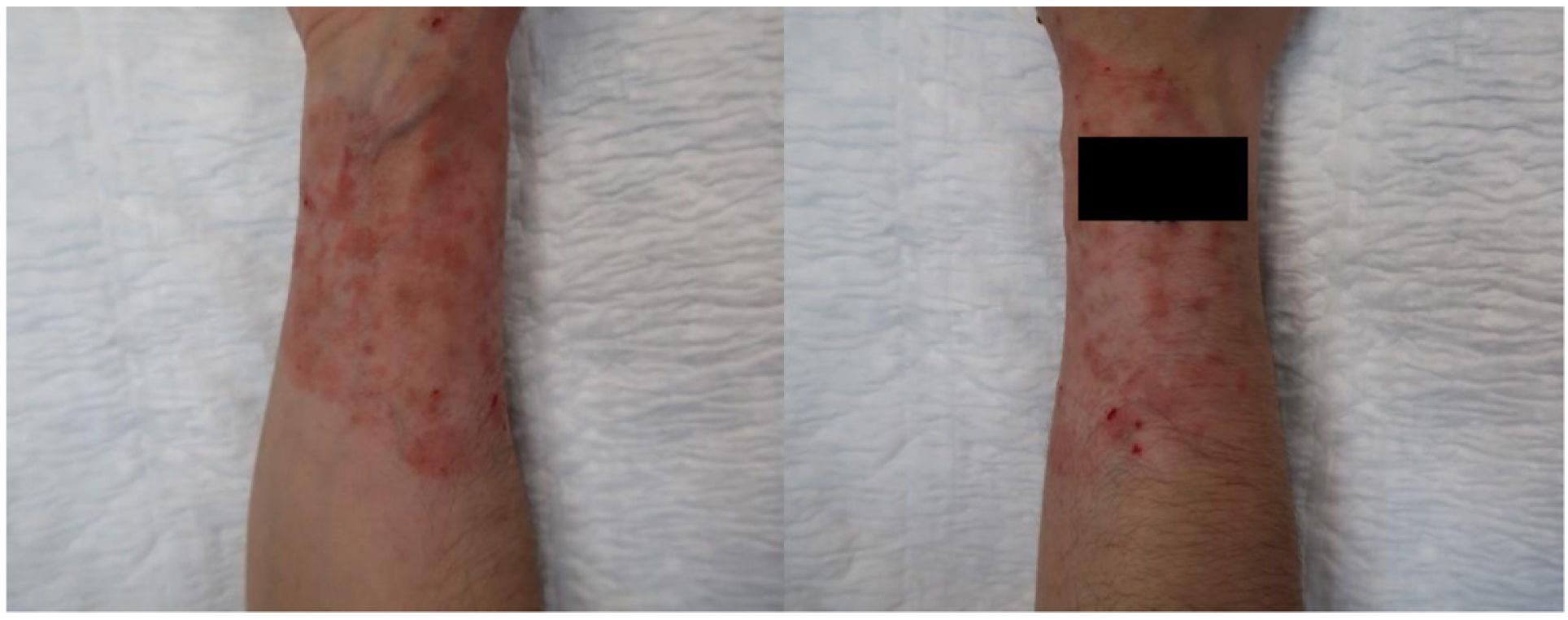
This was a 32-year-old woman with a 10-year history of ulcerative colitis treated with infliximab and mesalazine. She lived on a farm with horses, although she had no direct contact with them. The patient was referred to the Dermatology clinic with a very itchy erythematous, scaly plaque with scattered macules and papules inside on her right forearm, which had been growing along the edge, with a circular or ring-like appearance, for a year (Fig. 1). Previously, she had been treated with high-potency topical corticosteroids for 6 months, with the lesion becoming worse. Skin scales were taken for mycology culture and treatment was started with oral terbinafine 250 mg/ h and topical flutrimazole 1% every 12 h for 2 months.
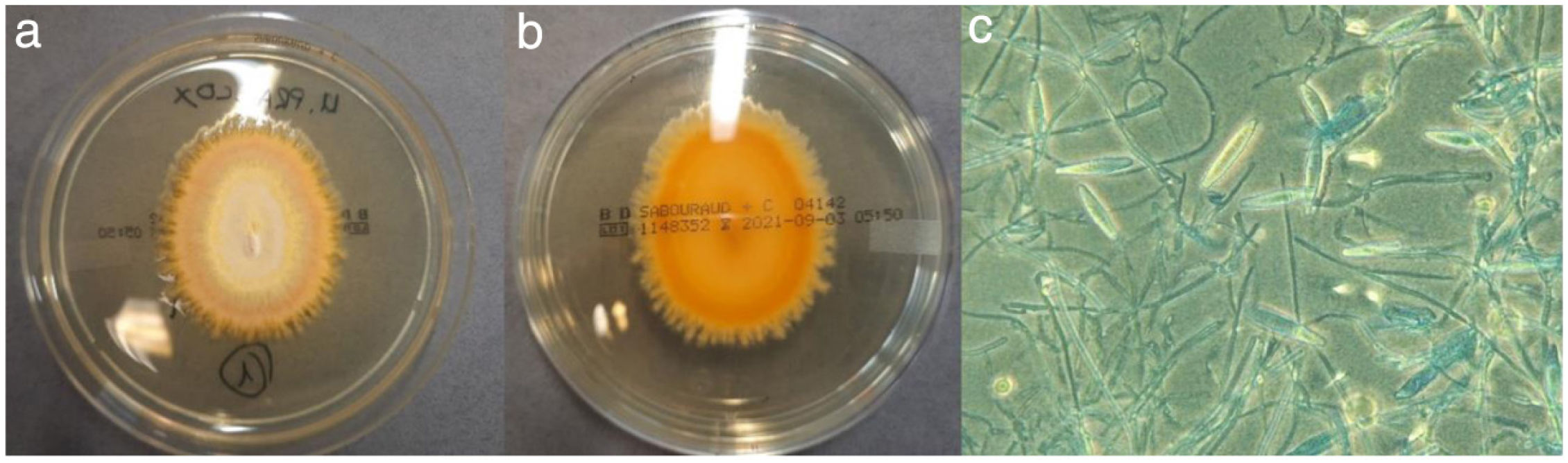
Skin flakes were cultured on Sabouraud-chloramphenicol agar (Becton–Dickinson, Tullastrasse, Germany) and Sabouraud-cycloheximide agar (Becton–Dickinson, Tullastrasse, Germany) and incubated at 30°C aerobically. After 6 days of incubation, the growth of two colonies of a filamentous fungus with a flat, powdery, yellowish front and a smooth, bright yellow back was observed on the Sabouraud-cycloheximide agar plate (Fig. 2a and b). Microscopic examination using lactophenol blue staining revealed pyridiform microconidia arranged along the hyphae and lanceolate, rough, septate (6–9 septa) thin-walled macroconidia emerging from the central or final part of the hyphae (Fig. 2c), characteristics with which it was identified as Nanizzia praecox, based on De Hoog et al.1 Identification was corroborated by MALDI/TOF mass spectrometry (Bruker®, Billerica, United States) after protein extraction in a liquid medium described by Cassagne et al.2 with a score of 2.21 for N. praecox.
Clinical courseAfter an initial worsening, the lesion slowly improved. At 13 days, the patient still had considerable itching and erythema. At 2 months, the lesion was virtually resolved (Fig. 3), but the itching and some erythema persisted, so it was decided to continue treatment with oral itraconazole 50 mg/24 h for 14 days and topical flutrimazole until full resolution.
CommentsN. praecox is a dermatophyte belonging to the Arthrodermataceae family, classified until 2017 in the genus Microsporum (M. praecox). It is a geophilic and zoophilic fungus closely associated with equine environments, which rarely causes infection in humans.3,4 To date, fewer than 40 cases have been described in the literature. Uhrlaß et al.5 reported three cases of tinea corporis caused by N. praecox in five years, in which two of the patients had had direct contact with horses. Alanio et al.6 reported another case of a female horse rider with tinea corporis in which the aetiological agent was M. praecox. In the case we describe here, our patient did not have direct contact with horses, but she did live in an equine environment, so indirect transmission through the soil and contaminated materials seems the most likely route of infection, as the characteristic geophilic properties of this dermatophyte enable it to remain in the environment without the need for an animal reservoir.4 The main limitation of this work is not having had a PCR technique to confirm the identification. However, the study by Hamal et al.7 included 196 filamentous fungi, including dermatophytes, where identification by MALDI/TOF associated with a previous extraction of proteins in a liquid medium had a correlation rate at the species level close to 90% with sequencing results. The results obtained by Hamal et al.7 in conjunction with the case we describe here, show that using two complementary techniques affordable for most laboratories, like mass spectrometry and macro/microscopic identification, results are comparable to those obtained with more complex molecular techniques, which are less accessible to most Microbiology services. In terms of treatment, topical antifungals are usually sufficient in demarcated non-inflammatory lesions; in more severe cases, combining with a systemic antifungal (terbinafine, griseofulvin or azoles) is usually necessary.4 The lesion usually resolves within a month with appropriate treatment.5,6 In this case, the resolution was slower (>2 months) probably because the patient was receiving long-term immunosuppressive therapy for the treatment of her disease. To sum up, N. praecox is a pathogen to be considered in patients with lesions compatible with tinea corporis and/or tinea capitis and who live in environments with direct or indirect contact with horses.