Development of secondary haemophagocytic lymphohistiocytosis (sHLH) in the context of typhoid fever (TF) is a very rare but serious complication.
MethodsDescription of the first pediatric case of typhoid fever acquired in a non-endemic area complicated by sHLH. A systematic literature review of sHLH in the context of TF was performed with extraction of epidemiological, clinical and laboratory data.
ResultsThe literature search revealed 17 articles (22 patients). Fifteen patients were eligible for data analysis (53.4% children). All patients had fever and pancytopenia. Transaminases and LDH were frequently elevated (46.6%). Salmonella typhi was detected mainly by blood culture (64.3%). All the patients received antibiotics whereas immunomodulation (dexamethasone) was used in two cases.
ConclusionsA high suspicion index for this condition is needed even in non-endemic areas. The addition of immunmodulation to standard antimicrobial therapy should be considered in selected cases.
El síndrome hemofagocítico (HLH) secundario en el contexto de fiebre tifoidea es una complicación rara pero seria.
MétodosDescripción del primer caso pediátrico de fiebre tifoidea adquirida en área no endémica complicada con síndrome hemofagocítico y revisión sistemática de la literatura de casos de HLH secundarios a fiebre tifoidea. Descripción de datos epidemiológicos, clínicos y de laboratorio, diagnóstico y manejo.
ResultadosLa búsqueda bibliográfica reveló 17 artículos (22 pacientes). Quince pacientes eran elegibles para el análisis (53,4% niños). La fiebre y la pancitopenia estaban siempre presentes, y las transaminasas y la LDH estaban frecuentemente elevados (46,6%). La detección de S. typhi se realizó mediante hemocultivo, principalmente (64,3%). Todos los pacientes reportados recibieron antibióticos; la dexametasona fue usada como tratamiento inmunomodulador en 2 de los casos.
ConclusionesMantener alto el grado de sospecha de esta condición es necesario, incluso en áreas no endémicas, ya que el uso de tratamiento inmunomodulador junto al tratamiento antimicrobiano puede ser determinante para una evolución clínica favorable.
Typhoid fever (TF) is endemic in Asia and Africa1 but relatively rare in Europe (0.31:100,000), where cases are mainly related with traveling to low/middle-income countries.2 In 2016, 33 cases were reported in Spain.3 TF, caused by Salmonella enterica serotype typhi (S. typhi) and Salmonella paratyphi (S. paratyphi), includes classically fever, abdominal and neurological symptoms. Clinical courses can range from uncomplicated to serious manifestations with multiorganic involvement.4 Hemophagocytic lymphohistiocytosis (HLH) secondary to TF is a very rare but potentially fatal complication.5 To the best of our knowledge we describe the first pediatric case suffering from HLH secondary to (domestically acquired) TF in Europe. In addition, we provide a systematic literature review.
For the preparation and publication of this manuscript informed consent was obtained from the family.
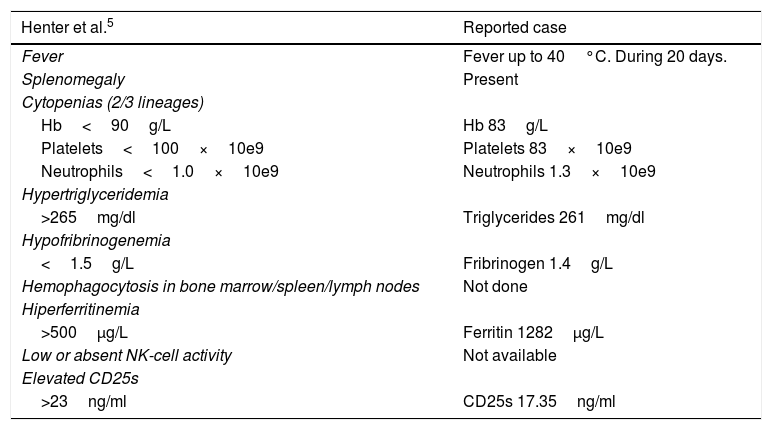
Case reportA previously healthy 7-years old boy was admitted to the local hospital with high-grade fever (40°C) and abdominal pain. There was no history of recent traveling, consumption of non-potable water or potentially contaminated food and there was no contact with a known typhoid case or carrier. He was transferred to our hospital 13 days after symptom-onset due to progressive clinical deterioration including persistent fever, vomiting, diarrhea and clinical suspicion of acute appendicitis. At admission he had diffuse abdominal pain and the physical examination revealed hepatosplenomegaly. Empiric antibiotic therapy with cefotaxime (150mg/kg/day) plus metronidazole (30mg/kg/day) was initiated. An abdominal CT-scan did not show signs for acute appendicitis or intra-abdominal abscess. 72h after admission, S. typhi was identified in blood and stool cultures. Subsequently metronidazole was discontinued and cefotaxime changed to ceftriaxone (80mg/kg/day). However, fever persisted and he developed progressive lethargy, ascites, and respiratory distress. Blood analyzes revealed pancytopenia, hyperferritinemia, hypertriglyceridemia, hypofibrinogenemia and raised sCD25 (17.35ng/ml, normal<7.5ng/ml; HLH criteria>23ng/ml) (Table 1). Laboratroy resources did not allow to testf for NK cell activity. Although bone marrow aspiration could not be performed, given the unstable clinical situation, the patient fulfilled 5/8 HLH criteria. Methylprednisolone (2mg/kg) was started; resulting in clinical improvement and apyrexia within 48h. Methylprednisolone was maintained for seven days and subsequently tapered over 14 days. Ceftriaxone was continued for a total of 14 days resulting in complete clinical and analytical recovery.
Analytic values.
| Henter et al.5 | Reported case |
|---|---|
| Fever | Fever up to 40°C. During 20 days. |
| Splenomegaly | Present |
| Cytopenias (2/3 lineages) | |
| Hb<90g/L | Hb 83g/L |
| Platelets<100×10e9 | Platelets 83×10e9 |
| Neutrophils<1.0×10e9 | Neutrophils 1.3×10e9 |
| Hypertriglyceridemia | |
| >265mg/dl | Triglycerides 261mg/dl |
| Hypofribrinogenemia | |
| <1.5g/L | Fribrinogen 1.4g/L |
| Hemophagocytosis in bone marrow/spleen/lymph nodes | Not done |
| Hiperferritinemia | |
| >500μg/L | Ferritin 1282μg/L |
| Low or absent NK-cell activity | Not available |
| Elevated CD25s | |
| >23ng/ml | CD25s 17.35ng/ml |
EIMC-D-18-00035 – REVISADO.
In order to systematically review the experience with HLH cases secondary to TF a structured literature search was performed.
MethodsFor the systematic database search, the terms “(Salmonella typhi or Salmonella paratyphi or typhoid fever or enteric fever) AND (hemophagocytic lymphohistiocytosis or hemophagocytic syndrome or hemophagocytosis)” were introduced in the Medline Database. All articles published in English or Spanish language including at least an abstract were reviewed. In addition, one French article was selected as it describes the only European case report. For specific data analysis three review articles (seven patients) were excluded given the lack of detailed case descriptions.
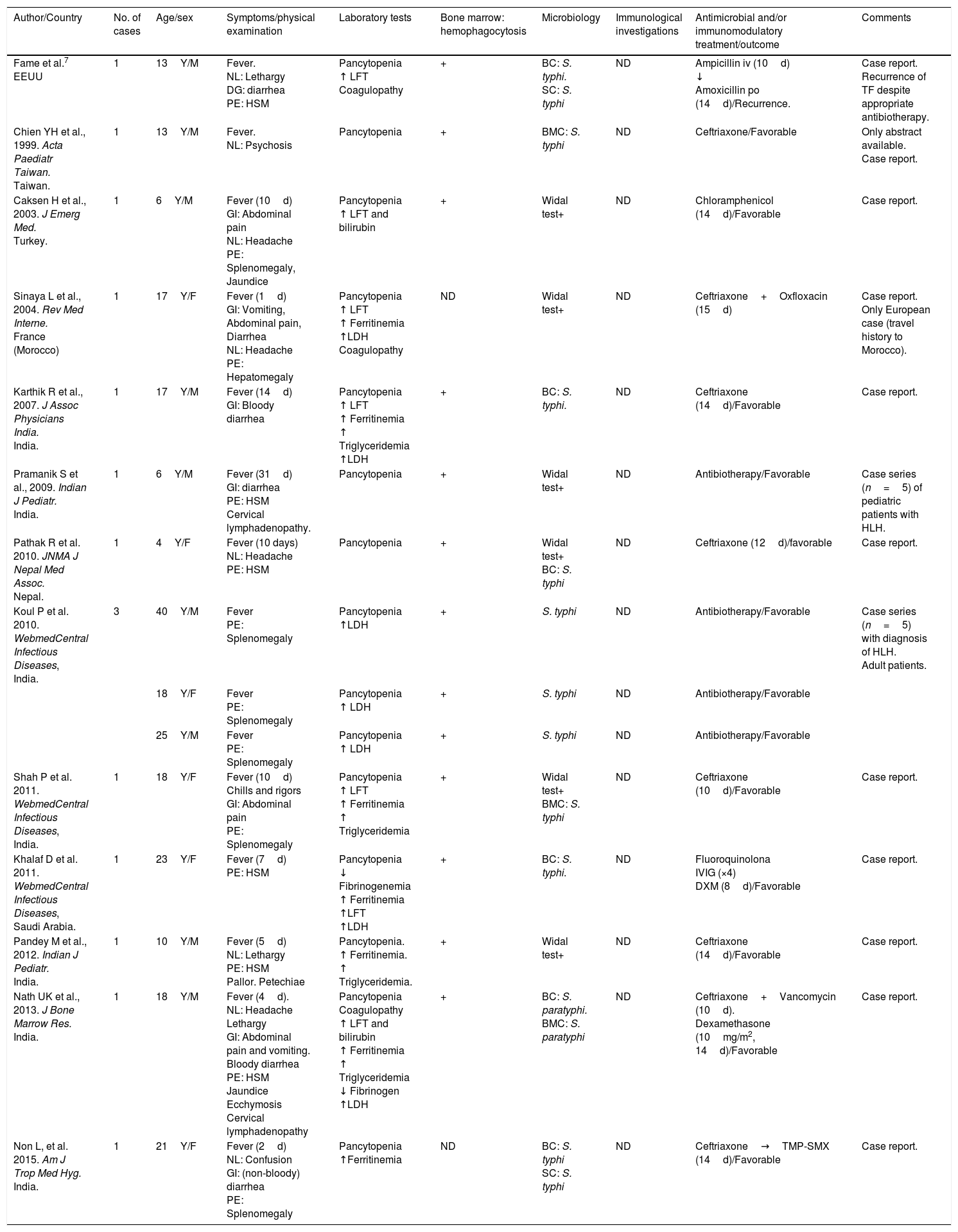
ResultsThe literature search revealed 17 articles, with a total of 22 patients (one review article6 contained 3 previously reported cases).
Only one of the reported cases was from Europe (imported from Morocco) and another one from the USA, whilst all the remaining cases were documented in Asia (n=20).
A total of 15 patients were eligible for data analysis (Table 2). Of these, nine (60%) were males. Eight patients (53.4%) were children or adolescent (<18 years old). Medium age for pediatric patients was 10.75 years (range: 4–17) and 23.3 years old (range: 18–40) for adult patients. Clinical data was available for 15 cases. Fever was the most common manifestation (100%); all except 2 patients had fever for more than 4 days, with a median duration of 8.5 days (range: 1–31). 53.3% of patients suffered from neurologic (headache, confusion/lethargy) or gastrointestinal (bloody diarrhea and abdominal pain) symptoms. Splenomegaly was common and accompanied by hepatomegaly in 46.6% of patients. Less frequent findings included jaundice, cervical lymphadenopathy and petechias/ecchymosis (each representing 13% of cases).
HLH secondary to TF: literature review.
| Author/Country | No. of cases | Age/sex | Symptoms/physical examination | Laboratory tests | Bone marrow: hemophagocytosis | Microbiology | Immunological investigations | Antimicrobial and/or immunomodulatory treatment/outcome | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Fame et al.7 EEUU | 1 | 13Y/M | Fever. NL: Lethargy DG: diarrhea PE: HSM | Pancytopenia ↑ LFT Coagulopathy | + | BC: S. typhi. SC: S. typhi | ND | Ampicillin iv (10d) ↓ Amoxicillin po (14d)/Recurrence. | Case report. Recurrence of TF despite appropriate antibiotherapy. |
| Chien YH et al., 1999. Acta Paediatr Taiwan. Taiwan. | 1 | 13Y/M | Fever. NL: Psychosis | Pancytopenia | + | BMC: S. typhi | ND | Ceftriaxone/Favorable | Only abstract available. Case report. |
| Caksen H et al., 2003. J Emerg Med. Turkey. | 1 | 6Y/M | Fever (10d) GI: Abdominal pain NL: Headache PE: Splenomegaly, Jaundice | Pancytopenia ↑ LFT and bilirubin | + | Widal test+ | ND | Chloramphenicol (14d)/Favorable | Case report. |
| Sinaya L et al., 2004. Rev Med Interne. France (Morocco) | 1 | 17Y/F | Fever (1d) GI: Vomiting, Abdominal pain, Diarrhea NL: Headache PE: Hepatomegaly | Pancytopenia ↑ LFT ↑ Ferritinemia ↑LDH Coagulopathy | ND | Widal test+ | ND | Ceftriaxone+Oxfloxacin (15d) | Case report. Only European case (travel history to Morocco). |
| Karthik R et al., 2007. J Assoc Physicians India. India. | 1 | 17Y/M | Fever (14d) GI: Bloody diarrhea | Pancytopenia ↑ LFT ↑ Ferritinemia ↑ Triglyceridemia ↑LDH | + | BC: S. typhi. | ND | Ceftriaxone (14d)/Favorable | Case report. |
| Pramanik S et al., 2009. Indian J Pediatr. India. | 1 | 6Y/M | Fever (31d) GI: diarrhea PE: HSM Cervical lymphadenopathy. | Pancytopenia | + | Widal test+ | ND | Antibiotherapy/Favorable | Case series (n=5) of pediatric patients with HLH. |
| Pathak R et al. 2010. JNMA J Nepal Med Assoc. Nepal. | 1 | 4Y/F | Fever (10 days) NL: Headache PE: HSM | Pancytopenia | + | Widal test+ BC: S. typhi | ND | Ceftriaxone (12d)/favorable | Case report. |
| Koul P et al. 2010. WebmedCentral Infectious Diseases, India. | 3 | 40Y/M | Fever PE: Splenomegaly | Pancytopenia ↑LDH | + | S. typhi | ND | Antibiotherapy/Favorable | Case series (n=5) with diagnosis of HLH. Adult patients. |
| 18Y/F | Fever PE: Splenomegaly | Pancytopenia ↑ LDH | + | S. typhi | ND | Antibiotherapy/Favorable | |||
| 25Y/M | Fever PE: Splenomegaly | Pancytopenia ↑ LDH | + | S. typhi | ND | Antibiotherapy/Favorable | |||
| Shah P et al. 2011. WebmedCentral Infectious Diseases, India. | 1 | 18Y/F | Fever (10d) Chills and rigors GI: Abdominal pain PE: Splenomegaly | Pancytopenia ↑ LFT ↑ Ferritinemia ↑ Triglyceridemia | + | Widal test+ BMC: S. typhi | ND | Ceftriaxone (10d)/Favorable | Case report. |
| Khalaf D et al. 2011. WebmedCentral Infectious Diseases, Saudi Arabia. | 1 | 23Y/F | Fever (7d) PE: HSM | Pancytopenia ↓ Fibrinogenemia ↑ Ferritinemia ↑LFT ↑LDH | + | BC: S. typhi. | ND | Fluoroquinolona IVIG (×4) DXM (8d)/Favorable | Case report. |
| Pandey M et al., 2012. Indian J Pediatr. India. | 1 | 10Y/M | Fever (5d) NL: Lethargy PE: HSM Pallor. Petechiae | Pancytopenia. ↑ Ferritinemia. ↑ Triglyceridemia. | + | Widal test+ | ND | Ceftriaxone (14d)/Favorable | Case report. |
| Nath UK et al., 2013. J Bone Marrow Res. India. | 1 | 18Y/M | Fever (4d). NL: Headache Lethargy GI: Abdominal pain and vomiting. Bloody diarrhea PE: HSM Jaundice Ecchymosis Cervical lymphadenopathy | Pancytopenia Coagulopathy ↑ LFT and bilirubin ↑ Ferritinemia ↑ Triglyceridemia ↓ Fibrinogen ↑LDH | + | BC: S. paratyphi. BMC: S. paratyphi | ND | Ceftriaxone+Vancomycin (10d). Dexamethasone (10mg/m2, 14d)/Favorable | Case report. |
| Non L, et al. 2015. Am J Trop Med Hyg. India. | 1 | 21Y/F | Fever (2d) NL: Confusion GI: (non-bloody) diarrhea PE: Splenomegaly | Pancytopenia ↑Ferritinemia | ND | BC: S. typhi SC: S. typhi | ND | Ceftriaxone→TMP-SMX (14d)/Favorable | Case report. |
BC, blood culture; BMC, bone marrow culture; d, day; F, female; GI, gastrointestinal manifestations; HLH, hemophagocytic lymphohistiocytosis; HSM, hepatosplenomegaly; IVIG, intravenous immunoglobulin; LFT, liver function test, M, male; ND, not done; NL, neurologic manifestations; PE, physical examination; SC, Stool culture; TF, typhoid fever; TMP-SMX, trimethoprim/sulfamethoxazole; UK, unknown; Y, years.
Laboratory tests included in the HLH criteria were commonly found positive. Pancytopenia was described in all cases, hyperferritinemia in 46.6%, hypertriglyceridemia in 26.6% and hypofibrinogenemia in 13.3%. Hemophagocytosis was present in 100% of the performed bone marrow studies (n=13). Other frequent analytical findings were hypertransaminasemia and elevated LDH (46.6% each). No immunological studies were described as part of diagnostic work-up in any of the patients. Microbiological diagnosis was mainly done by culture (11/14) of one (73%) or two (28.6%) biological samples; 4 patients (26.6%) were diagnosed using serological methods (Widal test). S. typhi was the most common isolate, with only one culture reported positive for S. paratyphi. Blood cultures were positive in 64.3% of the reviewed patients whereas bone marrow and stool cultures were found to be positive in 28.6% and 14.3%, respectively.
Management of HLH secondary to infectious agents is primarily based on directed antimicrobial therapy. In non-responsive cases concomitant immunomodulatory treatment may be considered.5 All reported patients (15/15) received antibiotics (mostly ceftriaxone) with a medium duration of 14 days (range 10–24). In addition, dexamethasone was used successfully in two patients as immunomodulatory treatment. One of these two patients received also intravenous immunoglobulin. Recurrence of TF was reported in only one of the 15 patients.7 This patient received antibiotic therapy without immunomodulation. Overall, all patients showed a favorable outcome with complete clinical recovery.
DiscussionTyphoid fever is uncommon in developed countries,1 but should be included as differential diagnosis in a patient with fever, abdominal symptoms and recent history of traveling to low/middle-income countries (Asia, Africa).1 All except one7 of the reviewed cases were from countries where TF is endemic (Table 2). Our patient is a child from Spain, a non-endemic country for TF, and neither he nor his family had any history of risk factors favoring S. typhi or S. paratyphi infection.
Overall TF is more frequently reported in children.8 However, in our literature review of TF related to HLH cases we found the same number of cases in the pediatric and the adult age group. Whereas familiar/primary HLH (fHLH) (genetic cause),5,9 is usually related with presentations in infancy or early childhood, secondary HLH (sHLH), an immune dysregulation disorder triggered by concurrent infections or other underlying medical conditions, is typically diagnosed in older children and adults, which might in part explain the age distribution found in our literature review. A broad range of infectious and non-infectious triggers can lead to sHLH,9 viral infections being the most common described etiology. To our knowledge, we provide here the most extensive summary of the available published data on sHLH in the context of TF (n=14+1).
Classically, TF has been described to have 3 illness stages. The third stage is characterized by persistent fever, hepatic involvement and anemia±leukopenia. These features are also often found in HLH patients5 converting the differential diagnosis between these two entities in a diagnostic challenge. A theoretical explanation for these similar clinical presentations may be that Salmonella enterica, the causative agent of TF, is an intracellular pathogen, which uses macrophages for its replication. TF infected macrophages persist in lymph nodes, spleen, liver and bone marrow and can initiate cytokine cascades that result in macrophage activation and subsequently lead to hemophagocytosis.10 Moreover, Salmonella infections have been used to create animal models of hemophagocytosis.10 In this context, bone marrow study and microbiological workup are critical for a correct diagnosis. In all previously reported patients, hemophagocytosis was seen when bone marrow studies were performed. In our patient, the impaired clinical status did not allow performing this procedure, thus HLH diagnosis was established based on the presence of 5/8 HLH criteria (pancytopenia, fever, hepatosplenomegaly, hypofibrinogenemia and hyperferritinemia).
Microbiological diagnosis using blood (40–80%) and stool cultures (37%) are less sensitive than bone marrow (90%) cultures,11 however in the reviewed cases TF diagnosis was mainly established by blood cultures (68%), whereas bone marrow cultures were positive in only 28% of cases. Sensitivity for the different specimens could not be estimated, as negative cultures were not specified for all patients. Severe TF has been described in the context of immunodeficiencies (e.g. HIV, IL-12 receptor deficiencies).12 In the previously published cases a detailed immunologic work-up was not reported. In our patient, the immunologic testing revealed normal results including lymphocyte subsets, immunoglobulin's levels and perforin expression.
The correct management of HLH patients is challenging due to the heterogeneity of the underlying diseases, genetic defects and patient conditions. The differentiation between fHLH and sHLH can be difficult as patients with fHLH often present with an underlying infection. All patients with symptoms suggestive for HLH require a prompt evaluation, ideally by an infectious disease and immunology specialist. Whilst severe, early-onset HLH (mostly fHLH) cases require aggressive immunosuppressive therapy, sHLH cases related to bacterial and parasitic infections would benefit from targeted anti-infectious treatment.5 In selected cases (severe affected or non-responding patients) the additional use of immunomodulatory agents should be considered.5 In our patient, with sHLH due to TF, the addition of methylprednisolone to the antimicrobial therapy resulted in rapid clinical improvement and was followed by a complete and uneventful recovery.
ConclusionTF is uncommon in Europe, but must be ruled out in patients with suggestive symptoms and a recent travel history to endemic areas, although as described here, the later does not exclude TF. sHLH due to TF is a very rare complication but should be considered in patients with an inadequate clinical response to appropriate antimicrobial therapy and these may benefit from adjuvant immunomodulatory therapy.
Ethical adherenceThe study was performed according to the ethical standards of the Helsinki-Declaration, local institution standards and after reception of written informed consent by the parents.
Conflict of interestOn behalf of all authors, the corresponding author states that there is no conflict of interest.