The need for specific antibiotic stewardship programs (ASP) in children is increasingly acknowledged.1 Neonates are a high-interest target population because of their unique characteristics and the widespread use of antibiotics in neonatal ICUs. Therapeutic drug monitoring (TDM), a key element of ASP, aims to achieve highest effectiveness with lowest risk of adverse events by maintaining plasma drug levels within a safe therapeutic range. The rapid physiologic changes as newborns mature, coexisting clinical factors, and diverse dosing regimens have led to recommendations for aminoglycoside and vancomycin TDM in this population.2 Our paediatric ASP (PROA-NEN), formally established in 2015, includes a specific neonatal approach. This study aimed to analyze the results of amikacin and vancomycin TDM in neonates, relationships between TDM and clinical outcomes, and our physicians’ adherence to local TDM guidelines.
We performed a prospective, observational study conducted in a tertiary-care neonatal ICU, including all consecutive episodes of vancomycin and/or amikacin treatment in newborns (June 2017–May 2019), excluding those lasting <48h. Amikacin and vancomycin dosing was based on Neofax criteria (Reuters T, Montvale, USA, 2011). The current local guidelines recommend TDM in treatments lasting >3 days, and every 3 days thereafter (or 24h after if dose is changed). Plasma amikacin was determined 8–12h post-dose, and vancomycin pre-dose (plus 3h post-dose in severe infection or central nervous system involvement). The therapeutic ranges were: amikacin, 1–8μg/mL; vancomycin trough level, 5–15μg/mL and peak 18–30μg/mL.3,4 Adherence to TDM guidelines was evaluated for each treatment episode and considered appropriate if at least 1 antibiotic with duration >3 days had 1 or more determinations. Statistical analyses used SAS v9.4 (SAS Institute Inc., Cary, NC, USA). The study was approved by the local ethics committee for clinical research (EPA(AG)28/2017(5085)).
The study included 146 newborns: 78 (53%) males, 107 (73%) preterm, 72 (49%) with underlying diseases. There were 259 infectious episodes; neonatal late-onset sepsis was the main suspected condition (207, 80%). Infection-attributed mortality was 2.5%; renal impairment and hearing disabilities at discharge were 0.5% and 11%, respectively.
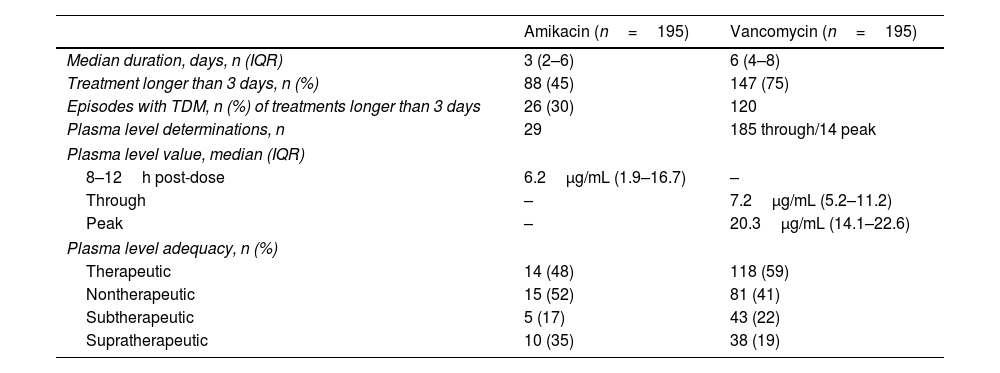
In total, 390 antibiotic courses were administered (64 amikacin alone, 64 vancomycin, 131 amikacin plus vancomycin). In total, 228 plasma determinations were performed: 132 (58%) within the therapeutic range. Non-therapeutic values led to dose changes in 93/96 cases (97%). Overall adherence to TDM guidelines was 63%: 82% for vancomycin and 30% amikacin (p<0.001) (Table 1). Confirmed infection (OR 2.29 [CI 1.03–5.13]; p<0.04) was the only factor related to greater TDM requests. No significant relationships were found between TDM request and infection-related mortality, clinical resolution, renal impairment, or hearing disabilities at discharge.
Antimicrobial characteristics and TDM results.
| Amikacin (n=195) | Vancomycin (n=195) | |
|---|---|---|
| Median duration, days, n (IQR) | 3 (2–6) | 6 (4–8) |
| Treatment longer than 3 days, n (%) | 88 (45) | 147 (75) |
| Episodes with TDM, n (%) of treatments longer than 3 days | 26 (30) | 120 |
| Plasma level determinations, n | 29 | 185 through/14 peak |
| Plasma level value, median (IQR) | ||
| 8–12h post-dose | 6.2μg/mL (1.9–16.7) | – |
| Through | – | 7.2μg/mL (5.2–11.2) |
| Peak | – | 20.3μg/mL (14.1–22.6) |
| Plasma level adequacy, n (%) | ||
| Therapeutic | 14 (48) | 118 (59) |
| Nontherapeutic | 15 (52) | 81 (41) |
| Subtherapeutic | 5 (17) | 43 (22) |
| Supratherapeutic | 10 (35) | 38 (19) |
n, number; %, percentage; IQR, interquartile range; TDM, therapeutic drug monitoring.
Therapeutic drug monitoring identified non-therapeutic antibiotic levels in 42% of determinations. Previous studies have also described significant rates of non-therapeutic levels,5,6 although dosing schemes and TDM procedures differed from those used here. In preterm newborns, an improvement in amikacin TDM has been reported after implementing more complex dosing schemes.7
Regarding vancomycin TDM, a recent model-based study used AUC/MIC ≥400 as the primary pharmacokinetic target (instead of through levels, a surrogate marker), showed the need for higher vancomycin doses.8 A multicenter clinical trial, NeoVanc (NCT02790996), is ongoing to validate new dosing regimens.
Data is scarce on adherence of prescribing physicians to paediatric TDM protocols. Some studies describe better monitoring after establishing specific guidelines, but precise data on compliance are not provided.5,6 Pain and anemia associated with extractions are reported as barriers for TDM in newborns.9 Although TDM enabled dose correction in many cases, a benefit on clinical outcome was not found here, likely due to the relatively low adherence to TDM guidelines and small percentage of confirmed infections. In contrast to what is reported in adults, no paediatric or neonatal studies to date have been able to demonstrate the impact of TDM on mortality or toxicity; nonetheless, expert neonatologists recommend TDM despite this lack of supporting data.2,3 The main limitations of this study are its single-center, observational design and use of TDM procedures different from those of other studies.
To conclude, our paediatric ASP team should implement targeted actions to improve TDM requests and monitoring procedures. As a final remark, new TDM tools are emerging, such as AUC-based models for vancomycin and model-informed precision dosing (MIPD) systems, which include patient and disease information. These may be superior approaches in this scenario.10
FundingThe present work received a pre-doctoral grant by Amics de la Vall d’Hebron (Institut de Recerca de la Vall d’Hebron).
Competing interestsThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
We thank Celine Cavallo for English language support.