To analyse factors associated with short-term mortality in elderly patients seen in emergency departments (ED) for an episode of infectious disease.
Materials and methodsA prospective, observational, multicentre, analytical study was carried out on patients aged 75years and older who were treated in the ED of one of the eight participating hospitals. An assessment was made of 26 independent variables that could influence mortality at 30days. They covered epidemiological, comorbidity, functional, clinical and analytical factors. Multivariate logistic regression analysis was performed.
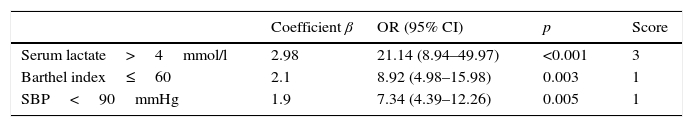
ResultsThe study included 488 consecutive patients, 92 (18.9%) of whom died within 30days of visiting the ED. Three variables were significantly associated with higher mortality: severe functional dependence, with Barthel index≤60 [odds ratio (OR) 8.92; 95% confidence interval (CI): 4.98–15.98, p=0.003], systolic blood pressure <90mmHg [OR 7.34; 95% CI: 4.39–12.26, p=0.005] and serum lactate >4mmol/l [OR 21.14; 95% CI: 8.94–49.97, p=0.001]. The area under the curve for the model was 0.971 (95% CI: 0.951–0.991; p<0.001).
ConclusionsSeveral factors evaluated in an initial assessment in the ED, including the level of functional dependence, systolic blood pressure and, especially, serum lactate, were found to determine a poor short-term prognosis in the elderly patients who presented with an episode of an infectious disease.
Analizar los factores asociados a la mortalidad a corto plazo en los pacientes ancianos que acuden al servicio de urgencias (SU) por un episodio de infección.
Material y métodosEstudio observacional, prospectivo, multicéntrico y analítico. Se incluyó consecutivamente a pacientes de 75 o más años atendidos en 8 servicios de SU por un proceso infeccioso. Se analizaron 26 variables independientes (epidemiológicas, de comorbilidad, funcionales, clínicas y analíticas) que pudieran influir en la mortalidad a corto plazo (30días). Se realizó un estudio multivariable mediante regresión logística.
ResultadosSe incluyó a 488 pacientes, de los que 92 (18,9%) habían fallecido a los 30días tras su consulta en el SU. Tres variables se asociaron de forma significativa con la mortalidad: la dependencia funcional basal grave con índice de Barthel ≤60 (odds ratio [OR] 8,92; intervalo de confianza [IC] del 95%: 4,98-15,98, p=0,003), la existencia de una presión arterial sistólica (PAS)<90mmHg (OR 7,34; IC95%: 4,39-12,26, p=0,005) y lactato sérico >4mmol/l (OR 21,14; IC 95%: 8,94-49,97, p=0,001). El área bajo la curva-ROC del modelo fue 0,971 (IC 95%: 0,951-0,991; p<0,001).
ConclusionesExisten varios factores disponibles tras una primera atención en el SU—entre ellos la valoración funcional, la PAS y, el más importante, el lactato sérico—que determinan un mal pronóstico a corto plazo del paciente anciano que consulta por un proceso infeccioso.
The number of patients over 75 years of age who attend emergency departments (EDs) due to infection has increased significantly over the last 10years (from 24.8% to 31.7%; p<0.001),1 as has the severity of the condition and short-term mortality (30days).1–3 Suspecting and confirming infection in the ED is particularly important in elderly patients owing to their susceptibility to infection and infection severity, especially given that the clinical manifestations of infection are often nonspecific and variable.4 This hinders the early detection of infection in these patients and results in a false diagnosis and subsequent erroneous patient referral, inappropriate complementary and analytical tests,5 the administration of unnecessary antimicrobials in more than 50% of cases or their delayed administration when their correct and early administration is vital for a positive patient outcome.6–8 Immunosenescence leads to immune cell function deterioration and diminished humoral immune function, as well as a chronic proinflammatory state that alters the production of cytokines, chemokines and some biomarkers.4
The challenge for emergency departments is to detect elderly patients at high vital risk and/or with severe infection (sepsis, severe sepsis or septic shock [SS]) as early as possible (from triage or the initial patient assessment), based purely on the patient's past medical history, physical examination and complementary tests that emergency departments usually have available.5,6
In terms of objective tools to assist clinicians in establishing a prognosis and identifying the severity of the infection, the functional geriatric assessment (Lawton IADL scale or the Barthel index), comorbidities (Charlson index) and a reduced level of consciousness,6 as well as biomarkers and serum lactate, have come to the fore in recent years and are used by a growing number of EDs.9 Serum lactate, considered the best marker of hypoperfusion and tissue hypoxia, is included in all the emergency department assessment guidelines for patients with sepsis, severe sepsis and SS.9,10 Patients with concentrations >2mmol/l should be closely and clinically monitored as it is an independent predictor of poor clinical progression, mortality and severity of severe sepsis and SS.9,10 However, few studies have been conducted specifically in patients >75 years of age.11
In light of the above, the aim of this study was to determine which identifiable factors that are generally used in the initial emergency department assessment, including baseline and functional status, are related to short-term mortality in elderly patients (≥75 years) diagnosed with infection.
MethodsA descriptive, multi-centre, analytical and observational study conducted at the 8 emergency departments of the participating investigators (Annex), belonging to the INFURG-SEMES (Emergency Department Infections Study Group of the Spanish Society of Emergency Medicine) network of centres. Patients ≥75years of age who completed 30 days of follow-up with a diagnosis of infection were consecutively enrolled by chance (when the investigators were on duty) upon clinical diagnosis of the infection in the EDs. The variables were recorded on an encrypted electronic case report form (online). The various criteria, definitions and parameters were defined in advance by the INFURG-SEMES scientific committee and were agreed by the investigators. The study was approved by the Hospital Universitario de Basurto Independent Ethics Committee and met the ethical standards of all the participating centres. All the encrypted data were kept strictly confidential. Patients or family members were informed both orally and in writing, and informed consent was required prior to enrolment. The study did not involve any therapeutic procedure or have any clinical implications.
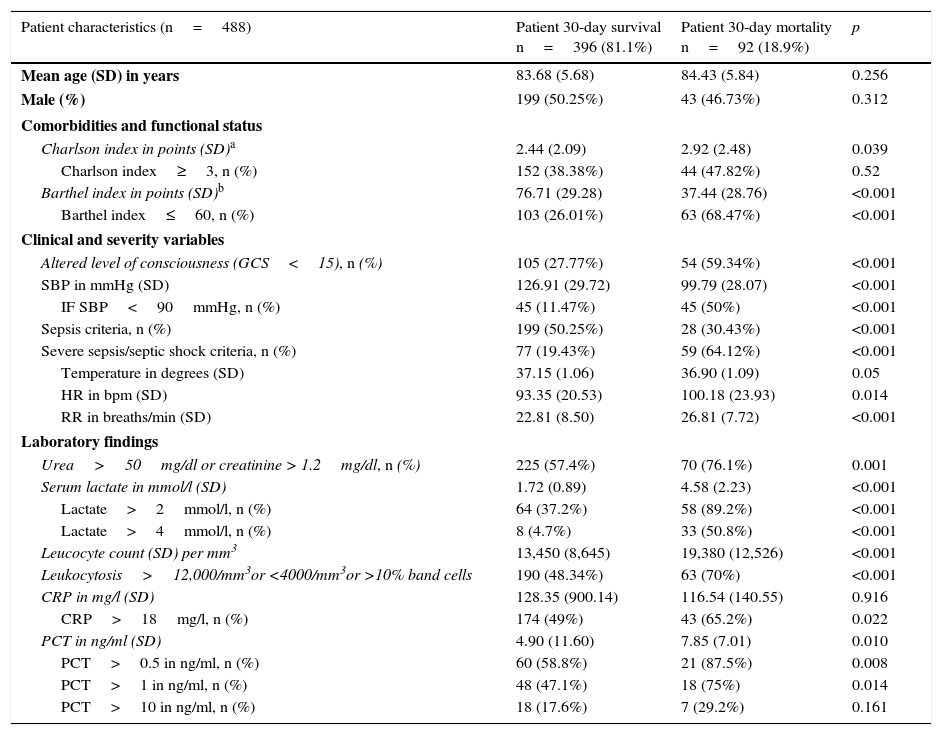
Unadjusted 30-day mortality was considered a dependent variable. Independent variables that were deemed to be able to support the prognosis during the patient's initial assessment in the ED were chosen, as detailed in Table 1: demographic variables (age, gender), comorbidity (Charlson index12 and dichotomised index≥3), functional variables (Barthel index13 and dichotomised index≤60), clinical variables (altered level of consciousness, systolic blood pressure [SBP] and SBP<90mmHg, sepsis, severe sepsis or septic shock criteria and their defining variables according to the 2001 International Sepsis Definitions Conference14) and analytical variables (kidney failure if urea >50mg/dl or Cr>1.2mg/dl), leucocyte count, concentration of serum lactate (mmol/l), C-reactive protein (CRP) and procalcitonin (PCT). Serum lactate 5–20mg/dl (0.55–2.22mmol/l), PCT<0.5ng/ml and CRP 0–18mg/l were adopted as normal reference values as agreed between the participating centres for patients ≥75 years, and these were dichotomised in accordance with the recommendations of a recent review.9
Clinical–epidemiological and analytical characteristics of patients over the age of 75 treated for infection in the ED (univariate analysis).
| Patient characteristics (n=488) | Patient 30-day survival n=396 (81.1%) | Patient 30-day mortality n=92 (18.9%) | p |
|---|---|---|---|
| Mean age (SD) in years | 83.68 (5.68) | 84.43 (5.84) | 0.256 |
| Male (%) | 199 (50.25%) | 43 (46.73%) | 0.312 |
| Comorbidities and functional status | |||
| Charlson index in points (SD)a | 2.44 (2.09) | 2.92 (2.48) | 0.039 |
| Charlson index≥3, n (%) | 152 (38.38%) | 44 (47.82%) | 0.52 |
| Barthel index in points (SD)b | 76.71 (29.28) | 37.44 (28.76) | <0.001 |
| Barthel index≤60, n (%) | 103 (26.01%) | 63 (68.47%) | <0.001 |
| Clinical and severity variables | |||
| Altered level of consciousness (GCS<15), n (%) | 105 (27.77%) | 54 (59.34%) | <0.001 |
| SBP in mmHg (SD) | 126.91 (29.72) | 99.79 (28.07) | <0.001 |
| IF SBP<90mmHg, n (%) | 45 (11.47%) | 45 (50%) | <0.001 |
| Sepsis criteria, n (%) | 199 (50.25%) | 28 (30.43%) | <0.001 |
| Severe sepsis/septic shock criteria, n (%) | 77 (19.43%) | 59 (64.12%) | <0.001 |
| Temperature in degrees (SD) | 37.15 (1.06) | 36.90 (1.09) | 0.05 |
| HR in bpm (SD) | 93.35 (20.53) | 100.18 (23.93) | 0.014 |
| RR in breaths/min (SD) | 22.81 (8.50) | 26.81 (7.72) | <0.001 |
| Laboratory findings | |||
| Urea>50mg/dl or creatinine > 1.2mg/dl, n (%) | 225 (57.4%) | 70 (76.1%) | 0.001 |
| Serum lactate in mmol/l (SD) | 1.72 (0.89) | 4.58 (2.23) | <0.001 |
| Lactate>2mmol/l, n (%) | 64 (37.2%) | 58 (89.2%) | <0.001 |
| Lactate>4mmol/l, n (%) | 8 (4.7%) | 33 (50.8%) | <0.001 |
| Leucocyte count (SD) per mm3 | 13,450 (8,645) | 19,380 (12,526) | <0.001 |
| Leukocytosis>12,000/mm3or <4000/mm3or >10% band cells | 190 (48.34%) | 63 (70%) | <0.001 |
| CRP in mg/l (SD) | 128.35 (900.14) | 116.54 (140.55) | 0.916 |
| CRP>18mg/l, n (%) | 174 (49%) | 43 (65.2%) | 0.022 |
| PCT in ng/ml (SD) | 4.90 (11.60) | 7.85 (7.01) | 0.010 |
| PCT>0.5 in ng/ml, n (%) | 60 (58.8%) | 21 (87.5%) | 0.008 |
| PCT>1 in ng/ml, n (%) | 48 (47.1%) | 18 (75%) | 0.014 |
| PCT>10 in ng/ml, n (%) | 18 (17.6%) | 7 (29.2%) | 0.161 |
bpm: beats per minute; breaths/min: breaths per minute; CRP: C-reactive protein; ED: emergency department; GCS: Glasgow Coma Scale; HR: heart rate; PCT: procalcitonin; RR: respiratory rate; SBP: systolic blood pressure; SD: standard deviation.
For the statistical analysis, means and their standard deviations (SD) were used for quantitative variables, and percentages for qualitative variables. The chi-square test, Fisher's exact test, Student's t test or Mann–Whitney U test were used, as applicable, to investigate the correlation between mortality and the independent variables (and the dichotomised variables). The groups were stratified beforehand by the centres variable to check homogeneity. A multivariate logistic regression analysis was conducted (the “enter method” was chosen to include all the chosen variables of the model, that is, all those that had statistical significance in the univariate analysis). The comparison results were expressed as p-values and odds ratios (OR) with a 95% confidence interval (95% CI). A p-value <0.05 or when the 95% CI of the OR excluded the value 1 was accepted as significant. The efficacy of the 30-day mortality prediction was assessed by analysing ROC (receiver operating characteristic) curves with a 95% CI of the area under the ROC curve (AUROC), which was compared against the neutral value (0.5). The bootstrap15,16 method on 1000 samples to evaluate their behaviour and reliability was used to perform internal validation of the model. The values of the β coefficients were used to assign the weight of each variable and the model's score. Youden's index was used to determine the cut-off points with the highest diagnostic value that maximised the difference between the true positive rate and the false positive rate, and their sensitivity (SEN) and specificity (SPE) were found. The statistical analysis was performed using IBM-SPSS® Statistics 19 for Windows and STATA 12.0.
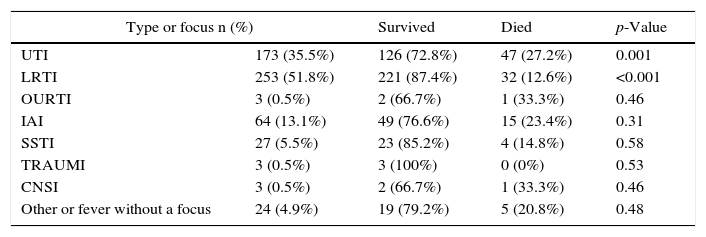
Results488 cases that met the inclusion and follow-up criteria (maintaining the infection diagnosis established by the ED at 30days) were collected by the 8 investigators during the study period. The baseline, functional, comorbidity, clinical-epidemiological and analytical characteristics analysed during the patient's initial assessment in the ED are shown in Table 1. Of these, 92 (18.9%) died within 30days following their consultation in the ED. Table 2 shows case distribution by type of infection in relation to mortality, demonstrating respiratory infections to be the most common (51.8%) and UTIs to cause the highest mortality proportionally. More patients with a UTI than with a respiratory infection were found to have a Barthel index (BI)≤60 and SBP<90mmHg, although both were found to have serum lactate >4mmol/l. These differences were not maintained after the multivariate analysis was adjusted for infection type. The univariate study (Table 1) showed mortality to be directly related to 10 variables: Charlson comorbidity index (CI), Barthel index (BI) (specifically severe functional dependence with a BI≤60), confusion/altered level of consciousness, SBP in mmHg (and SBP<90mmHg), sepsis, severe sepsis/septic shock criteria (and heart rate [HR] and respiratory rate [RR] individually), kidney failure, lactacidaemia in mmol/l (and after dichotomising into >2mmol/l and >4mmol/l), leucocyte count/mm3 (and dichotomised when >12,000 or <4000 or >10% band cells), CRP in mg/l and PCT in ng/ml (and dichotomised into >0.5 and >1ng/ml). However, after performing the multivariate logistic regression analysis, just three maintained statistical significance as predictors of 30-day mortality: severe functional dependence with a BI≤60 (OR 8.92; 95% CI: 4.98–15.98, p=0.003), SBP<90mmHg (OR 7.34; 95% CI: 4.39–12.26, p=0.005) and lactacidaemia >4mmol/l (OR 21.14; 95% CI: 8.94–49.97, p=0.001). The serum lactate cut-off point found to have greatest diagnostic value was 3.84mmol/l (60% sensitivity and 100% specificity), while for the BI it was found to be ≤60points (41% sensitivity and 96% specificity) and for SBP it was found to be <90mmHg (72% sensitivity and 63% specificity).
Types of infection and their correlation to 30-day mortality.
| Type or focus n (%) | Survived | Died | p-Value | |
|---|---|---|---|---|
| UTI | 173 (35.5%) | 126 (72.8%) | 47 (27.2%) | 0.001 |
| LRTI | 253 (51.8%) | 221 (87.4%) | 32 (12.6%) | <0.001 |
| OURTI | 3 (0.5%) | 2 (66.7%) | 1 (33.3%) | 0.46 |
| IAI | 64 (13.1%) | 49 (76.6%) | 15 (23.4%) | 0.31 |
| SSTI | 27 (5.5%) | 23 (85.2%) | 4 (14.8%) | 0.58 |
| TRAUMI | 3 (0.5%) | 3 (100%) | 0 (0%) | 0.53 |
| CNSI | 3 (0.5%) | 2 (66.7%) | 1 (33.3%) | 0.46 |
| Other or fever without a focus | 24 (4.9%) | 19 (79.2%) | 5 (20.8%) | 0.48 |
CNSI: central nervous system infection; IAI: intra-abdominal infection; LRTI: lower respiratory tract infection; OURTI: otolaryngological upper respiratory tract infection; SSTI: skin and soft tissue infection; TRAUMI: traumatic infection: UTI: urinary tract infection.
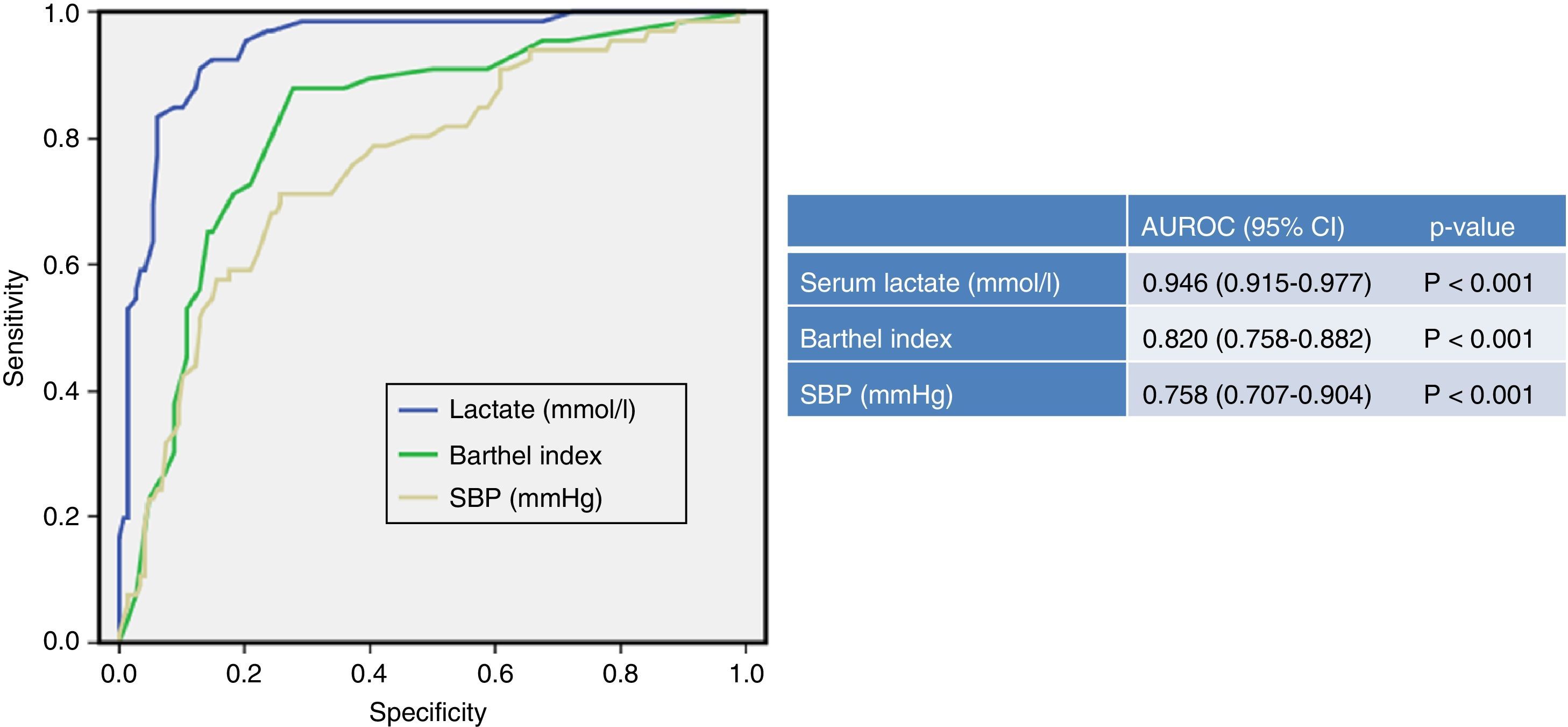
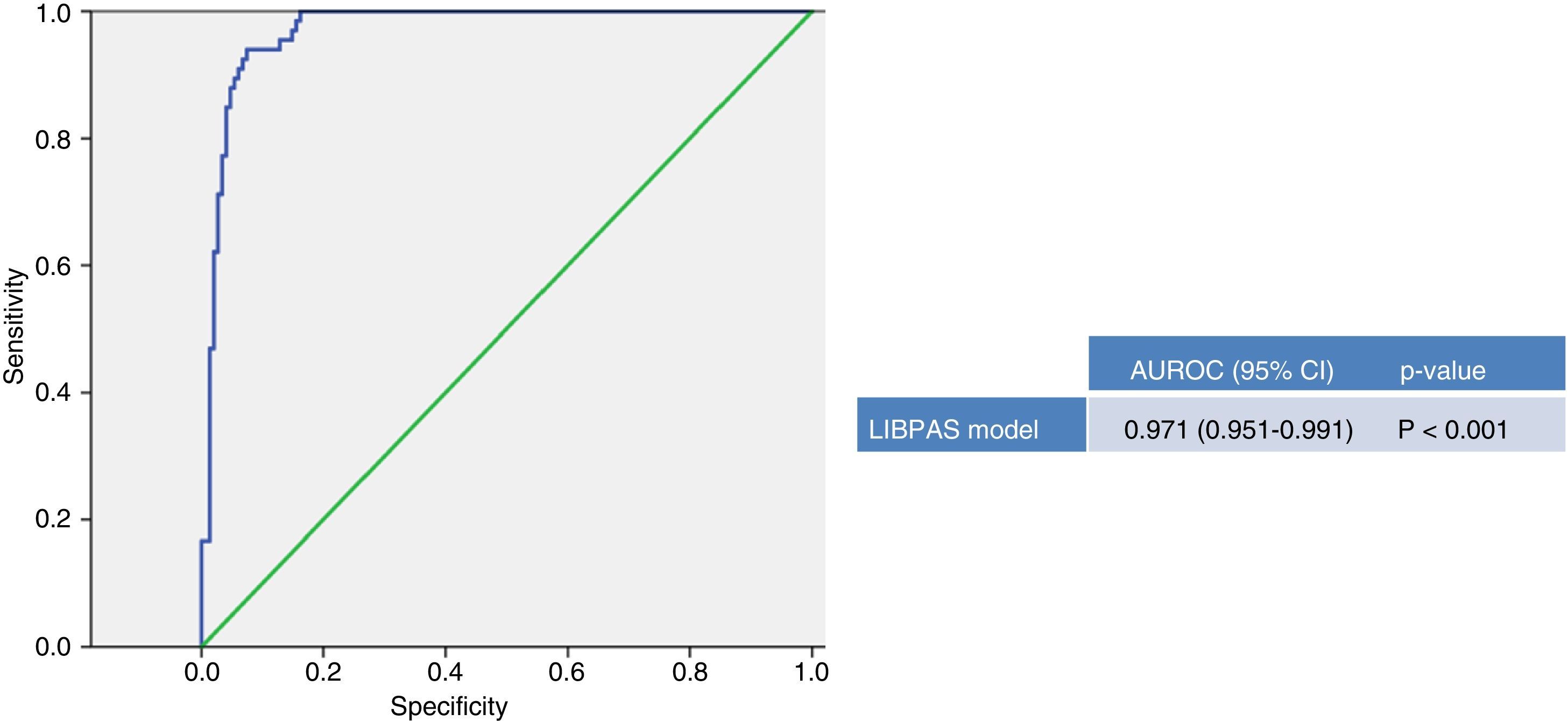
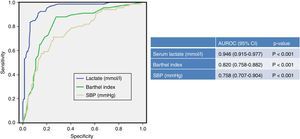
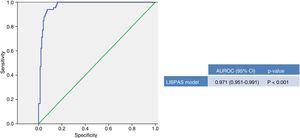
Fig. 1 depicts the area under the ROC curve of the 3 variables that maintained an independent association with 30-day mortality and which achieved the best outcomes (serum lactate, BI and SBP). Fig. 2 shows the ROC curve generated by the model that includes the 3 variables (LIBPAS model: serum Lactate>4mmol/l, Barthel Index ≤60 and SBP<90mmHg), obtaining an area under the ROC curve of 0.971 (95% CI: 0.951–0.991; p<0.001). After correction by the bootstrap method, the model maintained its performance with an area under the ROC curve of 0.910 (95% CI: 0.885–0.935).
Predictive capacity of 30-day mortality in elderly patients in the emergency department. CI: confidence interval; CRP: C-reactive protein; PCT: procalcitonin; p-value: indicates the risk of type 1 error in the null hypothesis test where the area under the ROC curve is 0.5; AUROC: area under the receiver operating characteristic curve; SBP: systolic blood pressure.
Predictive capacity for 30-day mortality of the LIBPAS model. LIBPAS model: Spanish acronym of serum Lactate >4mmol/l, Barthel Index ≤60 and SBP <90mmHg. CI: confidence interval; p-value: indicates the risk of type 1 error in the null hypothesis test where the area under the ROC curve is 0.5; AUROC: area under the receiver operating characteristic curve; SBP: systolic blood pressure.
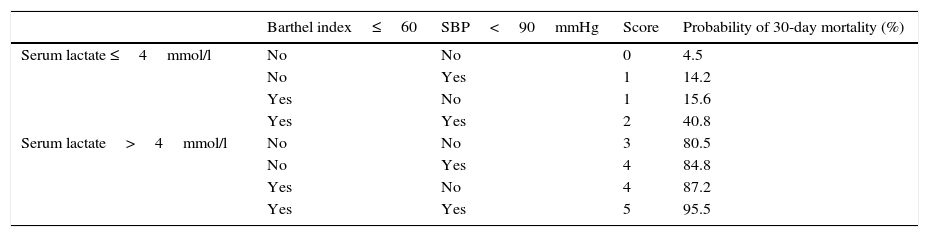
For the LIBPAS model, the weight of each variable was weighed against the individual weight obtained (the results are shown in Table 3). Table 4 presents the probability of elderly patient 30-day mortality in relation to the various LIBPAS model combinations of variables.
Probability of 30-day mortality based on the LIBPAS model.
| Barthel index≤60 | SBP<90mmHg | Score | Probability of 30-day mortality (%) | |
|---|---|---|---|---|
| Serum lactate ≤4mmol/l | No | No | 0 | 4.5 |
| No | Yes | 1 | 14.2 | |
| Yes | No | 1 | 15.6 | |
| Yes | Yes | 2 | 40.8 | |
| Serum lactate>4mmol/l | No | No | 3 | 80.5 |
| No | Yes | 4 | 84.8 | |
| Yes | No | 4 | 87.2 | |
| Yes | Yes | 5 | 95.5 |
LIBPAS model: serum Lactate>4mmol/l, Barthel Index ≤ 60 and SBP<90mmHg.
The results of our study confirm that after the emergency assessment conducted on elderly patients with infection, serum lactate, baseline status (and specifically severe functional dependence with a BI≤60) and SBP<90mmHg are the significantly-correlated independent factors and the strongest prognostic indicators for short-term mortality (30days). These 3 factors that are readily available in the ED make up a new predictive model (LIBPAS), the mandatory use of which should be key in establishing an initial prognosis and in guiding this patient subgroup to the most appropriate resources and healthcare setting.5,6
Serum lactate, which is the best hypoperfusion-tissue hypoxia marker, is included in the emergency department assessment guidelines for patients with sepsis, severe sepsis and septic shock.10 However, it should also be included in the assessment guidelines for elderly patients with or without hypotension, as concentrations >2mmol/l would necessitate close and clinical patient monitoring.9,17 Although few studies have been conducted specifically in elderly patients, Del Portal et al.11 found serum lactate >2mmol/l in the ED to be associated with a relative risk of 30-day mortality of 1.7–2.6, consistent with other studies and reviews where significant differences were also found in adult patients.9 Thus, as in our results, significant differences are obtained with a serum lactate cut-off point >2 or >4mmol/l. In a recently-published study on elderly patients with pneumonia with or without hypotension, Julián-Jiménez et al.18 found serum lactate concentrations >2.5mmol/l to be correlated to 30-day mortality, with an area under the ROC curve of 0.85 (95% CI: 0.78–0.92), in line with our results. In our study, lactacidaemia >4mmol/l gave an OR of 21.1 (95% CI: 8.9–49.9, p=0.002). The optimal cut-off point with a SPE of 100% was 3.84mmol/l, similar to findings in adult patients.9,10,17,18
Severe functional dependence and comorbidity are determining prognosis factors that have become more relevant than ever, and their assessment in EDs is becoming increasingly widespread.6 Specific warning signals comprising serum lactate, baseline and functional status and other specific measures20 are also recommended for elderly patients who are submitted to classic triage or computer-aided simple triage.19 Finally, as already shown, SBP<90mmHg is confirmed as the haemodynamic factor with the highest prognostic value for mortality in elderly patients with infection.10
Although it is known that the appropriateness of hospital admission is higher in elderly patients, with a positive association having been found between appropriateness and age (OR 1.021; 95% CI: 1.008–1.035),21 prognostic assessment in the ED could be objectively and significantly improved through the widespread application of LIBPAS and, due to their weight, assessment of individual serum lactate values, to guide decision-making towards discharge rather than admission and towards the appropriate healthcare setting.
Elderly patients with a LIBPAS model score of 0 points and a serum lactate value of <2mmol/l could be discharged or referred to in-home care or a day hospital. There, patients could be kept under observation for a few hours and receive initial antimicrobial treatment and other therapeutic measures,22 provided that the infection does not require admission or any other urgent procedure.
Elderly patients with a score of 0–1 points and serum lactate concentrations between 2 and 4mmol/l should always be admitted. Although experience with elderly patients in short-stay units in recent years has shown the practice to be a safe and effective alternative to conventional hospitalisation,23,24 decision-making should be based on each patient's baseline status and the resources available.
Elderly patients with a score of 2 points should be admitted to units that provide more intensive clinical monitoring and continuous testing.
Depending on their personal situation, intensive care unit admission should be considered for all patients with ≥3 points or serum lactate >4mmol/l.
Given that this was a multicentre study with patients enrolled by chance, its main limitation is selection bias resulting from the inclusion of patients only when each centre's investigator was on duty, despite the fact that enrolment was consecutive during the recruitment period. Given that the various criteria, definitions and parameters were defined in advance by the INFURG-SEMES scientific committee and were agreed by the investigators, some infection type classification errors may have occurred in the clinical diagnoses. Furthermore, patient characteristics and differences in mortality between different infection types were not analysed as they did not form part of the study objective. As such, some infection types, such as respiratory, were assumed to be heterogeneous and comprised both viral and bacterial infections, which could explain the differences found between them.
The selection of clinical variables could also have been more comprehensive (if it were not for the lack of data) and lab tests were only conducted for those variables available and generally formalised in the emergency department protocols.25 Despite these limitations, we believe that the study is a true reflection of actual clinical practice in our EDs.
In conclusion, the inclusion of serum lactate in the requested lab tests, together with the functional and haemodynamic assessment of all elderly patients with infection in the emergency departments’ initial assessment, have been found to be effective prognostic indicators of short-term mortality. In the future, these measures could significantly improve the prognostic power and comprehensive assessment of patients with sepsis from the moment they arrive at the ED, when used in conjunction with prognostic scores, other biomarkers (such as PCT) or detection systems. The LIBPAS model, which encompasses hyperlactacidaemia >4mmol/l, significant functional dependence and SBP<90mmHg, is a very effective predictor of short-term mortality in elderly patients with infection treated by EDs. Future external validation studies of the model are required.
FundingNo funding was received from any public or private body to complete this manuscript.
Conflicts of interestThe authors declare that they have no conflicts of interest with regards to this article.
Agustín Julián Jiménez (Complejo Hospitalario de Toledo), Juan González del Castillo and Eric Jorge García Lamberechts (Hospital Universitario Clínico San Carlos, Madrid), Mikel Martínez Ortiz de Zárate (Hospital Universitario de Basurto, Bilbao), María Jesús Arranz Nieto (Hospital Nuestra Señora del Prado, Talavera de la Reina), Félix González Martínez (Hospital Virgen de la Luz, Cuenca), Pascual Piñera Salmerón (Hospital Universitario Reina Sofía, Murcia), Carmen Navarro Bustos (Hospital Universitario Virgen de la Macarena, Seville), César Henríquez Camacho (Hospital Universitario Fundación Alcorcón).
Please cite this article as: Julián-Jiménez A, González-del-Castillo J, Martínez-Ortiz-de-Zárate M, Arranz-Nieto MJ, González-Martínez F, Piñera-Salmerón P, et al. Factores pronósticos a corto plazo en los ancianos atendidos en urgencias por infección. Enferm Infecc Microbiol Clin. 2017;35:214–219.