Tuberculosis (TB) continues to be a serious public health problem and establishing a definitive diagnosis among children is extremely challenging. Pulmonary tuberculosis is the most prevalent form, with children under the age of 2 years being at greatest risk of severe and disseminated forms. The aim of this study was to describe TB among children in Spain in recent years.
Patients and methodsA retrospective study of paediatric patients diagnosed with TB in two hospitals of the Community of Madrid over a 26-year period (1991-2017). Epidemiological and clinical variables, additional tests and treatments received were analysed.
Results170 children were included. The two most-affected age groups were infancy and adolescence. 42.9% of patients were immigrant children (South-America or Morocco). The main reasons for consultation were TB contact (20.6%) and fever (15.3%). At diagnosis, 61.8% of cases referred an epidemic environment, and 30.6% were asymptomatic. The Mantoux tuberculin skin test was positive in 92.2% of patients and IGRA was positive in 70.6%. Pulmonary TB was identified in 91.8% of children vs. 8.2% with extrapulmonary forms. Gastric juice culture was positive in 36.9% of cases and three strains resistant to isoniazid were isolated. All patients were cured without complications except one who died.
ConclusionsPulmonary TB continues to be the most prevalent form among children and presumptive diagnosis (symptoms consistent with positive Mantoux test or suggestive X-ray) is the most common form of diagnosis. It is important to conduct a contact investigation in order to control the spread of TB.
La tuberculosis (TB) continúa siendo un problema de salud pública grave. En la edad pediátrica existe gran dificultad para obtener un diagnóstico de certeza. La principal forma de presentación es la pulmonar, con mayor riesgo de formas graves y extrapulmonares en menores de 2 años. El objetivo del estudio es describir la TB en población pediátrica en nuestro medio en los últimos años.
Pacientes y métodosEstudio retrospectivo de TB diagnosticadas en 2 hospitales de la Comunidad de Madrid durante 26 años (1991-2017). Se analizan variables epidemiológicas, clínicas, pruebas complementarias y tratamientos recibidos.
ResultadosSe incluyeron 170 niños. Las 2 franjas de edad más afectadas son la lactancia y la adolescencia. Población inmigrante: 42,9% (Sudamérica y Marruecos). Los principales motivos de consulta fueron contacto con TB (20,6%) y fiebre (15,3%). Al diagnóstico, el 61,8% refería ambiente epidémico. El 30,6% estaba asintomático. El Mantoux fue positivo en el 92,2% de los pacientes y el IGRA fue positivo en el 70,6% de casos realizados. Se halló enfermedad pulmonar en el 91,8% vs. afectación extrapulmonar en el 8,2% de los niños. El cultivo fue positivo en el 36,9% de muestras de jugo gástrico y se aislaron 3 cepas resistentes a isoniacida. Todos los pacientes seguidos curaron sin secuela, salvo uno que falleció.
ConclusionesLa afectación pulmonar continúa siendo la forma de presentación más frecuente de TB en pediatría. El diagnóstico de presunción (clínica compatible con Mantoux positivo o radiografía patológica) es el más habitual. Es importante realizar estudio de contactos como medida de control de enfermedad tuberculosa.
Tuberculosis (TB) is one of the infectious diseases with the greatest impact worldwide. It is one of the leading causes of death of infectious origin, ahead of HIV and malaria.1 In the European Union, a decrease was observed in the incidence rate of TB between 2012 and 2017. In 2017, the estimated incidence rate stood at 11.9 cases/100,000 and 4.4% of all the cases diagnosed were under the age of 15.2 In that same year (2017) in Spain, the overall incidence rate was 9.43 cases/100,000 (4390 cases), below the European average.3 Despite the reduction, TB continues to be a significant public health problem.
HIV infection is the most important cofactor for the development of disease in people infected by Mycobacterium tuberculosis. There are other risk factors that contribute significantly to the development of the disease, such as age, immigration or the use of immunomodulatory therapies.
In childhood, the infection is very often asymptomatic, except for infants and adolescents, who are more likely to show symptoms, with lung disease being the most common form of presentation. Children under two years of age have a greater likelihood of progressing to severe and extrapulmonary forms of TB.4–7
Infected children are the reservoir from which new cases of disease will occur in the future. Appropriate management of exposure to active TB and latent infection in children helps prevent the development of more severe forms.8 Furthermore, any infected child represents a sentinel event of recent transmission of M. tuberculosis in the community, the source of contagion generally being a close family member with active TB. Therefore, setting up close surveillance of family units, ensuring the study and treatment of contacts of the sentinel case, helps break the chain of infection.
The biggest challenge in childhood TB is the difficulty in obtaining a definite diagnosis.9 There are new diagnostic techniques such as the Interferon Gamma Release Assay (IGRA),10 which are very useful in children vaccinated with BCG, as a positive result confirms infection by M. tuberculosis, and techniques for DNA amplification (polymerase chain reaction [PCR]),11 which provide a faster diagnosis.
In Spain, there is little information on childhood TB, with few reported series on paediatric patients. The aim of the study was to describe the epidemiological and clinical characteristics of TB in the paediatric population of two hospitals in the Autonomous Region of Madrid over the last 26 years.
Patients and methodsThis was a descriptive, observational, retrospective study which included all cases of patients from 0 to 17 years of age diagnosed with tuberculosis from June 1991 to December 2017 at Hospital Clínico San Carlos and Hospital Getafe.
We collected epidemiological variables: age, gender, place of birth and origin of the parents; epidemiological environment and contact with TB. We described clinical characteristics (symptoms at diagnosis, existence of BCG scar) and analytical and microbiological characteristics at diagnosis. We also recorded treatment received and the clinical outcome (follow-up time, complications).
The presence of clinical symptoms and/or radiological abnormalities compatible with TB with at least one of the following criteria was considered a diagnosis of infection with TB: history compatible with TB (contact with TB) or positive Mantoux test or compatible microbial isolates. Cases of TB affecting the lung parenchyma or the tracheobronchial tree were considered to be pulmonary TB, and the remaining cases were considered as extrapulmonary.
The Mantoux test was considered positive when the induration (48/72h after inoculation and measured as the transverse diameter) was larger than 10mm or larger than 5mm combined with a high degree of clinical suspicion or the patient being immunosuppressed.9 Where available, we collected the results of IGRA techniques (QuantiFERON-TB).
The chest X-ray or chest CT scan was described as abnormal if there was evidence of infiltrates, lymphadenopathy, atelectasis or mediastinal enlargement compatible with TB.
All children of foreign parents were considered to be of immigrant origin. Of these patients, we also recorded whether they were born in Spain or outside Spain and the country of origin of the parents.
Fasting gastric juice and induced sputum samples (performed since 2007) were collected on three consecutive days. AFB staining, culture for mycobacteria and genomic amplification technique (PCR) were performed simultaneously on the samples collected.
The study was approved before starting by the Ethics Committee of both hospitals. No personal information was collected in the study. Each patient received an anonymous numerical code, with this being the only data that identified them and it was not therefore necessary to request the patients’ informed consent for this study.
For the statistical analysis, we used the SPSS 20 system for Windows. Continuous variables were expressed as median and interquartile range (IQR) and categorical variables as distribution of frequencies or percentages.
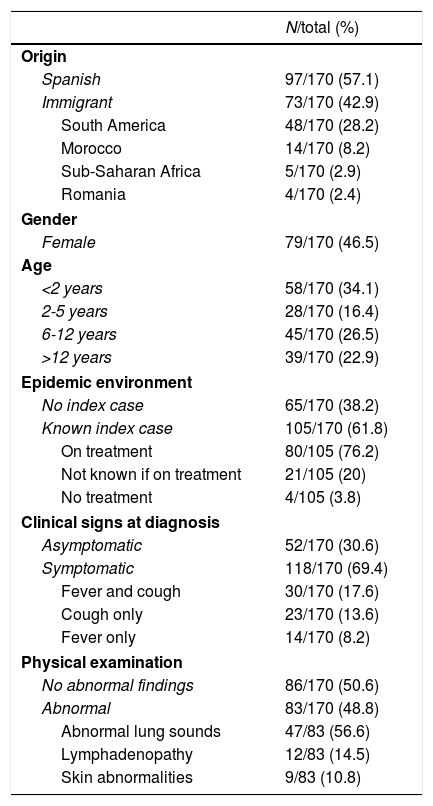
ResultsA total of 170 patients were diagnosed with TB; 91 were male (53.5%). The median age at diagnosis was 4.5 years (IQR 2-11). The epidemiological and clinical characteristics of the patients are shown in Table 1.
Epidemiological and clinical characteristics of patients with tuberculosis.
| N/total (%) | |
|---|---|
| Origin | |
| Spanish | 97/170 (57.1) |
| Immigrant | 73/170 (42.9) |
| South America | 48/170 (28.2) |
| Morocco | 14/170 (8.2) |
| Sub-Saharan Africa | 5/170 (2.9) |
| Romania | 4/170 (2.4) |
| Gender | |
| Female | 79/170 (46.5) |
| Age | |
| <2 years | 58/170 (34.1) |
| 2-5 years | 28/170 (16.4) |
| 6-12 years | 45/170 (26.5) |
| >12 years | 39/170 (22.9) |
| Epidemic environment | |
| No index case | 65/170 (38.2) |
| Known index case | 105/170 (61.8) |
| On treatment | 80/105 (76.2) |
| Not known if on treatment | 21/105 (20) |
| No treatment | 4/105 (3.8) |
| Clinical signs at diagnosis | |
| Asymptomatic | 52/170 (30.6) |
| Symptomatic | 118/170 (69.4) |
| Fever and cough | 30/170 (17.6) |
| Cough only | 23/170 (13.6) |
| Fever only | 14/170 (8.2) |
| Physical examination | |
| No abnormal findings | 86/170 (50.6) |
| Abnormal | 83/170 (48.8) |
| Abnormal lung sounds | 47/83 (56.6) |
| Lymphadenopathy | 12/83 (14.5) |
| Skin abnormalities | 9/83 (10.8) |
BCG scars were found in 14.3% of patients (23/161). No primary or acquired immunodeficiency was identified in our patients, and there were no cases with pharmacological suppression.
The main reason for consultation was contact with active TB (20.6%), followed by fever (15.3%) and respiratory symptoms (14.1%); four cases (2.4%) consulted due to limping and another four (2.4%) had erythema nodosum.
In terms of the epidemic environment, described in Table 1, it is worth highlighting that of the 105 index cases, 80/105 (76.2%) maintained close contact with the child (same household), while 25/105 (23.8%) had only partial contact (family members or teachers).
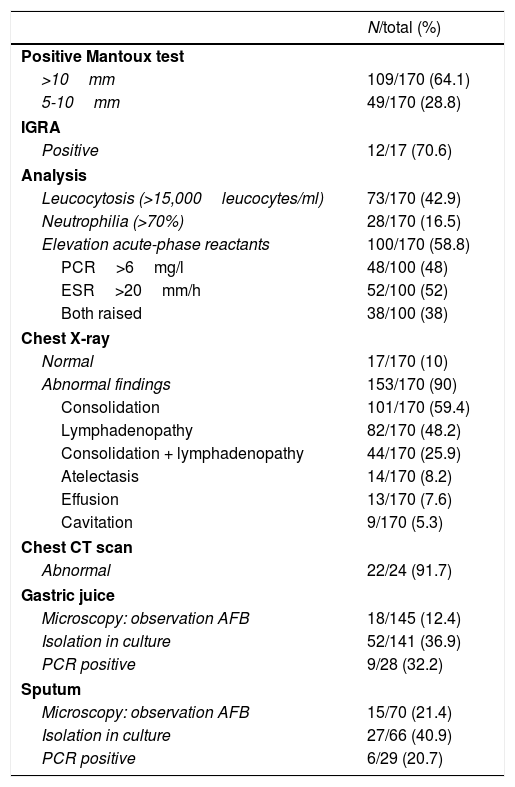
The investigations carried out are shown in Table 2. A positive Mantoux skin test was found in 92.9% of the children (158/170). In 12/170 cases (7.1%) the Mantoux test was <5mm (one was diagnosed with chicken pox the week prior to the study, another had a miliary TB pattern, four had a compatible chest CT scan; infection was confirmed in three cases by positive IGRA; and in the rest, positive results were obtained in microbiological tests).
Complementary tests.
| N/total (%) | |
|---|---|
| Positive Mantoux test | |
| >10mm | 109/170 (64.1) |
| 5-10mm | 49/170 (28.8) |
| IGRA | |
| Positive | 12/17 (70.6) |
| Analysis | |
| Leucocytosis (>15,000leucocytes/ml) | 73/170 (42.9) |
| Neutrophilia (>70%) | 28/170 (16.5) |
| Elevation acute-phase reactants | 100/170 (58.8) |
| PCR>6mg/l | 48/100 (48) |
| ESR>20mm/h | 52/100 (52) |
| Both raised | 38/100 (38) |
| Chest X-ray | |
| Normal | 17/170 (10) |
| Abnormal findings | 153/170 (90) |
| Consolidation | 101/170 (59.4) |
| Lymphadenopathy | 82/170 (48.2) |
| Consolidation + lymphadenopathy | 44/170 (25.9) |
| Atelectasis | 14/170 (8.2) |
| Effusion | 13/170 (7.6) |
| Cavitation | 9/170 (5.3) |
| Chest CT scan | |
| Abnormal | 22/24 (91.7) |
| Gastric juice | |
| Microscopy: observation AFB | 18/145 (12.4) |
| Isolation in culture | 52/141 (36.9) |
| PCR positive | 9/28 (32.2) |
| Sputum | |
| Microscopy: observation AFB | 15/70 (21.4) |
| Isolation in culture | 27/66 (40.9) |
| PCR positive | 6/29 (20.7) |
Of the 170 cases, 156 (91.2%) were diagnosed with pulmonary TB; 153 (90.0%) had abnormal X-rays but diagnosis had to be confirmed by chest CT scan in the other three.
The other 14 of the total 170 cases were extrapulmonary TB (8.2%): 5/14 (35.7%) in the form of lymphadenitis; 5/14 (35.7%) with cutaneous forms; 2/14 (14.3%) were joint involvement; and 2/14 (14.3%) were tuberculous meningitis.
In the microbiological tests (Table 2), it is worth noting M. tuberculosis was isolated in gastric juice in 36.9% and sputum in 40.9%.
In terms of treatment, the recommended regimen for TB with a sensitive strain in children was used in 70.6% (120/170): isoniazid and rifampicin for six months combined with pyrazinamide for the first two months. Resistance to isoniazid was identified in 3/170 patients (1.8%), but there were no cases of multi-drug resistant TB; 27/170 patients (15.9%) received treatment with combined-drug preparations. Directly observed therapy was documented in 5/170 (2.9%) and 7/170 (4.1%) patients received adjuvant corticosteroid therapy. The documented adverse effects (18/170 patients [10.5%]) were: hypertransaminasaemia, vomiting, abdominal pain/diarrhoea, hyperuricaemia and rash (interpreted as related to pyrazinamide). Withdrawal of the drug or dose adjustment was necessary in 9/170 cases (5.2%).
Follow-up was performed in 86.5% (147/170) of the patients (at hospital or outpatient clinics) and continued for >6 months in 124/147 patients (84.4%). Correct adherence to treatment was confirmed in 75.9% of patients. All of the patients had a good prognosis, with no subsequent sequelae documented, except for one patient who died at the age of two months after being diagnosed with pulmonary TB with secondary haemophagocytic syndrome.12
DiscussionTB continues to be a common health problem in our area. As shown in the results, there was no clear predominance of gender overall. In our series, in line with published articles, lactation and adolescence were the most affected periods in terms of age.13,14
The epidemiology is changing and in most western countries over the last few years, childhood TB has affected immigrants from highly endemic areas14,15, with the native population only sporadically suffering from microepidemics. In our study, 76 children were immigrants or children of immigrants, mainly from South America or Morocco, countries from which Spain receives the most immigration. Only half of the patients belonged to the native population.
The main reason for consultation, reported in two thirds of the patients, was exposure to an index case of TB. It is important that this be borne in mind, since, apart from the early diagnosis and treatment of patients, the best strategy for controlling tuberculosis is to conduct an exhaustive study of exposed contacts,16,17 as paediatric patients are sentinel events of TB in the community. Of the index cases, 76.2% had been or were being treated correctly. However, almost 24% did not receive anti-tuberculosis treatment, with these cases being missed opportunities to break the chain of infection and eradicate the disease.
The lack of symptoms and their non-specificity can make diagnosis difficult. In our series, a third of the children were asymptomatic and among the symptomatic, the majority had nonspecific manifestations such as a cough and fever. The main form of skin involvement described in the series was erythema nodosum, which is a typical form of presentation in childhood.18
The majority of the 170 patients suffered from the pulmonary form of the disease, this being the most common clinical onset in childhood.4–7 However, there is a higher risk of extrapulmonary disease in the paediatric population, with the rate of tuberculous meningitis in children under five years of age being much higher than the average in the adult population.19 Our series had a not insignificant number of cases with extrapulmonary symptoms (8.2%) such as cervical lymphadenitis, hip arthritis, skin involvement and central nervous system involvement.
The tuberculin test is the most useful method for diagnosing TB infection and is very helpful in detecting the disease in both children and adolescents.9 In our series, over 90% of the children had a positive Mantoux test, with induration >10mm in 64.1% of cases. In the last few years of the period covered by the study, where necessary, tests were completed with IGRA (similar sensitivity [>80%] to the Mantoux test but greater specificity),9 which was positive in almost three quarters of patients, reflecting its utility in cases where infection and disease are uncertain (BCG vaccinated).
The chest X-ray is also still very important as a diagnostic tool. A chest CT scan was only necessary in patients with compatible symptoms, positive Mantoux test or close contact with TB and inconclusive/suspect X-ray, as described in the guidelines,9,20 and, of the 24 patients in whom it was performed, it was found to be abnormal in 22. The radiological manifestations of TB in children are highly variable.21 In our series, the most common abnormality was simple parenchymal involvement followed by lymph node involvement (right predominance). Other abnormalities described were unilateral pleural effusion (in pre-pubertal patients, with symptoms of chest pain), and a smaller number of patients with cavitation (all over 11 years of age, except one 7-year-old, at diagnosis).
All patients with suspected TB should have a microbiological study with the aim of arriving at a definitive diagnosis. Of the three microbiological techniques described in our series, culture continues to be the most cost-effective, although PCR does provide benefits in clinical practice, such as speed of results and the ability to report the strain and sensitivity to anti-TB drugs.
The treatment used was as recommended in the paediatric TB guidelines22,23: HRZ(E)2m+HR4m, with variations over the period covered by the study; initially three drugs were used [HRZ], but later, due to the increased resistance to isoniazid in our area, the therapy regimen was modified, with four drugs until confirmation of strain sensitivity. Only three cases of resistance to isoniazid were detected, with no cases of multi-drug resistance. In patients with poor adherence, directly observed therapy was opted for as an improvement strategy (five cases). In our series (as in the above-mentioned guidelines), few adverse reactions were reported, most of them mild and transient, only on occasion requiring discontinuation of the medication or dose reduction.
Most of the patients were followed up for six months, either at the hospital or at an outpatient centre. In a quarter of the patients, we were unable to confirm whether or not they had completed the full course of treatment, either because they were lost to follow-up or they did not complete the treatment during the prescribed time, and we could not therefore confirm whether or not they were cured.
Among the limitations of the study are its retrospective nature and the incorporation of diagnostic tests or slight changes in the therapeutic guidelines over time. However, the strengths are that it was a very big series (the second largest series in our setting) with a large sample size, reflecting the experience of two hospitals covering a very substantial population over 26 years.
In short, in terms of the clinical and epidemiological characteristics, our experience is in line with the literature on childhood TB: age distribution with predominance in infants and adolescents, and paucity and non-specificity of symptoms in the paediatric age group. Our findings are also consistent from the point of view of the greater frequency of pulmonary disease compared to other extrapulmonary manifestations. Even so, we believe that in order to better understand the changes in the epidemiology and history of childhood TB, more collaborative studies are necessary, and we should highlight the recent creation and important development of the Spanish childhood tuberculosis network (pTBred), which is contributing to a better understanding of this disease in our paediatric population.24,25
FundingThis study has received no specific funding from public, private or non-profit organisations.
Conflicts of interestNone declared.
Please cite this article as: Berzosa Sánchez A, Illán Ramos M, Prados M, Calderón Gallego C, Francisco González L, Callejas Caballero I, et al. Enfermedad tuberculosa en población pediátrica en Madrid en los últimos 26 años. Enferme Infec Microbiol Clin. 2020;38:312–316.