sixth and Seventh Programme Frameworks), Catalan Society of Family Medicine and Instituto de Salud Carlos III. The other authors have no conflicts to declare.