The development and research of new technologies for identifying microorganisms, has allowed the identification of hitherto unknown bacteria. Auritidibacter ignavus is a newly described Gram-positive rod possibly associated with otitis, although its role as an etiologic agent in otitis is currently controversial.
MethodsWe report two cases of recurrent otitis in paediatric patients in which A. ignavus was isolated and review the previous cases reported in the literature.
ResultsAll the isolates were identified as A. ignavus by proteomic and genomic methods. Both patients recovered from their symptoms.
ConclusionA. ignavus was recovered from ear discharges of paedriatic patients with chronic ear problems. All the cases previously reported in the literature were adults. More evidence is needed for the association between A. ignavus and otitis, since data regarding this species are still scarce.
El desarrollo e investigación de nuevas tecnologías para la identificación de microorganismos, ha permitido la identificación de microorganismos hasta ahora desconocidos. Auritidibacter ignavus es un bacilo Gram-positivo recientemente descrito, posiblemente asociado con otitis, aunque su papel como patógeno ótico actualmente es controvertido.
MétodosPresentamos dos casos de otitis recurrente en pacientes pediátricos en los que se aisló A. ignavus y revisamos los casos previos descritos en la literatura.
ResultadosTodos los aislamientos fueron identificados como A. ignavus por métodos proteómicos y genómicos En ambos pacientes se resolvieron los síntomas clínicos.
ConclusiónA. ignavus se recuperó de las secreciones del oído de pacientes pediátricos con problemas crónicos del oído. Todos los casos descritos previamente en la literatura eran adultos. Es necesaria más evidencia para asociar a A. ignavus con la patología ótica, ya que los datos sobre esta especie aún son escasos.
Auritidibacter ignavus was first described in 20111 in a case of fulminant otitis externa in a 28-year-old male, where a facultative anaerobic gram-positive bacillus was isolated from an ear discharge sample. A new genus with a single species was created within the family Micrococcaceae, order Micrococcales, class Actinomycetes.
We present two cases of recurrent otitis in children in which A. ignavus was isolated and review the available literature on this microorganism (accessed 07/04/2022).
Case 1A 7-year-old male patient from Morocco who, since his arrival in Spain 10 months earlier, had suffered from at least four episodes of otorrhoea in both ears.
He was taken to the Accident and Emergency department (A&E) with purulent otorrhoea. He was assessed by Paediatrics and Ear Nose and Throat (ENT) and diagnosed with acute otitis media (AOM) with oedematous ear canal and otorrhoea, which was aspirated, and the patient was discharged with empirical treatment: oral amoxicillin 450 mg/every 8 h and ciprofloxacin otic 1 mg/every 12 h/for seven days. No samples were taken for culture, so the aetiology of this episode is unknown. ENT examination revealed mild/moderate asymmetric bilateral sensorineural hearing loss without any other clinical symptoms suggestive of ear infection.
One month later, he returned to A&E with an episode of otorrhagia and otalgia, with perforation of the anterior-superior quadrant of the tympanic membrane. With the final diagnosis of perforated AOM, he was discharged on empirical treatment with oral amoxicillin/clavulanic acid 350 mg/43.75 mg/every 8 h for 10 days, without any further recommendation and/or treatment. In this episode, a sample of ear discharge was collected for culture. ENT follow-up found the patient to have normal hearing bilaterally and to be asymptomatic, with closure of the tympanic perforation.
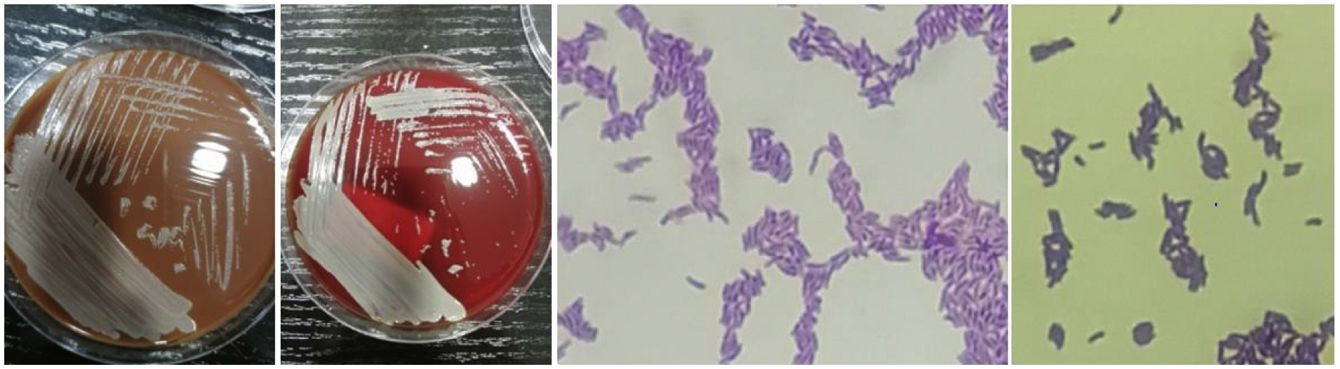
The ear discharge was cultured on chocolate agar and CHROMID®CPS®/Columbia CNA agar bi-plate with 5% sheep blood (bioMerieux, Marcy l'Etoile, France). The plates were incubated for 48 h at 37 °C in a 5% CO2 atmosphere. Gram staining of the sample showed mixed microbiota with a clear predominance of gram-positive bacilli. The culture showed mostly small, smooth, creamy-looking colonies growing on both plates together with sparse commensal skin microbiota.
Gram staining of the colony showed Gram-positive bacilli in a palisade arrangement (Fig. 1). Identification was carried out by mass spectrometry (MALDI Biotyper®, Bruker Daltroniks, Billerica, USA), resulting in the species A. ignavus, with a score of 2.140 (MSP library version BADAL11, which contains only two entries of A. ignavus). Identification was subsequently confirmed by amplification and sequencing of the 16S ribosomal small subunit coding gene according to the protocol published by Xu et al.4 with sequence analysis by BLAST, resulting in 99% similarity. The sequences obtained were not submitted to GenBank.
The antibiotic sensitivity study of the microorganism was performed by the broth microdilution method using the MICroSTREP plus 3 panel (MicroScan®, Beckman Coulter, Brea, USA). The MIC results (mg/l) obtained were: ampicillin/amoxicillin (0.25); amoxicillin-clavulanic acid (<0.25/0.12); penicillin (0.25); cefaclor (<1); cefuroxime (≤0.25); cefotaxime (0.5); cefepime (2); meropenem (1); ciprofloxacin (0.5); trimethoprim/sulfamethoxazole (<0.25/4.7); rifampicin (≤0.5); tetracycline (≤1); chloramphenicol (≤1); erythromycin (≤0.25); azithromycin (≤0.25); clindamycin (≤0.25); and vancomycin (≤0.5). Interpreting these values according to the 2022 EUCAST cut-off points for Corynebacterium spp.,5 the isolate was reported as sensitive to ciprofloxacin, rifampicin, clindamycin and vancomycin and resistant to penicillin and tetracyclines.
Case 2This was a 10-year-old female patient with recurrent otitis (at least five episodes in the last year), under follow-up by ENT since 2016 for hearing loss and recurrent otitis.
In the microbiology department, we received a sample of ear discharge from primary care for AOM after consultation for otalgia and a positive swallowing sign.
Sample processing was carried out as described above. Gram-positive bacilli were observed in the Gram stain and the same type of colonies were isolated and identified (MALDI-Biotyper®) as A. ignavus, with a score of 1980. Identification was confirmed by PCR and 16S rRNA gene sequencing. In addition to this species, commensal microbiota from the skin were also isolated.
The sensitivity study was performed as above; with the following results: ampicillin/amoxicillin (0.25); amoxicillin–clavulanic acid (0.5/0.25); penicillin (0.5); cefaclor (2); cefuroxime (0.5); cefotaxime (0.5); cefepime (>2); meropenem (1); ciprofloxacin (>2); trimethoprim/sulfamethoxazole (2/38); rifampicin (≤0.5); tetracycline (≤1); chloramphenicol (2); erythromycin (2); azithromycin (2); clindamycin (0.5); and vancomycin (≤0.5). The isolate was reported as resistant to penicillin and ciprofloxacin, and sensitive to rifampicin, clindamycin, vancomycin and tetracyclines.
The patient was prescribed empirical ciprofloxacin otic 0.6 mg/every 8 h for 10 days, without any further recommendation and/or treatment. She completed the treatment, her symptoms of infection resolved clinically and otoscopy was normal. After 10 days, a second sample (requested by Microbiology for aetiological confirmation) was received in which A. ignavus was still isolated, along with skin microbiota.
DiscussionThe species A. ignavus has only recently been described and there are only a few published cases, so far associated with ear infections.1–3
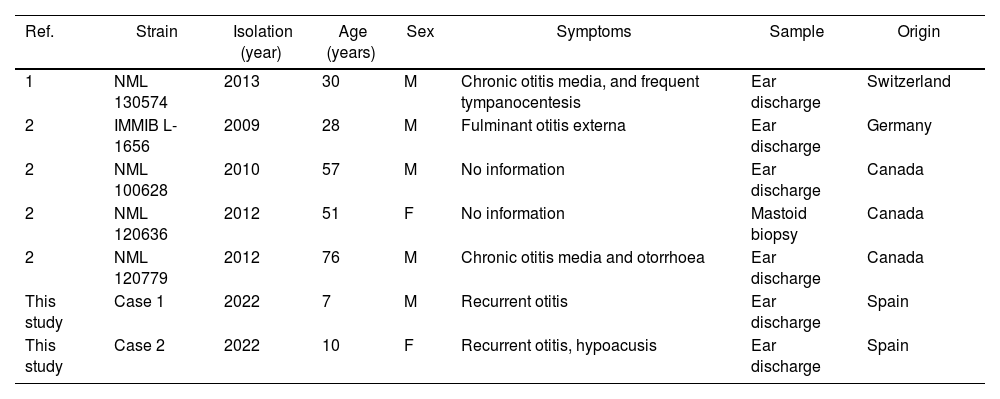
Yassin et al.1 described the first isolate in 2011, while proposing the new genus and species. Bernard et al.2 in 2020 added the description of four more cases and reviewed the characteristics of the species. Table 1 shows the clinical and demographic characteristics of these cases and the two we present here.
Clinical characteristics of patients in whom A. ignavus was isolated.
| Ref. | Strain | Isolation (year) | Age (years) | Sex | Symptoms | Sample | Origin |
|---|---|---|---|---|---|---|---|
| 1 | NML 130574 | 2013 | 30 | M | Chronic otitis media, and frequent tympanocentesis | Ear discharge | Switzerland |
| 2 | IMMIB L-1656 | 2009 | 28 | M | Fulminant otitis externa | Ear discharge | Germany |
| 2 | NML 100628 | 2010 | 57 | M | No information | Ear discharge | Canada |
| 2 | NML 120636 | 2012 | 51 | F | No information | Mastoid biopsy | Canada |
| 2 | NML 120779 | 2012 | 76 | M | Chronic otitis media and otorrhoea | Ear discharge | Canada |
| This study | Case 1 | 2022 | 7 | M | Recurrent otitis | Ear discharge | Spain |
| This study | Case 2 | 2022 | 10 | F | Recurrent otitis, hypoacusis | Ear discharge | Spain |
M: male; F: female.
The isolate published by Yassin et al.1 was sensitive to all antibiotics tested by disc/diffusion (µg per disc): penicillin (10); ampicillin (10); cefazolin (30); oxacillin (5); vancomycin (30); and clindamycin (2). The isolates described by Bernard et al.2 were tested by broth microdilution and were sensitive to penicillin, cefepime (one resistant strain), cefotaxime, ceftriaxone, meropenem, vancomycin, daptomycin, gentamicin (two resistant strains), erythromycin (three resistant strains), tetracycline, trimethoprim-sulfamethoxazole, rifampicin and linezolid, and all were resistant to ciprofloxacin and clindamycin applying the CLSI6 cut-off points for Corynebacterium spp. and related genera.
Comparing the antibiotic sensitivity of published cases and our strains, there does not seem to be a clear pattern of antibiotic sensitivity in this species, although all strains appear to be sensitive to vancomycin.
The strains in the two cases we present here would be considered intermediate susceptible (CLSI) or resistant (EUCAST) to penicillin, according to the criteria used. As there is no consensus, or specific cut-off points for this species, it is not possible to determine with certainty its classification as sensitive or resistant, or whether or not the antibiotic treatment received by the first patient (amoxicillin) was responsible for resolving the symptoms.
In the case of treatment of the second patient with ciprofloxacin, resistant using cut-off points for systemic treatments, it was applied topically, so the relationship between the MIC and the antibiotic concentration reached at the focus is probably different from that established in the criteria.
Further isolates need to be studied to determine specific cut-off points for this species and to correlate in vitro MIC with in vivo antibiotic treatments.
For identifying the isolates, as stated by Bernard et al., the addition of two entries in the MALDI-Biotyper® microorganism library which were previously non-existent enables unequivocal identification in any laboratory equipped with MALDI-TOF MS.2
The classifying of A. ignavus as an ear pathogen is subject to debate. Although the history of cases for this species is very limited, we believe the fact that all the isolates have been recovered from ear samples in patients with clinical infections means we can hypothesise the existence of such an association. In the two cases presented here, the isolation of A. ignavus was not accompanied by any other ear-infecting pathogen.
However, further evidence, a greater number of isolates and more studies in both otitis patients and healthy individuals are needed to clarify the pathogenic or commensal role of A. ignavus. Interestingly, the two cases we present here are paediatric patients, whereas all the isolates described previously were from adult patients. A subject of further investigation should therefore be whether there are differences in ear canal microbiota between children and adults.
FundingThis study received no specific funding from public, private or non-profit organisations.
Conflicts of interestThe authors have no conflicts of interest.
To Dr. Juan José Palacios Gutiérrez and Dr. Fernando Vázquez Valdés for their help in revising the article.