Streptococcus suis (S. suis) infection is poorly described zoonosis in our country, which is related with exposure to pigs or their meat. The most common clinical presentation is meningitis, while spine’s involvement is rare.
MethodsWe report 2 cases of S. suis infection and perform a systematic review of the articles published on S. suis spondylodiscitis between January 1994 and May 2020 with the aim of defining the clinical characteristics, predisposing factors and evolution.
Results17 cases are described, 76.5% males with a mean age of 57.6 years, generally without associated underlying disease. Enolism was a factor present in 17.6%. 70.6% had exposure to pigs or their meat and 20% hand injuries. The mean duration of symptoms was 10.2 days and the most affected segment was the lumbar level. 70.6% had meningitis. All were treated with beta-lactams with an average duration of 53.2 days. There was a recurrence and none died.
ConclusionThere are few cases of S. suis spondylodiscitis in the literature. When occurs, it is associated with another type of infection in most cases. They present a good response to medical treatment and a good prognosis.
La infección por Streptococcus suis (S. suis) es una zoonosis poco descrita en nuestro país, que se relaciona con la exposición al ganado porcino o su carne. La forma de presentación más frecuente es la meningitis, mientras que la afectación de la columna vertebral es rara.
MétodosPresentamos 2 casos de infección por S. suis y realizamos una revisión sistemática de los trabajos publicados sobre espondilodiscitis por S. suis entre el enero de 1994 y mayo de 2020 con el objetivo de definir las características clínicas, sus factores predisponentes y su evolución.
ResultadosSe describen 17 casos, el 76,5% varones con una edad media de 57,6 años, generalmente sin enfermedad de base asociada. El enolismo fue un factor presente en casi el 17.6% de los pacientes. Un 70.6% presentaron exposición a ganado porcino o su carne y un 20% heridas en manos. La duración media de los síntomas fue de 10,2 días y el segmento más afectado fue el lumbar. Un 70.6% cursó con meningitis. Todos se trataron con betalactámicos con una duración media de 53,2 días. Hubo una recidiva y ninguno falleció.
ConclusiónExisten pocos casos de espondilodiscitis porS. suis en la literatura. Cuando ocurre, se asocia a otro tipo de infección en la mayoría de los casos. Presentan buena respuesta al tratamiento médico y buen pronóstico.
Streptococcus suis (S. suis) is a zoonotic agent that is transmitted to human beings mainly by contact with pigs or their meat.1 Most cases described in humans originate in east Asia, where pig breeding and the processing of pig meat is one of the main activities of their economy and also the consumption of raw or partially cooked meat is not uncommon.2 To a lesser extent, cases are also reported in northern European countries, where the disease is almost always work related. The first case in Spain was published in 19943 and since then only 19 more cases have been described.4 Of these, 13 were due to occupational exposure.
While meningitis is the most common clinical manifestation (50–60%), followed by septicaemia, osteoarticular manifestations and, more specifically, spondylitis are rare.5 We are going to study 2 cases and also review all cases of spondylitis caused by S. suis recorded in the literature.
Case reportsCase 137-year-old male with a history of alcoholism who, 5 days prior to admission (January 1999), slaughtered pigs at his home and then developed severe lumbar pain, fever, bilateral hypoacusis and tinnitus. During a physical examination, he had blood pressure of 120/70 mmHg, heart rate of 110 bpm and a temperature of 39.5 °C, stiff neck and hypoacusis as well as selective pain in the region of the lumbar spinous processes. His full blood count results showed a white blood cell count of 6,300, with 80% polymorphonuclear (PMN) leukocytes, and his cerebrospinal fluid (CSF) biochemistry results showed 219 leukocytes (90% PMN), hypoglycorrhachia (glucose 3 mg/dl) and hyperproteinorrhachia (148 mg/dl). S. suis was isolated in blood and CSF cultures (penicillin minimum inhibitory concentration 0.047 mcg/mL). A bone scan showed an abnormal increased uptake at the L5 level suggestive of spondylodiscitis and an audiometry exam confirmed the presence of severe bilateral total deafness, which did not improve over time. The patient received ceftriaxone 4 g/24 h for 14 days and then received intramuscular ceftriaxone 1 g/24 h for a further 14 days.
Case 248-year-old male, butcher by profession with a history of alcoholism and psoriasis who, 9 days prior to admission (August 2001), began to experience severe lower back pain and also a frontal headache, photophobia, nausea and fever for the past 3 days. Prior to these symptoms, the patient reported a wound over his right olecranon after slaughtering a pig at home. The results of his physical examination were as follows: blood pressure 140/80 mmHg, heart rate 62 bpm and temperature 37 °C, impaired consciousness with no meningeal signs and pain on palpating the region of the lumbar spinous processes. His blood test results showed a white blood cell count of 13,330 with neutrophilia (83% PMN) and his CSF biochemistry results showed 352 leukocytes (88% PMN), glucose 30 mg/dl and protein 318 mg/dl. A magnetic resonance scan of the lumbar region showed evidence of spondylodiscitis at the L4-L5 level with an epidural abscess. S. suis biotype II was isolated both in blood and CSF cultures (penicillin minimum inhibitory concentration 0.064 mcg/mL and ceftriaxone minimum inhibitory concentration 0.19 mcg/mL). In view of these findings, ceftriaxone 4 g/24 h was prescribed for 2 weeks, with a dose of 2 g/24 h administered for a further 14 days. The patient had a rapid decrease in body temperature with improved consciousness but subsequently developed hypoacusis and impaired gait, evidence of bilateral cochleovestibular dysfunction. His unsteady gait gradually improved but his hearing loss remained unchanged.
MethodsIn order to identify additional cases of spondylitis caused by S. suis, we searched PubMed for articles published between 1 January 1994 and 31 May 2020. The keywords used for the search were “Streptococcus suis”, “osteoarticular infection”, “osteomyelitis” and "spondylitis". Secondary sources cited in the articles found were also reviewed.
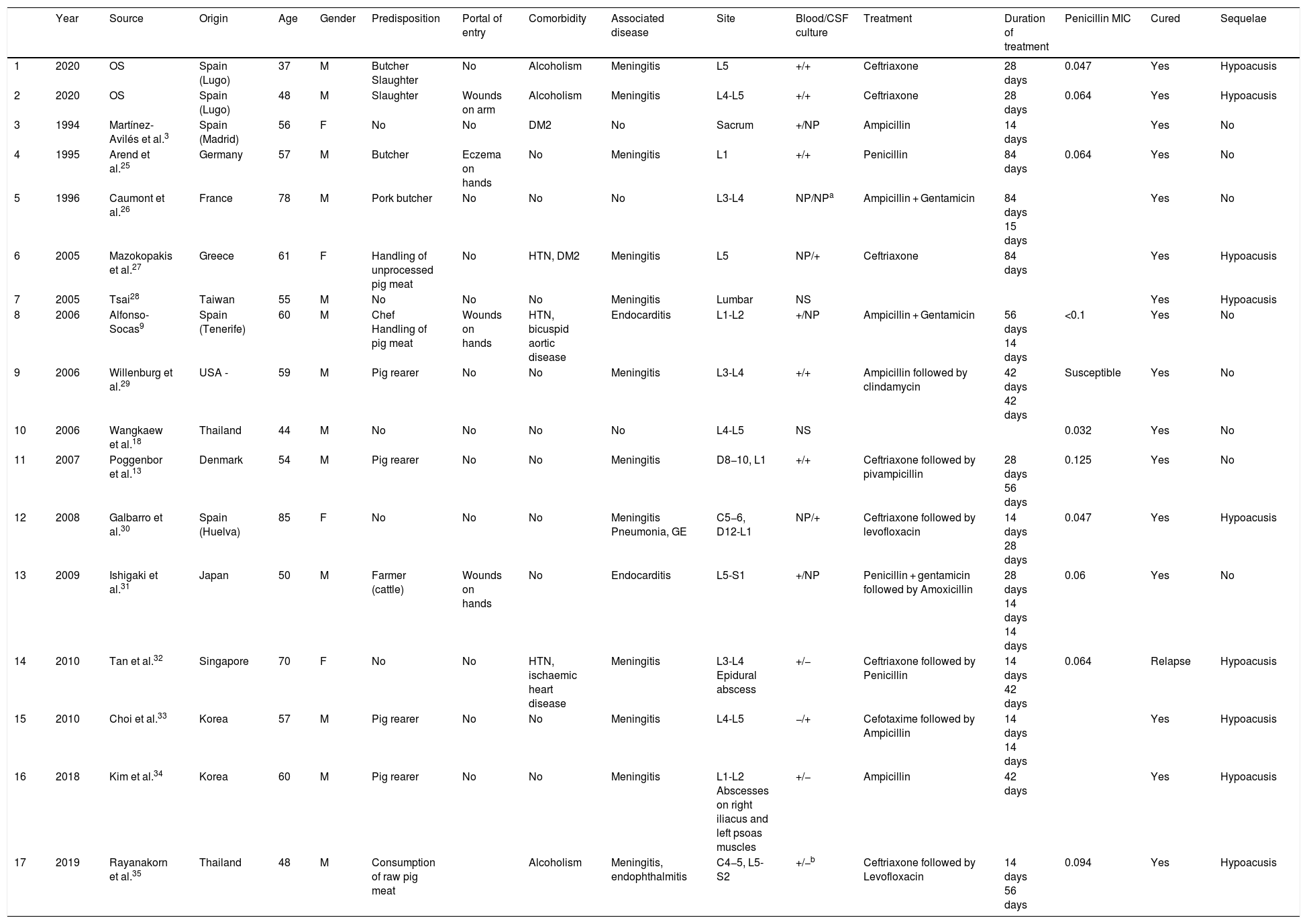
ResultsFollowing a systematic review, we identified 15 cases of spondylitis caused by S. suis, in addition to our 2 cases. The sociodemographic characteristics, predisposing factors and symptoms of these cases, along with microbiological aspects and treatment, are shown in Tables 1 and 2.
Sociodemographic, microbiological and clinical characteristics and treatment of spondylodiscitis caused by S. suis.
| Year | Source | Origin | Age | Gender | Predisposition | Portal of entry | Comorbidity | Associated disease | Site | Blood/CSF culture | Treatment | Duration of treatment | Penicillin MIC | Cured | Sequelae | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2020 | OS | Spain (Lugo) | 37 | M | Butcher Slaughter | No | Alcoholism | Meningitis | L5 | +/+ | Ceftriaxone | 28 days | 0.047 | Yes | Hypoacusis |
| 2 | 2020 | OS | Spain (Lugo) | 48 | M | Slaughter | Wounds on arm | Alcoholism | Meningitis | L4-L5 | +/+ | Ceftriaxone | 28 days | 0.064 | Yes | Hypoacusis |
| 3 | 1994 | Martínez- Avilés et al.3 | Spain (Madrid) | 56 | F | No | No | DM2 | No | Sacrum | +/NP | Ampicillin | 14 days | Yes | No | |
| 4 | 1995 | Arend et al.25 | Germany | 57 | M | Butcher | Eczema on hands | No | Meningitis | L1 | +/+ | Penicillin | 84 days | 0.064 | Yes | No |
| 5 | 1996 | Caumont et al.26 | France | 78 | M | Pork butcher | No | No | No | L3-L4 | NP/NPa | Ampicillin + Gentamicin | 84 days 15 days | Yes | No | |
| 6 | 2005 | Mazokopakis et al.27 | Greece | 61 | F | Handling of unprocessed pig meat | No | HTN, DM2 | Meningitis | L5 | NP/+ | Ceftriaxone | 84 days | Yes | Hypoacusis | |
| 7 | 2005 | Tsai28 | Taiwan | 55 | M | No | No | No | Meningitis | Lumbar | NS | Yes | Hypoacusis | |||
| 8 | 2006 | Alfonso-Socas9 | Spain (Tenerife) | 60 | M | Chef Handling of pig meat | Wounds on hands | HTN, bicuspid aortic disease | Endocarditis | L1-L2 | +/NP | Ampicillin + Gentamicin | 56 days 14 days | <0.1 | Yes | No |
| 9 | 2006 | Willenburg et al.29 | USA - | 59 | M | Pig rearer | No | No | Meningitis | L3-L4 | +/+ | Ampicillin followed by clindamycin | 42 days 42 days | Susceptible | Yes | No |
| 10 | 2006 | Wangkaew et al.18 | Thailand | 44 | M | No | No | No | No | L4-L5 | NS | 0.032 | Yes | No | ||
| 11 | 2007 | Poggenbor et al.13 | Denmark | 54 | M | Pig rearer | No | No | Meningitis | D8−10, L1 | +/+ | Ceftriaxone followed by pivampicillin | 28 days 56 days | 0.125 | Yes | No |
| 12 | 2008 | Galbarro et al.30 | Spain (Huelva) | 85 | F | No | No | No | Meningitis Pneumonia, GE | C5−6, D12-L1 | NP/+ | Ceftriaxone followed by levofloxacin | 14 days 28 days | 0.047 | Yes | Hypoacusis |
| 13 | 2009 | Ishigaki et al.31 | Japan | 50 | M | Farmer (cattle) | Wounds on hands | No | Endocarditis | L5-S1 | +/NP | Penicillin + gentamicin followed by Amoxicillin | 28 days 14 days 14 days | 0.06 | Yes | No |
| 14 | 2010 | Tan et al.32 | Singapore | 70 | F | No | No | HTN, ischaemic heart disease | Meningitis | L3-L4 Epidural abscess | +/− | Ceftriaxone followed by Penicillin | 14 days 42 days | 0.064 | Relapse | Hypoacusis |
| 15 | 2010 | Choi et al.33 | Korea | 57 | M | Pig rearer | No | No | Meningitis | L4-L5 | −/+ | Cefotaxime followed by Ampicillin | 14 days 14 days | Yes | Hypoacusis | |
| 16 | 2018 | Kim et al.34 | Korea | 60 | M | Pig rearer | No | No | Meningitis | L1-L2 Abscesses on right iliacus and left psoas muscles | +/− | Ampicillin | 42 days | Yes | Hypoacusis | |
| 17 | 2019 | Rayanakorn et al.35 | Thailand | 48 | M | Consumption of raw pig meat | Alcoholism | Meningitis, endophthalmitis | C4−5, L5-S2 | +/−b | Ceftriaxone followed by Levofloxacin | 14 days 56 days | 0.094 | Yes | Hypoacusis |
MIC: minimum inhibitory concentration; DM2: type 2 diabetes mellitus; M: male; HTN: hypertension; CSF: cerebrospinal fluid; F: female; NS: not specified; NP: not performed; OS: our study; GE: gastroenteritis.
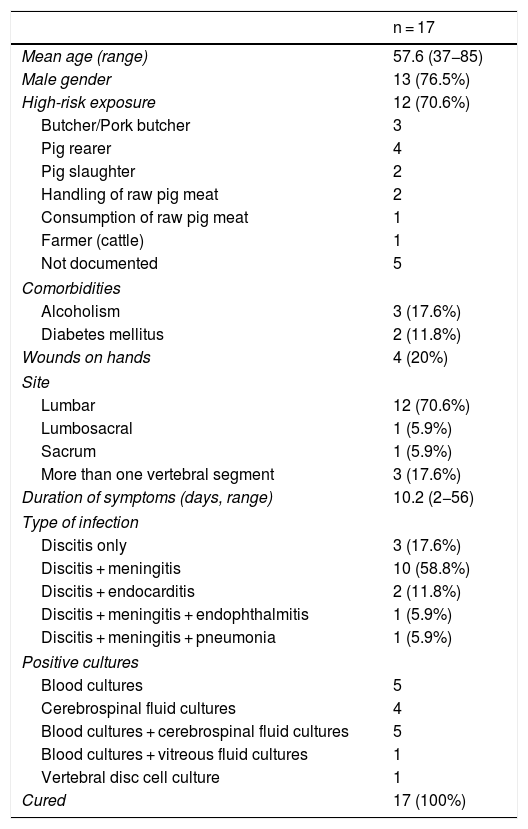
Clinical characteristics of spondylodiscitis caused by S. suis.
| n = 17 | |
|---|---|
| Mean age (range) | 57.6 (37−85) |
| Male gender | 13 (76.5%) |
| High-risk exposure | 12 (70.6%) |
| Butcher/Pork butcher | 3 |
| Pig rearer | 4 |
| Pig slaughter | 2 |
| Handling of raw pig meat | 2 |
| Consumption of raw pig meat | 1 |
| Farmer (cattle) | 1 |
| Not documented | 5 |
| Comorbidities | |
| Alcoholism | 3 (17.6%) |
| Diabetes mellitus | 2 (11.8%) |
| Wounds on hands | 4 (20%) |
| Site | |
| Lumbar | 12 (70.6%) |
| Lumbosacral | 1 (5.9%) |
| Sacrum | 1 (5.9%) |
| More than one vertebral segment | 3 (17.6%) |
| Duration of symptoms (days, range) | 10.2 (2−56) |
| Type of infection | |
| Discitis only | 3 (17.6%) |
| Discitis + meningitis | 10 (58.8%) |
| Discitis + endocarditis | 2 (11.8%) |
| Discitis + meningitis + endophthalmitis | 1 (5.9%) |
| Discitis + meningitis + pneumonia | 1 (5.9%) |
| Positive cultures | |
| Blood cultures | 5 |
| Cerebrospinal fluid cultures | 4 |
| Blood cultures + cerebrospinal fluid cultures | 5 |
| Blood cultures + vitreous fluid cultures | 1 |
| Vertebral disc cell culture | 1 |
| Cured | 17 (100%) |
Of the 17 cases, 9 originated in Europe (5 in Spain), 1 originated in the USA and the others were from Asia. Furthermore, 76.5% were male, with a mean age of 57.6 years. The most common predisposing factor was exposure to pigs or their meat products (70.6%) and hand wounds were reported in 20% of cases.
The mean duration of symptoms was 10.2 days and the vertebral segment most commonly affected was the lumbar region (70.6%), followed by symptoms affecting more than one vertebral segment (17.6%). Two patients experienced complications in the form of abscesses, with one psoas abscess and one epidural abscess. A total of 70.6% of the patients had concomitant meningitis and 11.8% had concomitant endocarditis. These patients with concomitant endocarditis had a clearly longer duration of symptoms than the other patients (44 vs. 6.8 days, respectively).
Diagnostic microbiology was used to reach a diagnosis based on blood and/or CSF cultures in 15 cases (88.2%). Only one patient was diagnosed by vertebral biopsy culture. One case did not specify how diagnostic microbiology was used.
In 15 patients for whom the treatment used was specified, beta-lactams were the treatment of choice, with ceftriaxone being the most commonly used in a total of 8 cases. Gentamicin was used in 3 cases and IV-to-oral switch therapy was used in 4 cases (switching to levofloxacin in 2 cases, to amoxicillin in 1 case and to clindamycin in 1 case). The mean duration of therapy was 53.2 days (range: 14–84 days). Surgical drainage was required in 2 patients but, despite this, one patient experienced a relapse. All patients were cured and 9 of the 12 patients with meningitis experienced hypoacusis as a sequela.
DiscussionS. suis is an emerging zoonotic pathogen that generally causes sporadic infections, although infection outbreaks have been described in recent decades. While most cases originate in Asia, Europe accounts for 8.5% of all cases reported worldwide, with the Netherlands, the United Kingdom and France having the highest incidence rates.6 In our country, it is an uncommon disease that is associated primarily with exposure to pigs or the processing of their meat products.7 At our hospital, 4 cases of S. suis infection have been seen in recent decades, 2 with spondylodiscitis, one with meningitis and another with bacteraemia. With these, a total of 24 cases have been reported in Spain. The distribution of cases is not uniform across Spain, with 7 (29%)8–10 originating in Galicia, a community with 2.7 million inhabitants, although it must be noted that our cases were reported over a period of 22 years. Surprisingly, in Catalonia, which has a larger population (7.2 million inhabitants) and a higher pork production,11 only one case has been reported.12 Perhaps the way in which the meat is processed and consumed may explain this geographical variation in incidence. Some years ago, some areas of our country, including Galicia, slaughtered pigs in a non-industrial setting relatively frequently. Protection and hygiene measures were therefore not as strict and those involved came into closer contact with the animals. Of the 20 patients reported in the Spanish literature, only one kept pigs for personal consumption and none of the cases were associated with home-based slaughtering. In contrast, 3 of the 4 cases assessed at our hospital were the result of this practice.
S. suis infection occasionally results in osteoarticular manifestations, the most common being arthritis. This generally affects large joints and sometimes affects multiple joints. Symptoms affecting the axial skeleton are less common with very few cases reported in the literature.13 In one meta-analysis published in 2014, an incidence of 3.7% was reported for spondylitis.5 In a more recent study conducted in northern Thailand,14 the incidence rate was higher (9%). In one of the Spanish cohorts with the highest number of cases of osteoarticular infection, 17% were caused by streptococci and no cases caused by S. suis were reported.15 Curiously, 5 of the 17 cases of spondylitis reported in the international literature originate in our country.
As observed with other infections caused by S. suis, spondylitis occurs primarily in middle-aged men. This may be explained by the fact that this microorganism is closely related to exposure to pigs, very often among professions in which most employees are men. Nevertheless, the age of onset is slightly higher than that of other manifestations, such as meningitis.16 This is probably due to the presence of more underlying bone diseases at higher ages, resulting in a higher risk of bone infection.
Most of these patients are healthy with no comorbidities.17 Of those comorbidities described, the most common is chronic alcoholism, affecting nearly 50% in some jobs14 and present in 3 of the cases studied. The second most common associated disease is diabetes, which is present in 8–19.5% of patients in the different studies5,14 and in 11% of the patients in our study.
With regards to the route of infection, the portal of entry for the pathogen may be cutaneous since around 20% of patients have wounds at the time of admission, which is similar to the percentage described for all infections caused by S. suis.16
The signs and symptoms of discitis caused by S. suis do not appear to be different from those described for other microorganisms. Nevertheless, its frequent association with meningitis (12 of the 17 cases) is notable as this is not observed in cases of discitis caused by other streptococci. Only 3 of the 17 cases of spondylitis reviewed were not associated with another type of infection.
Although in some countries, such as Thailand,18S. suis is one of the main causes of streptococcal endocarditis, worldwide it is an uncommon manifestation.17 In our study only 2 cases were associated with endocarditis, accounting for 11.8%. This is different from the situation described with other streptococci, such as S. bovis or S. viridans,19,20 where this association can reach 50%.
S. suis is easily isolated in blood or CSF, although it is often identified incorrectly as S. bovis, S. viridans or enterococcus with those commercial methods normally used. Nevertheless, mass spectrometry (MALDI-TOF MS) has improved diagnostic reliability and speed over recent years.21S. suis is generally highly susceptible to penicillin, with very few exceptions in human infections, although not in porcine infections.
With regards to treatment, all patients received beta-lactams with a mean duration of treatment of 2 months. Our 2 cases received beta-lactams for 28 days, with a good outcome. These shorter dosage regimens currently appear to be as effective as longer regimens in most cases of spondylitis.22
No patients developed significant osteoarticular sequelae, while auditory sequelae secondary to meningitis are frequently observed, with a similar incidence to that described in the literature (75%). Although somewhat controversial, it seems that steroids may prevent this sequela.16
Mortality in infections caused by this microorganism is generally low (3–11%),23 even in those cases associated with meningitis. Mortality rates only rise considerably in those cases associated with streptococcal toxic shock syndrome, such as those described during the outbreak in China,24
In conclusion, spondylitis caused by S. suis is rare and in most cases is associated with another type of infection. Such infections include predominantly meningitis, followed by rare cases of endocarditis. Despite this, prognosis is good.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Romay-Lema E-M, Ventura-Valcárcel P, Iñiguez-Vázquez I, García-Pais MJ, Garcia-Garrote F, Rabuñal-Rey R, et al. Espondilodiscitis por Streptococcus suis: 2 nuevos casos y revisión bibliográfica. Enferm Infecc Microbiol Clin. 2022;40:66–70.