Mediastinitis is an infrequent but serious complication of cardiac surgery. Antimicrobial treatment guidelines are not well established. The aim was to describe the efficacy of sequential intravenous to oral therapy in selected post-surgical mediastinitis patients.
MethodsA retrospective observational study including cases of mediastinitis after cardiac surgery, defined according to CDC criteria, at a third-level university hospital between January 2002 and December 2016. Sequential antimicrobial therapy was proposed in clinically stable patients. Rates of cure, relapse, and hospital stay were compared between patients who received sequential intravenous to oral therapy and those who received therapy exclusively by the intravenous route.
ResultsEighty-one cases were included. Sequential intravenous to oral therapy was performed in 48 (59.3%) patients on median day 15. No differences in baseline characteristics or causal microorganisms were found between the two cohorts. The average duration of antibiotic therapy was 41.2±10.09 days. The most commonly used drugs in sequential therapy were quinolones in 31 (64.6%) cases and rifampicin, always in association with another antibiotic, in 25 (52.1%). Hospital stay was shorter in the sequential therapy group (57.57±34.03 vs. 84.35±45.67; P=0.007). Cure was achieved in 77 (92.8%) patients. Overall in-hospital mortality was less frequent in the group that received sequential therapy (2.1% vs. 15.2%; P=0.039). There were no differences in relapse between the two cohorts (4.2% vs 9.1%; P=0.366).
ConclusionSequential antimicrobial treatment in selected patients with post-surgical mediastinitis may be as effective as exclusively intravenous treatment, reducing risks, hospital stay and associated costs.
La mediastinitis es una complicación grave pero infrecuente de la cirugía cardiaca. Las pautas de tratamiento antimicrobiano no han sido bien definidas. El objetivo es describir la eficacia del tratamiento antimicrobiano secuencial, de intravenoso a oral, en pacientes seleccionados con mediastinitis.
MétodoEstudio observacional retrospectivo en el que se incluyeron los casos de mediastinitis relacionados con la cirugía cardiaca, según criterios del CDC, en un hospital universitario entre enero de 2002 y diciembre de 2016. Una vez estabilizados los pacientes, se propuso completar el tratamiento antimicrobiano de forma secuencial, pasando de la vía intravenosa a la oral. Se compararon las tasas de curación, las recidivas y la estancia hospitalaria entre los pacientes que recibieron ambos regímenes.
ResultadosSe incluyeron 81 casos. El tratamiento antimicrobiano secuencial se utilizó en 48 (59,3%) pacientes, en una media de 15días. No se encontraron diferencias respecto a las características basales y microorganismos causales en ambos grupos. La duración media del tratamiento antibiótico fue de 41,2±10,09días. Los antimicrobianos más utilizados en el tratamiento secuencial fueron quinolonas en 31 (64,6%) y rifampicina, siempre asociada a otro antibiótico, en 25 (52,1%). La estancia hospitalaria fue menor en el grupo con tratamiento secuencial (57,57±34,03 vs. 84,35±45,67; p=0,007). En conjunto, curaron 77 (92,8%) pacientes. La mortalidad hospitalaria fue inferior en el grupo tratado secuencialmente (2,1% vs. 15,2%; p=0,039). No hubo diferencias en recidivas entre ambos grupos (4,2% vs 9,1%; p=0,366).
ConclusiónEl tratamiento antimicrobiano secuencial en pacientes con mediastinitis posquirúrgica seleccionados puede tener una eficacia similar al tratamiento exclusivamente intravenoso, permitiendo reducir riesgos y costes asociados.
Mediastinitis is a serious complication of cardiac surgery that affects soft tissues, bones and biomaterials, and frequently produces bacteremia.1 Its incidence is between 1% and 4%, depending on the definition used, and is associated with mortality rates between 5% and 47%.2–4 Combined medical and surgical treatment is generally required and it is associated with an increase in hospital stay and costs.5–7 The best therapeutic approach is still unclear.8,9 An empirical broad-spectrum therapy must be used, proceeding to de-escalation depending on etiology and susceptibility profile. Six weeks of therapy are recommended, usually intravenous. There is currently little evidence regarding sequential intravenous to oral therapy, although it has been shown to be effective in other similar infections such as bacteremia, endocarditis and osteomyelitis.10–14 It is worthy of mention that a recently published clinical trial showed that sequential intravenous to oral therapy was non-inferior to continued intravenous antibiotic therapy in selected patients with left-sided endocarditis.14 The objective of this study was to evaluate our experience of sequential antimicrobial therapy in patients with mediastinitis after cardiac surgery.
MethodsStudy design and patientsThis was a retrospective observational study that included all adult patients diagnosed with mediastinitis after cardiac surgery at the University Hospital Virgen Macarena, Seville, Spain, between January 2002 and December 2016. Our hospital is a tertiary reference center for cardiac surgery. All patients met the criteria for post-surgical mediastinitis established by the Centre Disease Control (CDC). Mediastinitis must meet at last 1 of the fllowing criteria: 1. Patient has organism cultures from mediastinal tissue or fluid obtained during a surgical operation or needle aspiration. 2. Patient has evidence of mediastinitis seen during a surgical operation or histopatologic examination. 3. Patient has at least 1 of the followings signs or symtoms with no other recognized cause: fever (>38°C), chest pain, or sternal instability AND at least of the following: purulent discharge from mediastinal area, organisms cultured from blood or discharge from mediastinal area, mediastinal widening on radiography.15 There has been an infection surveillance control team in cardiac surgery since the year 2000. All cases received antibiotic prophylaxis with cefazolin 2g administered 1h before the intervention and over the next 24h, except for those allergic to beta-lactams, when intravenous vancomycin 1000mg was used as close as possible to the surgical intervention.
During the diagnostic process or the operation, samples were obtained from all patients for blood cultures and wound aspirate cultures. Patients received empirical therapy with vancomycin 15mg/kg/day and ceftazidime 2g every 8h intravenously until the microbiological results were available. Patients subsequently continued with targeted intravenous therapy for an average of 2 weeks, required to stabilize the patient and rule out complications. At this point, the possibility of using sequential therapy was assessed, for which the patient had to meet all of the following criteria: (a) clinical stability (hemodynamic stability without the need for vasoactive amines, afebrile for at least 48h); (b) absence of collections and no need for reoperation; (c) absence of bacteremia, through the practice of blood cultures (systematically at 48–72h when the etiology was Staphylococcus aureus); (d) availability of suitable oral options, based on susceptibility profile and pharmacokinetic characteristics; (e) normal gastrointestinal function allowing sufficiently high plasma concentrations of antibiotics to be reached to achieve bacterial killing. These criteria were established based on experience of sequential intravenous to oral therapy in other infections.10–12
Variables and definitionsBaseline characteristics were recorded such as age, sex, the presence of comorbidities such as diabetes mellitus, hypertension, smoking, obesity, chronic obstructive pulmonary disease, chronic kidney disease, comorbidity rate assessed by the Charlson index16 and the presence of other predisposing factors, such as previous sternotomy, type of surgery, use of mammary artery (one or both), reasons for reoperation and post-surgical complications. The following were also recorded: the most frequent symptoms, microorganisms identified, therapy performed, the total number of procedures required, duration of hospital stay, cure rate, in-hospital mortality, relapse rate and long-term mortality. This manuscript was reported following the STROBE recommendations.17 The study was approved by the Center's Ethics Committee.
Statistical analysisA descriptive statistical analysis was carried out, comparing the characteristics of patients with sequential therapy and those treated exclusively by the intravenous route. Qualitative variables were expressed as proportions, and quantitative variables as means and standard deviation. In bivariate analysis, the Chi-square test or Fisher's test was used for qualitative variables, and the Student's t-test for quantitative variables. Variables with a value of P<0.05 were considered significant in models. PASW Statistics 18 (IBM SPSS, Chicago, IL, USA) was used for statistical analysis.
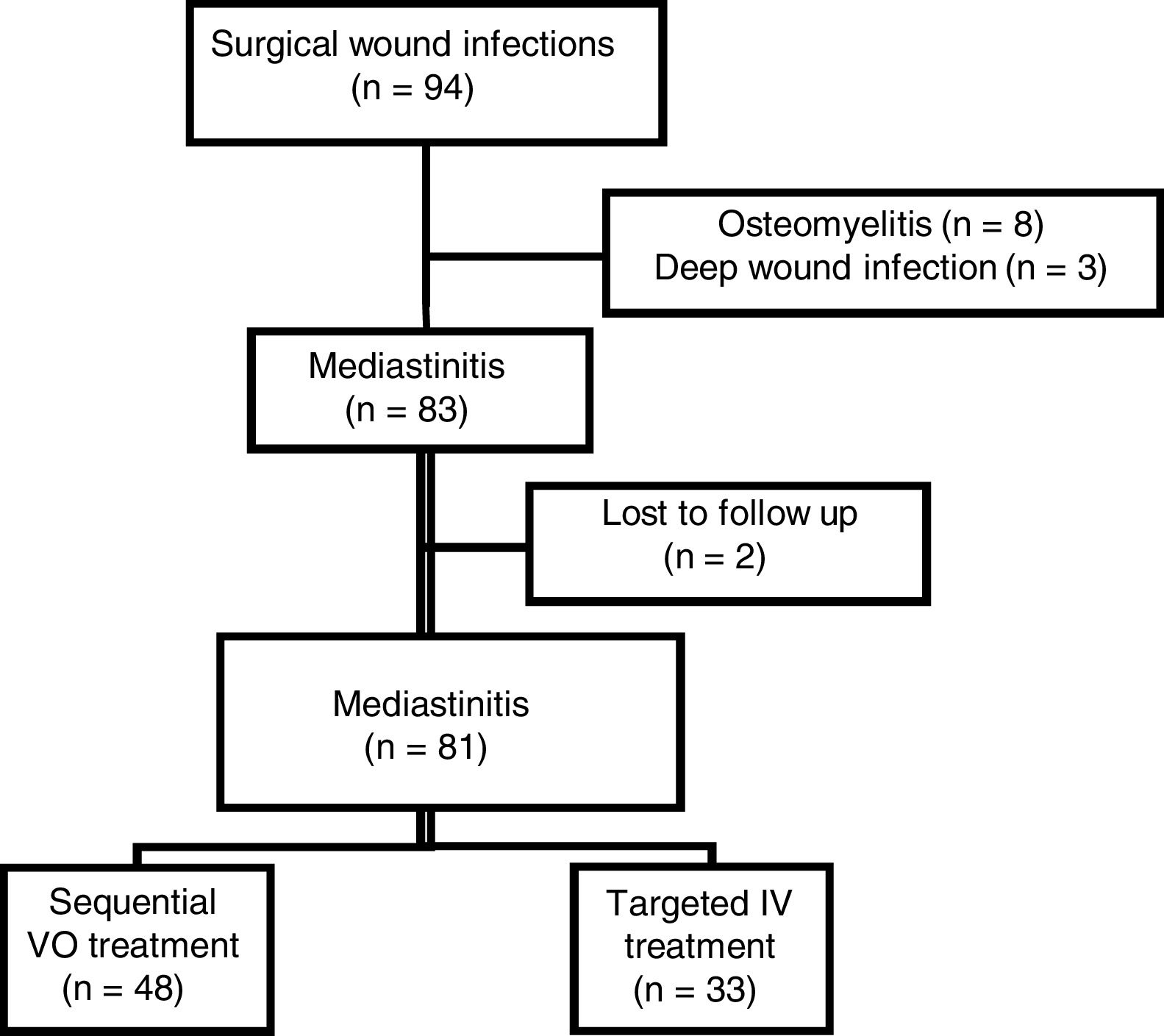
ResultsA total of 94 cases of surgical wound infection were selected. Eight cases were excluded due to sternal osteomyelitis, 3 due to deep surgical wound infection with uncertain mediastinal involvement and 2 cases were lost to follow-up (Fig. 1 suppl). Eighty-one cases of mediastinitis were finally included: the mean age was 68 (± 8.7) years, and 63 (75.9%) were males. A total of 48 (59.3%) patients received sequential intravenous to oral therapy, and 33 (40.7%) received intravenous therapy. The different types of antimicrobial treatment used during the study period are described in Fig. 1. Table 1 shows the baseline characteristics of the study population and types of cardiac intervention. There were no differences between the two cohorts, except for a predominance of males in the group treated intravenously (64.6% vs 90.9%; P=0.007). The mean follow-up was 3.3 years (range: 0.5–4.5 years). Figure 2
Baseline characteristics.
| Total(n=81) | Sequential therapy(n=48) | Intravenous therapy(n=33) | P-value | |
|---|---|---|---|---|
| Median age (SD) | 66.76 (8.70) | 66.50 (8.16) | 66.81 (8.80) | 0.87 |
| Males (percentage) | 61 (75.3%) | 31 (64.6%) | 30 (90.9%) | 0.007 |
| Diabetes mellitus | 44 (54.3%) | 25 (52.1%) | 19 (61.3%) | 0.42 |
| Chronic obstructive pulmonary disease | 12 (14.8%) | 7 (14.6%) | 5 (16.7%) | 0.52 |
| Chronic kidney disease | 10 (12.3%) | 6 (12.5%) | 4 (12.9%) | 0.61 |
| BMI≥30 | 32 (39.5%) | 19 (39.6%) | 13 (40.6%) | 0.92 |
| Charlson index, median (SD) | 4.7 (±2.13) | 4.8 (±2.31) | 4.7 (±1.84) | 0.97 |
| Coronary artery bypass graft | 42 (51.8%) | 29 (60.4%) | 13 (40.6%) | 0.82 |
| Valve surgery | 25 (30.8%) | 15 (31.3%) | 10 (31.3%) | 0.59 |
| Coronary artery bypass graft plus valve surgery | 9 (11.1%) | 2 (4.2%) | 7 (21.9%) | 0.19 |
BMI, body mass index; SD, standard deviation.
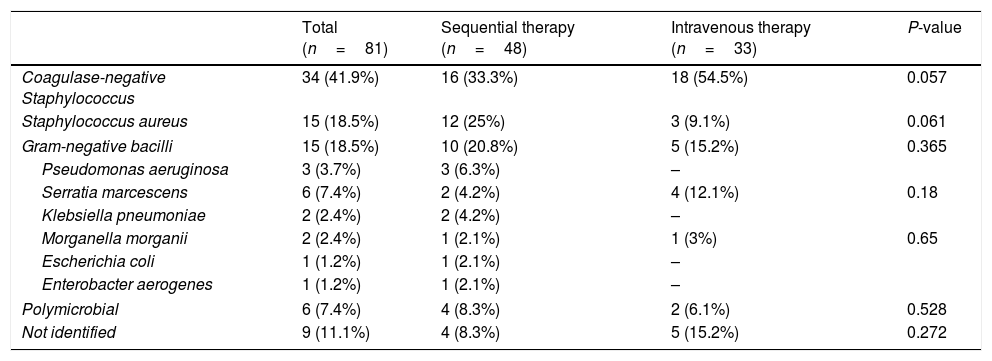
The isolated microorganisms (Table 2) showed no differences between the two cohorts. The most commonly isolated microorganisms were coagulase-negative Staphylococci, followed by S. aureus and gram-negative bacilli. In 6 cases the etiology was polymicrobial, and 9 cases failed to isolate microorganisms. The main clinical findings at diagnosis of mediastinitis are shown in Table 3, with no differences found between the cohorts (Table 3).
Etiology.
| Total (n=81) | Sequential therapy (n=48) | Intravenous therapy (n=33) | P-value | |
|---|---|---|---|---|
| Coagulase-negative Staphylococcus | 34 (41.9%) | 16 (33.3%) | 18 (54.5%) | 0.057 |
| Staphylococcus aureus | 15 (18.5%) | 12 (25%) | 3 (9.1%) | 0.061 |
| Gram-negative bacilli | 15 (18.5%) | 10 (20.8%) | 5 (15.2%) | 0.365 |
| Pseudomonas aeruginosa | 3 (3.7%) | 3 (6.3%) | – | |
| Serratia marcescens | 6 (7.4%) | 2 (4.2%) | 4 (12.1%) | 0.18 |
| Klebsiella pneumoniae | 2 (2.4%) | 2 (4.2%) | – | |
| Morganella morganii | 2 (2.4%) | 1 (2.1%) | 1 (3%) | 0.65 |
| Escherichia coli | 1 (1.2%) | 1 (2.1%) | – | |
| Enterobacter aerogenes | 1 (1.2%) | 1 (2.1%) | – | |
| Polymicrobial | 6 (7.4%) | 4 (8.3%) | 2 (6.1%) | 0.528 |
| Not identified | 9 (11.1%) | 4 (8.3%) | 5 (15.2%) | 0.272 |
Etiology of bacteremia in 31 patients: Coagulase-negative Staphylococcus 14, Gram-negative bacilli 12, S aureus 5, Propionibacterium acnes 1, polymicrobial 2.
Clinical findings at diagnosis.
| Total (n=81) | Sequential therapy (n=48) | Intravenous therapy (n=33) | P-value | |
|---|---|---|---|---|
| Wound exudate | 71 (87.6%) | 43 (89.6%) | 28 (87.5%) | 0.77 |
| Signs of inflammation in surgical wound | 59 (72.8%) | 35 (72.9%) | 24 (75%) | 0.83 |
| Fever | 56 (69.1%) | 36 (75%) | 20 (62.5%) | 0.23 |
| Sternal dehiscence | 54 (66.6%) | 29 (60.4%) | 25 (78.1%) | 0.09 |
| Chest pain | 36 (44.4%) | 23 (47.9%) | 13 (40.6%) | 0.52 |
| Bacteremia | 31 (38.2%) | 17 (41.5%) | 14 (56%) | 0.25 |
| Severe sepsis | 9 (11.1%) | 4 (8.3%) | 5 (15.6%) | 0.25 |
Treatment was medical-surgical, except in 17 cases that did not undergo surgery. Surgical therapy was less frequent in the group that received sequential therapy (70.8% vs. 93.9%; P=0.010) compared to the one that continued with intravenous therapy. Fourteen (82.4%) of the 17 cases that were not operated on, received sequential therapy. Patients who did not receive surgical therapy for whatever reason (patient refusal, absence of data on sepsis and sternal instability, and good response to therapy with vacuum aspiration system therapy fall outside the scope of the present study; hence, all cases met the clinical, microbiological and/or radiological criteria for mediastinitis, according to the diagnostic criteria of the CDC.15 The median number of days of intravenous antibiotics until sequential therapy was 15, with standard deviation of 10 days. In this group, the antimicrobials most frequently used in sequential treatment were combination therapy with rifampicin and quinolones in 25 (52.1%) cases, quinolones alone in 9 (18.7%), followed by trimethoprim-sulfamethoxazole in 4 (8.3%) and linezolid in 2 (4.2%) cases. The main regimens used are summarized in Table 4. In patients treated exclusively with intravenous antibiotics, the most commonly used antimicrobials were glycopeptides in 22 (66%) cases, followed by beta-lactams in 11 (33%), linezolid in 4 (12%), carbapenems in 4 (12%), and daptomycin in 1 (3%) case. Sequential therapy was used in 14 (82.4%) of the 17 patients who were not operated on.
Main antibiotics used in sequential therapy.
| Etiological microorganism | Antimicrobial treatment | Total (%) |
|---|---|---|
| Coagulase-negative Staphylococcus | Quinolones-rifampicin | 11 (56.2%) |
| Linezolid-rifampicin | 2 (12.5%) | |
| TMP/SMXa-rifampicin | 2 (12.5%) | |
| Staphylococcus aureus | Quinolones-rifampicin | 12 (100%) |
| Gram-negative bacilli | Quinolones | 9 (90%) |
| TMP/SMT- | 1 (10%) |
There were no differences between the two cohorts regarding the overall duration of antibiotic therapy (41.22±10.46 vs. 41.43±9.41 days; P=0.93). The final results are summarized in Table 5. Hospital stay was shorter in the group with sequential therapy (57.57±34.03 vs. 84.35±45.67 days; P=0.007) and in-hospital mortality was also lower (2.1% vs 15.2%; P=0.039).
Final results and evolution.
| Total | Sequential therapy | Intravenous therapy | P-value | |
|---|---|---|---|---|
| (n=81) | (n=48) | (n=33) | ||
| Cure | 75 (92.5%) | 47 (97.9%) | 28 (84.8%) | 0.027 |
| In-hospital mortality | 6 (7.4%) | 1 (2.1%) | 5 (15.2%) | 0.039 |
| Recurrence | 5 (6.1%) | 2 (4.2%) | 3 (9.1%) | 0.366 |
| Mortality during follow-up | 19 (23.4%) | 8 (16.7%) | 11 (33.3%) | 0.071 |
| In-mortality in operated | ||||
| Yes | 5 (6.1%) | 0 | 5 (15%) | 0.167 |
| No | 1 (6.1%) | 1 (2.0%) | 0 | |
| Average hospital stay (SD), days | 67 (±40.44) | 57.57 (±34.03) | 84.35 (±45.67) | 0.007 |
SD, standard deviation.
In selected patients with post-surgical mediastinitis who were clinically stable with normal gastrointestinal function and did not present collections or persistent bacteremia, sequential intravenous to oral therapy was as effective as intravenous therapy, and was also associated with a reduction in hospital stay.
The most frequently isolated microorganism is consistent with that isolated in other recent studies of mediastinitis.18,19 Other previous studies, however, showed that S. aureus was the most frequent microorganism.2,20
Current evidence regarding the treatment for mediastinitis is very scarce and there are no clinical trials available, so that evidence is based on expert opinion. There is also little evidence on sequential therapy. In only a few small case series have favorable results been reported in patients who received sequential antimicrobial therapy, mostly those with a staphylococcal etiology.7,12,21 Likewise, there is a scarcity of data on the prognostic impact of adding rifampicin.13 None of these studies compared their results against patients who continued with intravenous therapy. We used a sequential intravenous-to-oral therapy algorithm, based on favorable experience with other entities such as bacteremia, osteomyelitis and even endocarditis.10–14 In post-surgical mediastinitis, these types of infection usually coincide, so that this strategy could be useful once the patient is in a stable condition, drainage of collections has been carried out, and the bacteremia has been resolved. The association of antimicrobials for sequential therapy was based on the susceptibility of the microorganisms and on previous experience with staphylococcal infections in which the combination of fluoroquinolones with rifampicin was effective.11 Nevertheless, we cannot rule out the effectiveness of monotherapy, as is the case in infections due to gram-negative bacilli. Based on expert recommendations, six weeks are generally used for mediastinitis therapy,8,9 although there are no studies to show whether a shorter period could be equally effective. Since this was not the purpose of our study, we decided to follow the established recommendations.
Sequential therapy was introduced in well selected patients who were expected to have a better prognosis. The aim of the study was to describe the clinical results of selected patients with sequential therapy. Since the two cohorts are not comparable, it is not possible to conclude that oral was superior to intravenous therapy. We decided to include and compare two cohorts in order to have a reference for the prognosis of patients treated with the standard therapeutic strategy. Hospital stay was significantly shorter in the group that received sequential therapy compared to the group receiving intravenous therapy only. It is pointed out that, for the purposes of comparison of hospital stay, the total length of the patient's hospital stay was considered from initial intervention to patient discharge, after the diagnosis and treatment of mediastinitis. During the follow-up period, no differences in recurrence or mortality were observed between the two cohorts.
We consider that the results set out here are outstanding because they provide evidence of the effectiveness of sequential therapy in mediastinitis after cardiac surgery. Some observational studies have addressed the safety and efficacy of switching from intravenous to oral therapy in the treatment of endocarditis or bacteremia.10–14 A recent clinical trial conducted by Iversen et al.14 concluded that a shift from initial intravenous to oral antibiotic therapy was noninferior to continued intravenous antibiotic therapy in patients with left-sided endocarditis due to streptococcus, E. faecalis, S. aureus, or coagulase-negative staphylococci who were clinically stable and had had an adequate response to initial therapy. It should be noted that, since there are no specific recommendations for antimicrobial therapy in patients with post-surgical mediastinitis, our results help generate evidence. The major benefit of being able to perform sequential therapy is that patients who meet the criteria described above can be discharged earlier, which leads to earlier prevention of possible nosocomial infections and reduced costs due to shorter hospital stays and less use of resources.
The strengths of our study are that the results provide some evidence for the treatment of mediastinitis. In addition, although there was no etiological diagnosis in some cases, sequential therapy was used, generally combined, and with no differences in the number of recurrences or final outcomes. The main limitations of our study are those inherent in its retrospective, single-center, observational design. The number of cases included in the series was relatively low, which may have influenced the ability to detect statistically significant differences between the cohorts compared. Since the study period was long, we cannot exclude the beneficial effect of other therapeutic measures, such as the use of vacuum systems. We did not collect data about the rate of nosocomial infections in the compared cohorts, although by definition, it can be assumed that the frequency in patients with sequential therapy was zero.
In conclusion, sequential antimicrobial therapy was an effective strategy in patients with post-surgical mediastinitis and in a stable condition, and was associated with a reduction in hospital stay and healthcare costs.
FundingThis work was supported by the Plan Nacional de I+D+i and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI; RD16/0016/0001) cofinanced by the European Development Regional Fund “A way to achieve Europe” ERDF. The funders were not involved in the design, analysis, decision to publish or preparation of the manuscript.
Conflict of interestsLELC has served as spokesman for Merck, Sharp and Dohme, and Angellini, has received research support from Novartis, and has served as trainer for Merck, Sharp and Dohme. The rest of the authors declare that they have no competing interests.
We would like to gratefully acknowledge one each of the members of the different departments, since without support the work could not have been completed.